Physical therapy and rehabilitation
- What is it?
Treatments :
- Lumbar hernia
- Stroke rehabilitation
- Neck hernia
- Manual therapy
- Traumatic brain injury and rehabilitation
- Spinal cord injuries and rehabilitation
- Stroke rehabilitation
- Chiropractic treatment
- Low back pain
- Scoliosis
- Pediatric rehabilitation
- Ozone therapy
- Ergo therapy
- Facial paralysis
- Cerebral palsy
- Obesity rehabilitation
- Rehabilitation of muscle diseases
- Cardiac rehabilitation
- Joint calcification
- Fracture rehabilitation
- Acupuncture
- Pulmonary rehabilitation
- Hydrotherapy
- Spina bifida
- Nerve compression
- Osteopathy
- Neck pain
- Shoulder pain
- Neck flattening
- Cruciate ligament injuries
- Knee arthritis
- Restless leg syndrome
- Bursitis tendinitis
- Slipped back
- Clinical Pilates
- Dull shoulder
- Trigger point treatment
- Hip arthritis
- Achilles tendonitis
- Capral tunnel syndrome
- Shoulder muscle tears
- Shoulder impingement syndrome
- Multiple sclerosis (MS)
- Channel narrowing
- Bone marrow edema syndrome
- Fingertip deformation
- Halluks valgus
- Baker cyst
- Knee prosthesis rehabilitation
- Speech, tongue therapy
- Lymph edema treatment
- Cup treatment
- Torticollis
- Swallowing rehabilitation
- Dry needle therapy
- Brachial plexus rehabilitation
- Vertigo rehabilitation
- Mesotherapy
- Meniscus injuries
- Hip prosthesis rehabilitation
- Ankle sprains
- Tennis and golfer’s elbow treatment
- Inflammatory joint rheumatism
- Chronic fatigue
- Inflammatory low back pain
- Rheumatoid arthritis
- Fibromyalgia
- Heel spur
What is Physical Therapy and Rehabilitation?
Physical Therapy and Rehabilitation is a specialty that covers the diagnosis and treatment of physical and functional disorders in the musculoskeletal, nervous or cardiovascular systems.
Physical therapy means the use of physical methods and techniques in the treatment of diseases. The applied physical therapy methods and techniques do not cause any lesions or wounds in our body. The aim of physical therapy is to reduce or eliminate the patient’s pain, increase functional capacity, regain daily life activities, restore the functions of organs, and take their place in society as an independent individual.
In Which Areas Is Physical Therapy and Rehabilitation Used?
- Orthopedic Diseases and injuries
- Neurological and neuromuscular diseases and injuries
- Treatment of acute and chronic pain
- Rheumatic diseases
- Pediatric rehabilitation
- Cardiopulmonary rehabilitation (heart-lung rehabilitation)
- Congenital or acquired joint and bone disorders
- Rehabilitation after burns
- Geriatric (elderly) rehabilitation
- Metabolic diseases (diabetes, osteoporosis, etc.)
- Sports injuries
- Preventive treatment approaches
What are Physical Therapy and Rehabilitation Practices?
After the diagnosis of the disease, an appropriate physical therapy program is planned according to the patient’s condition. Physical therapy should be performed under the supervision of a specialist physician. This treatment program may include medication, application of physical therapy techniques and one or more therapeutic exercises.
Heat, light, water agents
Superficial heat (infrared, hot pack, paraffin, whirlpool bath),
Deep heat (ultrasound, high intensity laser, TECAR)
Hydrotherapy (in-pool exercise, contrast bath, spa treatment, underwater massage, whirlpool bath)
Electrotherapy
It is applied by applying current to the body at a certain frequency and intensity. It can be used for the treatment of acute or chronic pain, edema, muscle strengthening or functional training of certain muscles.
Mechanotherapy
It is the application of mechanical devices and apparatus for treatment purposes.
Walking robots, arm robots, traction, spinal decompression (waist-neck pulling), pneumatic compression, CPM devices etc. are used.
Manual Therapy Methods
Manual therapy is a form of physical therapy that is applied only by hand without the use of any devices or machines. In manual therapy, practitioners use only their hands to reduce problems caused by muscle spasm, muscle tension and joint dysfunction.
Therapeutic Exercises
It is one of the most important parts of physical therapy. Personalized exercises designed according to the patient and the condition of the disease should only be given by specialist physicians and physiotherapists.
Daily Life Modifications
During the treatment of the disease, the patient may make some adjustments in his/her daily life. Activity arrangements, adding exercise and sports to daily life, avoiding potentially harmful movements, dietary recommendations, etc. can be examples of this.
Use of prosthesis-orthotics
Prostheses Apparatus made to imitate the missing limb.
Orthotics: Apparatus used to protect, support and improve the performance of an existing limb (knee brace, corset, cane, bandage, tape, kinesiotape, etc.).
What is the Duration of Physical Therapy?
Physical therapy is done in sessions. In orthopedic diseases, a total of 10-20 sessions of 1 hour can be applied. In neurological diseases, rehabilitation is usually a longer process, it is applied in 1-2 hour sessions, but the rehabilitation process can last for years depending on the patient’s condition.
Are Physical Therapy Applications Painful?
The patient usually does not feel pain during physical therapy applications. However, if the patient has joint restriction, for example a frozen joint, there may be mild pain as the physiotherapist may perform stretching exercises.
What are the Conditions to Pay Attention to?
Inflammatory conditions, active periods of rheumatic diseases (periods when the joints are swollen, hot and painful), vascular occlusions, varicose veins, open wounds and infected areas are taken into consideration or applications that are not deemed appropriate by the specialist physician are not performed.
What are the Possible Risks and Side Effects of Physical Therapy and Rehabilitation Practices?
Physical therapy is a treatment approach with very few side effects and risks. However, undesirable effects such as skin rashes and sensitivity may occur, although rare.
Very rare side effects include skin hypersensitivity and blood pressure changes.
Risks are rarely seen in the presence of appropriate technique, adequate medical equipment and experienced medical personnel.
In order to minimize the incidence of these conditions, you should give detailed information to your doctor about your medical condition before the application. You should inform your doctor about any known drug allergies and diseases.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
What is Lumbar Hernia?
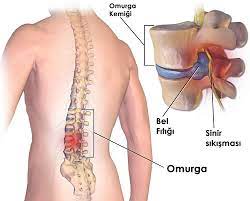
A herniated disc occurs when the discs between the 5 vertebrae that make up the lumbar spine wear out, tear or slip out of place due to various reasons, putting pressure on the spinal cord and the nerves leaving the spinal cord.
What are the Causes of Lumbar Hernia?
The fluid content in the discs between the vertebrae decreases with time and age. This reduces the durability of the disc against loads. Strains such as heavy lifting, uncontrolled sudden lumbar movements, prolonged standing or sitting, exposure to traumas such as falls and bumps can cause tears in the disc and cause a herniated disc.
Although herniated discs are more common in middle-aged and older people, they can also occur in young people and even in children. Although it occurs at the same rates in men and women, the risk of occurrence increases during pregnancy due to excessive weight gain in a short period of time. Being overweight is an important risk factor for herniated discs. In addition, smoking disrupts the nutrition of the discs, causing fluid loss and increasing the risk of herniated discs. It also prolongs the healing process. Other risk factors for herniated discs include working at a desk for long periods of time, driving for long periods of time, leading a sedentary life, engaging in movements and activities that strain the spine, and engaging in inappropriate sports activities.
Weak muscles around the spine and trunk-abdominal muscles increase the load on the discs and pave the way for herniation. Therefore, in order to prevent herniated discs, it is very important to do exercises and sports that strengthen the waist, abdomen and back muscles, as well as avoiding the above risk factors.
What are the Symptoms of Lumbar Hernia?
The most important symptom of a herniated disc is pain radiating from the waist to the leg. Patients usually consult a physician with this complaint. However, these symptoms may not be seen in every herniated disc patient. Sometimes it may be completely painless or only pain in the lumbar region may be observed at the beginning. The pain can usually radiate along the back of the leg to the hip, knee or even the heel. In situations that increase spinal cord pressure, such as coughing, sneezing and straining, the pain may intensify, and even stiffness may occur.
Pain in one or both legs may be accompanied by symptoms such as numbness, burning and tingling. The cause of these symptoms is the pressure of the hernia on the leg nerves. In cases of severe nerve compression, more advanced neurological problems such as weakness in the leg, ankle and foot muscles, difficulty walking, urinary incontinence and loss of sexual function may occur.
Due to pain, stiffness and functional inadequacy, the patient begins to experience difficulties in daily life activities such as sitting, standing and walking.
How is a herniated disc diagnosed?
Lumbar disc herniation is diagnosed with a careful patient history, physical and neurological examination, and imaging methods such as X-ray, MRI (magnetic resonance imaging) or CT (computed tomography). In some cases, nerve examinations called EMG (electromyography) may be needed.
What are the treatment methods for herniated discs?
Herniated disc treatment is applied individually. It is not a condition that requires urgent surgical treatment except for serious neurological symptoms such as progressive loss of strength, urinary and fecal incontinence. Generally, a very large proportion of patients can be treated without the need for surgical intervention.
The first step in the treatment of herniated disc is rest. However, since it has been understood in recent years that prolonged rest may have negative effects on the treatment of herniated discs, it is important to keep rest and restriction of movement as short as possible for the success of the treatment. Although short-term bed rest may be prescribed in cases of severe pain, resting is mostly in the form of restricting movements that put stress on the spine. Whether the patient can go to work or not is evaluated by his/her doctor depending on his/her job.
During this period, painkillers and muscle relaxants are usually administered. In some cases, steroid treatment can be administered in a controlled manner. Corsetry can be used for a short period of time when necessary.
Physical therapy methods have an important place in the treatment of herniated discs. For this purpose, hot applications, ultrasound, laser, pain relief current treatments, massage, mobilization, manual therapy, dry needling, taping, traction (classical and vertical traction-vertetrac) are the most commonly used treatment methods.
In some cases, epidural injections and nerve blocks can be performed in the lumbar region to relieve pain.
Exercise should be started early in the treatment of lumbar disc herniation and should be an integral part of the treatment. In the beginning, the patient is trained to regulate activities of daily living and a program that includes stretching, stretching and posture exercises that do not increase pain is initiated. As the pain decreases in the later stages of the process, endurance and strengthening exercises are started.
Spinal decompression therapy is a successful treatment method for herniated discs. It is a technology that applies controlled traction to create negative pressure on the problematic disc. It provides a safer and more effective traction than other traction methods and can be used in advanced herniated disc cases.
Surgery for herniated disc is the last treatment option used in cases with severe and progressive neurological deficits and in cases where no results are obtained despite all treatments. Physical therapy and rehabilitation can be performed in the postoperative period if needed.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is a stroke?
Paralysis is a condition involving a loss of muscle function that can be accompanied by a loss of sensation and is also called sensory loss. The term is derived from the Greek word meaning the neutralization of nerves. This is because there is often a loss of motor function or sensory information in the nervous system.
There are two main causes of paralysis. Paralysis is caused by damage to the brain or spinal cord. Paralysis, which is more common in older people, does not affect the whole body but only a certain part of it. The loss of sensation and movement in paralysis is usually unilateral and occurs only on the right or left side of the body.
What are the causes of paralysis?
There are several possible reasons why someone may have a temporary or permanent stroke. It is usually the result of damage to the spinal cord or other parts of the nervous system. These damages are
- Stroke
- Trauma
- Poliomyelitis
- Cerebral palsy
- Peripheral neuropathy
- Parkinson’s disease
- Botulism
- Spina bifida
- Multiple sclerosis
- Guillain Barre Syndrome
- In addition, some medicines affect the function of nerves and in rare cases can cause paralysis.
What are the types of paralysis?
Paralysis can be classified as localized, when a specific part of the body is affected, such as the face or hands, or generalized, when a large part of the body is affected. There are also more specific terms to describe the specific areas of the body affected:
- Monoplegia is paralysis of one limb.
- Hemiplegia is paralysis of an arm or leg on one side of the body.
- Paraplegia is paralysis of both legs and parts of the lower body, such as the pelvis.
- Tetraplegia or quadriplegia is paralysis of both arms or legs.
What are the conditions caused by paralysis?
Stroke can also cause other health problems. In particular, urinary incontinence and bowel incontinence are known to affect many people who have suffered a stroke. In addition, the sexual function of both men and women is negatively affected.
Pressure ulcers can also occur due to excessive pressure on certain tissues in the body.
Many people experience psychological effects as a result of the changes associated with paralysis. Depression is very common because individuals are no longer able to live the life they are used to and it can be difficult to adapt to this change.
How is paralysis treated?
The goal of stroke treatment is, in general, to live as independently as possible with the highest quality of life. The optimal treatment for each stroke patient depends on the type of stroke and its impact on quality of life.
Devices that assist people with disabilities can offer solutions for some types of paralysis. For example, paraplegics who lose the function of the lower part of the body can use a wheelchair and live a relatively independent lifestyle.
For people who are also paralyzed in the upper body, an electric wheelchair can help with mobility if they control the movement of their hands.
Orthotics are another alternative designed to improve limb function and compensate for weaknesses in the affected muscles.
Follow-up is very important in stroke complications. Being aware of possible complications so that signs can be diagnosed earlier in case they occur helps. Early diagnosis facilitates the patient’s treatment and improves quality of life. In addition, medical treatment of these conditions is justified and should be addressed to improve each patient’s quality of life.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
What is Neck Hernia?

Cervical herniated discs, which act as shock absorbers in the cervical vertebrae, compress the spinal cord and the nerves leaving the spinal cord due to wear, tear or displacement due to various reasons.
The human spine is a dynamic structure consisting of 33 vertebrae. The neck and waist region are the most mobile parts of the spine. The bone structures that make up the spine are the discs between the vertebrae and provide the connection between them. The discs act as shock absorbers for pressure and loads.
What are the Causes of Neck Hernia?
The fluid content in the discs between the vertebrae decreases over time and with age. Poor use of the spine also increases this decrease. As a result, the durability of the disc against loads decreases. Strains such as uncontrolled sudden movements, working at a desk for a long time and in a stationary position, doing jobs and sports that put a load on the spine or require continuous rotation movements, and being exposed to traumas such as falls from heights and traffic accidents can cause tears in the disc and cause a herniated disc in the neck.
Although cervical herniated discs are seen in all age groups, they are more common in the young-middle age group. It is known to be more common in people with thin, slender and long necks. In addition, smoking is a risk factor for cervical herniated discs, as it is for lumbar herniated discs. Other risk factors for cervical hernia include working at a desk for long periods of time, driving for long periods of time, leading a sedentary life, using inappropriate pillows during sleep, engaging in movements and activities that strain the spine and doing inappropriate sports activities. The weakness of the muscles around the neck also increases the load on the discs and prepares the ground for herniation.
What are the Symptoms of Cervical Hernia?
Lumbar and Cervical Hernia
The most common and earliest symptom of a cervical disc herniation is pain in the neck. Not all neck pain is due to a cervical hernia. Muscle-related pain is actually quite common in the neck region. Hernia-related pain, on the other hand, is both more resistant and shows some characteristics. The pain may radiate unilaterally from the neck to the arm, or it may radiate from the back or neck to the head. Although the pain is usually continuous, it tends to intensify with neck movements. In addition to pain, numbness, tingling, burning, pins and needles and electric shocks in the arms and hands may also be present. Neurological symptoms such as loss of sensation, decreased strength, decreased dexterity and thinning of the arm may also be observed. Coughing, sneezing and straining can increase the pain.
How is a cervical hernia diagnosed?
Cervical hernia is diagnosed with a careful patient history and physical and neurological examination. Imaging methods such as X-rays, MRI (magnetic resonance imaging) or CT (computed tomography) help to confirm the diagnosis and formulate a treatment plan. In some cases, nerve examinations called EMG (electromyography) may be needed.
Pain in the neck, back, shoulders and arms can also be caused by diseases other than cervical hernia. Sometimes pain reflected from internal organs can cause similar symptoms and signs. Therefore, before making a diagnosis of cervical hernia, it is necessary to exclude these conditions that may cause similar complaints. For this purpose, advanced imaging and laboratory examinations may be used if deemed necessary.
How is Cervical Hernia Treated?
A very large proportion of cervical hernia patients can be treated without the need for surgical intervention. In some mild cases, improvement in complaints can be achieved by resting, regulating daily life activities and educating the patient about the correct use of the neck. These patients should be directed to a regular exercise program and followed up.
Painkillers and muscle relaxants are frequently used for the treatment of cervical hernia. Drugs containing corticosteroids can be used under the supervision of a doctor if needed. In some cases, it may be necessary to temporarily use a neck collar.
Physical therapy methods are used in cervical herniated disc patients who do not get results with these treatments and measures or who present with severe nerve compression. For this purpose, hot applications, ultrasound, laser, painkillers and muscle strengthening current treatments, massage, mobilization, manual therapy, Hilterapy (high intensity laser therapy), dry needling, taping, traction (classical and vertical traction-vertetrac) are the most commonly used treatment methods.
As complementary and supportive treatment methods, acupuncture, neural therapy, cupping therapy and ozone therapy can also be used in the treatment of cervical disc herniation.
Spinal decompression therapy is an effective treatment method in the treatment of cervical herniated discs as in lumbar herniated discs. It is based on the application of controlled traction to create negative pressure at the level of the affected disc.
In some cases, epidural injections and nerve blocks can be performed in the neck area to relieve pain. Trigger point injections can also be applied to the muscles of the neck, back and shoulder region.
Exercise therapy should be an integral part of neck hernia treatment. First of all, the patient is trained on the correct use of the spine and daily life activities. Then an exercise program including stretching, stretching, strengthening and posture exercises is initiated. The intensity and duration of this program is determined according to the clinical condition of the patient.
Clinical pilates applications are a very useful treatment method in both treatment and prevention of cervical herniated discs as in other spinal problems.
Surgical treatment is rarely needed in the treatment of cervical hernia. Surgery is used as the last treatment option in patients who do not benefit from non-surgical treatments and who have severe and progressive neurological deficits.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Manual Therapy?

Manual therapy is a form of physical therapy that is applied only by hand without the use of any devices or machines. In manual therapy, practitioners use only their hands to manipulate the joints in the area and apply pressure on muscle tissue to reduce pain caused by muscle spasm, muscle tension and joint dysfunction.
Who Can Receive Manual Therapy?
Manual therapy can help in the treatment of people with joint disorders who do not have enough mobility and range of motion in some musculoskeletal structures. These disorders can cause pain and changes in function, posture and movement. Manual physical therapy is used to strengthen the mobility of joints and reduce muscle tension to allow the patient to move more naturally without pain. Manual therapy can provide relief in the treatment of joint problems such as sacroiliac joint dysfunction, chronic low back pain, acute back pain caused by soft tissue injuries, back muscle tension and ligament pulls. Following manual therapy, it is seen to be effective in the treatment of patients with chronic low back and back pain. Manual physical therapy techniques include various applications:
Pressure is applied to soft tissues and muscles, including massage. This pressure relaxes the muscles, increases circulation, helps break down damaged tissue and reduces pain in the soft tissues.
The mobilization/manipulation method, which involves movements at different speeds (from slow to fast), is used to bend, pull or push force (from light to strong) and stretch (called ‘amplitude’) bones and joints.
Things to Consider Before Manual Therapy
Before starting manual therapy or any physiotherapy, your therapist will carry out a detailed assessment to determine the muscle, bone and nerve damage of the area to be treated to avoid any risk. He or she will then prescribe a treatment that includes one or more of the types of physical therapy specific to the patient’s condition.
Soft Tissue Mobilization
It is applied to activate the joints and surrounding muscles. When joint movements improve, muscle tension decreases. Manual therapy is applied to relieve muscle tension and joint disorders. Soft tissue mobilization mobilizes tissue fluids to treat myofascial adhesions caused by various causes, resulting in reduced muscle tension. This procedure is applied to all the muscles surrounding the spine and consists of rhythmic stretching and strong pressure.
Stretch and Count
This technique focuses on correcting abnormal neuromuscular reflexes that cause structural and postural problems and is applied to the points that trigger pain. The therapist finds the patient’s most comfortable position by asking at which point the sensitivity is reduced. The patient is held in this comfortable position for approximately 90 seconds. During this time, asymptomatic tension occurs with mild stretching and is gradually removed from this position. The body muscles are then allowed to return to a normal level of tension. The natural tension in the muscles determines the stage of recovery. This technique is preferred for treating back problems that are too acute or too sensitive to be treated with other procedures.
Joint Mobilization
Patients often complain that a particular muscle in their back is stiff, and rest, ice and massage can help to reduce the pain. However, the back pain often recurs. Joint mobilization loosens the affected joints and increases the speed of movement.
What are the advantages of manual therapy?
The healing process in manual therapy is very fast. The treatment time is also very short compared to other techniques.
In manual therapy, very effective results can be obtained from the first session. While pain and tension decrease, the ability to move greatly increases.
The success rate of manual therapy is much higher than other techniques. Thanks to its high success rate, it is the most frequently requested physical therapy method.
In manual therapy, the damaged area is treated directly by hand. No tools and devices are used in any way.
One of the most important advantages of manual therapy is that it has no side effects.
For Which Diseases is Manual Therapy Suitable?
Manual therapy has been successfully applied for many years in the treatment of many diseases related to the muscular and joint system. Manual therapy especially:
- Lumbar hernia
- Slipped back
- Neck hernia
- Neck flattening
- Joint problems
- Muscle tear
- Dull shoulder
- Elbow and wrist disorders
- Hip dislocation
- Pain after hip replacement
- Heel spur
- It offers a very effective treatment for the treatment of problems such as foot disorders.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is traumatic brain injury?

Traumatic brain injury can occur due to a variety of causes, most commonly traffic accidents, falls from height, occupational accidents, assault, gunshot wounds. It is an important cause of disability in the society and its rehabilitation is very important. After early intensive care treatment, an intensive neurological rehabilitation program including robotic rehabilitation is needed.
Traumatic brain injury is a brain injury that occurs when the head is suddenly and violently struck by an object or when an object pierces the skull and damages the brain tissue. It can lead to impairments in the cognitive and physical functions of the person, causing impairments in thinking, perception, speech, swallowing and paralysis of organs such as arms and legs. Although it can occur almost anywhere and at any age, it is most common in young people, especially between the ages of 15-25. Motorcycle and bicycle accidents are an important cause. The use of helmets significantly reduces the occurrence of traumatic brain injury in such accidents. Falls and non-accidental traumas in children, traffic accidents in adults and falls in the elderly are common causes of head trauma.
What are the symptoms of traumatic brain injury?
Since the brain is the most sensitive and complex organ of the body, traumatic brain injuries can lead to changes that profoundly affect a person’s life. These changes can be cognitive changes such as memory, perception, attention, understanding, logical thinking or physical problems such as partial or complete paralysis, balance disorders, swallowing and speech disorders.
The mortality rate in the early stages of traumatic brain injury is quite high. Depending on the severity of the trauma, loss of consciousness, nausea, headache, neurological and cognitive effects are common. Depending on the location and extent of the brain damage, patients may experience many health problems such as loss of use of arms and hands, gait impairment, sensory impairment, impaired intellectual functions, behavioral and personality changes, epileptic seizures, chronic pain, depression, bladder and bowel problems. Cognitive problems such as decreased attention span, difficulty in organizing thoughts, forgetfulness, confusion, difficulties in learning new information, difficulties in reasoning and interpretation, inappropriate behavior in social situations, difficulty in problem solving, decision making and planning may occur. Language problems, like cognitive problems, can vary from person to person. These problems include difficulty in finding words, inability to form proper sentences, long and inaccurate expressions, difficulty in understanding words, inability to understand different uses of words, idioms and innuendos, decline in reading and writing skills, and deterioration in math skills. Behavioral disorders such as personality changes, aggression, tendency to violence and loss of control can also occur as a result of traumatic brain injury. Physical limitations such as partial or complete paralysis, involuntary muscle contractions (spasticity), impaired balance and coordination, and difficulty swallowing can reduce the person’s functional independence. These symptoms vary according to many factors such as the severity of the injury, the affected brain region, injuries to organs other than the brain and pre-injury personality traits.
How is traumatic brain injury treated?
Patients with traumatic brain injury require emergency intervention followed by early intervention by neurosurgery and neurology clinics. This intervention may take the form of intensive care follow-up or surgical intervention. The priorities of this intervention are to ensure oxygen supply and adequate blood flow to the brain and the rest of the body and to control blood pressure. Once the medical condition has stabilized, the patient should be immediately evaluated by a physical therapy rehabilitation physician and an early rehabilitation program should be initiated. When the patient becomes eligible, the best option would be to follow the patient in a physical therapy and rehabilitation clinic with specialized neurorehabilitation and robotic rehabilitation facilities.
The recovery that occurs with the disappearance of edema in the brain tissue after the early period is called spontaneous recovery. In the later period, the sprouting of nerve cells and the formation of new nerve connections contribute to the continuation of recovery. Research has shown that neurological recovery after brain injury is greatest in the first 6 months. However, recovery after brain injury continues rapidly for up to 2 years. During this period, a comprehensive physical therapy and rehabilitation program will maximize the patient’s gains. Although recovery is faster in the first 2 years, these patients may also have the potential for late recovery. Even in patients who are thought to have permanent cognitive and physical impairments, some abilities can be regained.
For this reason, it would be beneficial for a patient who has suffered a brain injury to be continuously monitored by a team of doctors consisting of neurology, neurosurgery and psychiatry specialists under the leadership of a physical therapy and rehabilitation specialist.
Rehabilitation in traumatic brain injury
Nowadays, thanks to the increasing and developing surgical and emergency aid methods, deaths due to traumatic brain injuries are decreasing, while rehabilitation and reintegration of patients into the society are gaining importance due to the increase in survival rate. The aim of rehabilitation in traumatic brain injury is to improve impaired functions, to enable walking, to restore the patient to the highest possible level of independence and to prevent other health problems that may occur due to the disease.
Rehabilitation in traumatic brain injury should be started early. Simple measures such as passive joint movements and turning the patient every two hours while the patient is in intensive care or even unconscious can prevent problems such as joint restrictions and pressure sores that may affect the success of rehabilitation in the future. Therefore, it is important that the patient is followed up by a physical therapy and rehabilitation specialist from an early stage. In this way, complications that may arise in the acute period are prevented and the patient is prepared for transfer to a rehabilitation clinic.
Patients who become medically stable are enrolled in a more intensive and comprehensive rehabilitation program. At the beginning of rehabilitation, the patient is evaluated in terms of level of consciousness, motor, sensory, perception, balance, gait and activities of daily living with a comprehensive examination and a special physical therapy and rehabilitation program is planned for the patient. This program is followed up with weekly evaluations and shaped according to newly determined goals.
Early mobilization of patients with traumatic brain injury is important. This prevents complications such as muscle atrophy, pressure sores, osteoporosis, joint restrictions and soft tissue calcifications that may arise due to immobilization. The physical therapy and rehabilitation program includes in-bed mobilization, sitting balance training, use of hands and arms, getting out of bed and transfer activities, standing up, standing balance training, walking, climbing up and down stairs, work-occupation and training of activities of daily living in accordance with the patient’s current medical condition and functional level.
Traumatic brain injury can cause involuntary muscle contractions called spasticity. If these contractions disrupt the patient’s joint movements, positioning, hygiene or cause pain during exercise, they need to be treated. In addition to medications, physical therapy and exercises, interventional and surgical methods can also be applied.
If the patient has joint contracture, range of motion exercises, stretching, bracing or surgical intervention may be required. Muscle weakness can be seen in traumatic brain injury. In these cases, muscle strengthening exercises are used to bring the muscles back to normal strength. If there are balance and coordination disorders, exercises are also performed. Orthotics and other assistive devices can be utilized during these studies when needed.
Robotic rehabilitation is an effective rehabilitation method that can be used from the early period in patients with traumatic brain injury. It contributes to the early mobilization of the patient, stimulates neurological recovery through neuroplasticity and increases the patient’s compliance with the rehabilitation program, motivation and awareness. Early Stroke Mobilization Device (vertical movement device with electrical stimulation), Walking Robot (robotic walking device), Armeo (shoulder-arm robot) and Amadeo (hand-finger robot) are among the robotic technologies used for this purpose. Integrating robotic rehabilitation into the rehabilitation program from an early stage significantly increases success in the rehabilitation of patients with brain injury.
Hydrotherapy, or in-water rehabilitation, is another rehabilitation option that has a place in the treatment of patients with traumatic brain injury. In-water exercises help to strengthen weak muscles, improve balance and coordination, and reduce involuntary muscle contractions.
Occupational therapy (occupational therapy) is a therapy and rehabilitation program that aims to improve the quality of life of individuals by improving their independence and life roles in daily life through work, occupation and activity. Occupational therapy is also actively used in the treatment of patients with traumatic brain injury.
Speech and language therapy and swallowing therapy are very important in the rehabilitation of patients with traumatic brain injury. First of all, the specialist therapist determines the areas where the patient is inadequate and organizes a treatment program for them. If necessary, a cognitive assessment can also be applied. In addition to exercises for speech and swallowing, cognitive problems such as forgetfulness are also addressed.
Respiratory rehabilitation, psychotherapy, neuropathic pain management and treatment of bladder and bowel problems are other important aspects of rehabilitation for patients with traumatic brain injury.
The success of rehabilitation in traumatic brain injury is influenced by many factors such as the severity of the brain injury, age, gender, pre-illness status, socioeconomic parameters, and the state of cognitive functions. Although the process is long and clinical recovery is sometimes very slow, these patients, most of whom are young, can lead an independent and productive life with an appropriate rehabilitation program. If the patient is not included in a rehabilitation program that is designed for him/her in every aspect, he/she will fall behind in his/her performance. The ultimate goal of rehabilitation is to complete the vocational and economic rehabilitation of patients who have suffered traumatic brain injury, and if they cannot continue their old profession, they should be given a new profession or placed in a suitable job and brought to a self-sufficient, productive life level.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is the spinal cord?
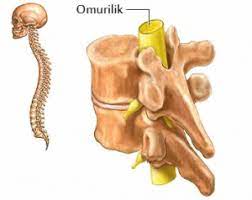
The spinal cord is a bundle of nerves that is part of the central nervous system as a continuation of the brain located in the spine. All the nerves to our arms and legs and some nerves to the muscles of the chest, bladder, bowel and genitals exit from the spinal cord.
What are the causes of spinal cord injury?
The spinal cord travels in the spinal canal in the middle of the spine extending from the brain to the neck, back, waist and coccyx and is protected by this bone structure. When the spine is damaged for any reason, the spinal cord is damaged and a spinal cord injury occurs. The most common cause of spinal cord injury in the world and in our country is traffic accidents. After that, falls from heights, gunshot wounds, sports injuries, especially jumping into shallow water are the most common causes of traumatic spinal cord injuries. In addition to traumatic causes, non-traumatic causes such as spinal cord tumors, spinal cord infections, motor neuron diseases and disc herniations may cause spinal cord injury.
What is the clinical picture after a spinal cord injury?
Depending on the level of injury, different types of paralysis occur. This picture is generally referred to as spinal cord injuries.
What are paraplegia and tetraplegia?
Injury to the spinal cord in the spinal canal in the neck region results in motor and/or sensory loss or impairment and dysfunction of the arms, trunk, legs and pelvic organs is called tetraplegia, and injury to the spinal cord in the spinal canal in the back and waist region results in motor and/or sensory loss or impairment and dysfunction of the trunk, legs and pelvic organs is called paraplegia.
What is a complete and incomplete injury?
If the spinal cord is completely damaged at the level of the spinal fracture, there is a complete loss of movement and sensation below the level of injury and this is called a complete injury and is referred to as ASIA A. However, if the spinal cord is partially damaged at the level of the fracture, the loss of movement and sensation below the level of injury is also partial and this is called incomplete injury and is expressed as ASIA B-C-D-E depending on the movement.
What are the Problems that can be seen in Patients?
The most important problem is partial or complete loss of movement and sensation in the muscles below the level of injury, depending on the level of injury and whether the injury is complete or incomplete. Since the nerve to the bladder and intestines will be affected, problems in feeling or controlling the large bladder and urine and related urinary tract problems and intestinal problems are observed. If the bladder cannot be emptied sufficiently, blood pressure problems that reach dangerous levels can be seen. If adequate bladder rehabilitation is not performed, the patient may face conditions leading to kidney failure in the future. Since the patient is constantly lying down, bed sores develop if good monitoring and positioning is not done. Bed sores are very difficult to heal and treat. Since the muscles and bones are not used due to lying down, muscle and bone resorption may occur and movement limitations may develop in the joints. Severe and unbearable neuropathic pain and spasticity are problems that hinder the rehabilitation program and affect the patient’s quality of life. Patients with spinal cord injury may also have problems with sexual function.
Will they benefit from rehabilitation?
Unfortunately, paralysis caused by spinal cord injuries is irreversible if it is a complete injury. In patients with partial spinal cord injury, partial or complete return of movement can be seen within a few months/years. Early and qualified rehabilitation is essential to prevent the above-mentioned problems in patients with both complete and partial spinal cord injuries and to enable the patient to continue his/her life independently by using the remaining functions in the best way possible.
What is done in rehabilitation?
In patients with spinal cord injury, the aim is to prevent complications and ensure the patient’s independence in life. For this purpose, the main goal is to try to regain strength in muscles that have lost strength. For this purpose, conventional treatment approaches such as range of motion exercises, stretching exercises, muscle strengthening exercises, neurofacilitation techniques as well as newer and advanced rehabilitation approaches such as robotic rehabilitation, pool treatments, virtual reality treatments, biofeedback, functional neuromuscular electrical stimulation, transcranial magnetic stimulation techniques can be included in the treatment plan. In addition, regular bladder and bowel emptying and adequate follow-up, air mattresses and positioning to prevent bedsores, in-bed exercises to prevent muscle and bone loss, and bringing the patient to a vertical position as soon as possible, walking appropriate patients with devices and external supports over time, and developing self-sufficient wheelchair transfers for patients who cannot walk should be included in the rehabilitation program.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
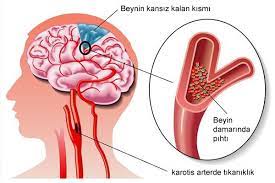
What is a stroke?
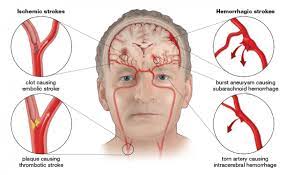
Stroke is a non-traumatic damage to brain tissue due to impaired blood supply to a region of the brain as a result of blockage (clotting or gradual narrowing of the vessel diameter over time) or bleeding in the brain vessels.
What are the Risk Factors for Stroke?
The known risk factors for stroke are divided into two groups: modifiable and non-modifiable risk factors. Non-modifiable risk factors include age, gender, race, family history, history of previous stroke or occlusion attack.
Modifiable risk factors are as follows:
- High Blood Pressure
- Diabetes (Diabetes)
- Cigarette smoking
- Excessive alcohol use
- Obesity
- Wrong eating habits
- Hyperlipidemia (elevated blood fats)
- Lack of physical movement
- Heart rhythm disorders
- Heart valve diseases
Studies show that approximately 90% of stroke cases are due to modifiable risk factors and therefore preventable.
What is the Clinical Picture of Stroke?
Stroke usually results in motor loss (weakness) in one half of the body depending on the location of the lesion, sensory impairment, balance coordination disorder, speech and swallowing disorders, urinary and fecal incontinence and cognitive function loss up to coma.
How is Stroke Treatment Administered?
Stroke treatment should start immediately after the stroke. If treatment is started within hours, permanent damage to brain tissue can be prevented. For this reason, medical treatment is applied according to the type of stroke and the clinical condition of the patient in the early period. Rehabilitation is also a part of this treatment and it is important to start early. You can get information about Romatem Early Rehabilitation Camp from our call center.
What is the Goal of Stroke Rehabilitation?
The aim of rehabilitation of stroke patients is to enable them to live as independently as possible with maximum quality of life. While the first aim is to restore impaired functions, one of the main goals of the rehabilitation program is to take all measures to treat and prevent certain complications that arise after stroke.
What are the Most Important Problems Requiring Rehabilitation in Stroke Patients?
Ambulation (walking) problems and upper extremity (arms and hands) function losses are at the forefront in patients after stroke. Especially ambulation and walking problems are the problems that cause the most dependency in patients. Shoulder, arm and hand problems are important in terms of both causing pain and causing limitations in daily life activities.
Is There Recovery After Stroke? Who Needs Rehabilitation Program?
Approximately 10 percent of stroke patients can return to work and daily life activities without sequelae. Another 10 percent need continuous care in inpatient care centers despite everything. The remaining 80 percent need an active rehabilitation program.
Does the brain regenerate itself? Does it heal on its own? What is the most important factor affecting this?
In recent years, studies on neurophysiological mechanisms have intensified and it has been understood that the brain has a great potential for clinical recovery and adaptation after stroke. With this mechanism called neuroplasticity, there is a restructuring in the brain and the brain renews itself. And it has been seen that rehabilitation approaches are the factor that best functions or activates this potential, and it has been understood that rehabilitation plays a key role in reducing sequelae and disability after stroke.
What are the Complications (problems) After Stroke?
Stroke can cause motor loss (weakness) in one half of the body, sensory impairment, balance and coordination disorders, speech and swallowing disorders, urinary and fecal incontinence, and a clinical picture that can go from loss of cognitive function to coma. In addition, complications such as joint contractures, movement limitations, spasticity, shoulder dislocation and shoulder pain, bladder dysfunction, bowel dysfunction, deep vein thrombosis, speech problems, swallowing problems, pressure sores, depression, sleep problems, infections, osteoporosis, falls and fractures, shoulder-hand syndrome and brachial plexus lesions may occur.
What is done in a Stroke Rehabilitation Program?
In the stroke rehabilitation program, conventional treatment approaches such as range of motion exercises, stretching exercises, muscle strengthening exercises, balance and gait training, neurofacilitation techniques, as well as newer and advanced rehabilitation approaches such as robotic rehabilitation, pool treatments, mirror treatments, compulsory use treatments, virtual reality treatments, biofeedback, functional neuromuscular electrical stimulation, transcranial magnetic stimulation techniques can be included in the treatment plan.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Chiropractic Treatment?

“Chiropractic” is a Greek word; it is composed of the words chiro (hand) and practic (practice). In other words, it means manual treatment.
Since the basis of this manual treatment is the manipulation of the spine, it is also known as “manipulation” or “spinal manipulation treatment” in most places. It is a scientific and more complicated form of the treatment known colloquially as “pulling”.
The main purpose of chiropractic treatment, i.e. spinal manipulation treatment, is to eliminate the malalignment of the spine and regulate the functions of the body.
How does chiropractic treatment work?
Our spinal cord, which is the continuation of our brain, is located behind our vertebrae. The spinal cord provides communication between the nerves that run throughout the body and the brain. Some disorders in the structure or placement of the vertebrae also affect the spinal cord. Over time, due to various reasons (trauma, stress, posture disorder, hernia, etc.), the natural structure of the spine deteriorates. In this case, there may be some disruptions in the communication between the brain and the body. These often manifest themselves as pain or dysfunction (constipation, excessive sweating, insomnia, etc.).
Chiropractic correction of treatable misalignments of the spine, i.e. manual manipulation of the spine, improves existing dysfunctions or pain.
The main goal is to correct the misalignment and thus ensure healthy communication between the brain, nervous system and organs.
Chiropractic treatment is a “scientific” treatment method accepted by the World Health Organization. In addition, the American Medical Association recommends chiropractic treatment as the first choice in the treatment of back and neck pain.
How Many Sessions of Chiropractic?
Depending on the condition of the patient and the disease, 2 sessions per week, 1 session per week, 1 session every two weeks or 1 session per month. An average of 6-8 sessions are planned. Combining it with physical therapy and exercise increases the effectiveness of the treatment and reduces the duration of treatment.
In Which Diseases Can Chiropractic Be Applied?
- In lumbar and neck hernias
- Low back, neck and back pain due to posture disorder
- Stress-related widespread muscle aches
- Myofascial pain syndromes
- Fibromyalgia
- Sports injuries
- Headaches
- Are Chiropractic and Chiropractic the Same Thing?
Unfortunately, due to the lack of knowledge and supervision in this field in our country, the scientific value of the treatment is lowered by giving it certain names such as stumping treatment, and some people who do not have sufficient knowledge and authorization apply it to patients who are looking for a solution to their problems by saying “I am an expert in this field”. These people widely advertise and advertise, especially on social media, using the sound of gas coming out of the joints as a result of the sudden manipulation of the spine during the treatment as an indicator of the success or effectiveness of the treatment, trying to convince patients that the procedure is successful with statements such as “I put it in place, I placed it in place”. Patients who are temporarily relieved by the release of gas from the joint believe that they are receiving an effective treatment. However, the patient’s complaints return when the gas fills the joint again after a while. Especially in these matters, patients should be very careful and should not have this treatment applied to them without thorough research.
Chiropractic treatment is a highly effective scientific treatment method without side effects when applied by experts. However, whether the person is suitable for chiropractic treatment should be decided after being evaluated by a physician.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Low back pain

Low back pain is an important health problem because of its high prevalence and the significant loss of financial resources, labor and time it causes.
The proportion of people who have experienced severe low back pain at least once in their lifetime is 75-85%. It is the most common reason for presentation to primary care physicians in the adult population.
The lumbar region is the center of gravity of the body and is affected by almost all body movements. Therefore, it is a region subjected to constant and repetitive strain.
Causes of low back pain
The causes of low back pain can be divided into mechanical and degenerative causes and inflammatory causes.
Mechanical and degenerative causes
They account for approximately 95% of all low back pain. Mechanical causes include lumbarization, sacralization, increased lumbar lordosis, disc herniations, trauma and low back pain due to weak muscles.
Degenerative causes are the aging of tissues and the deterioration of their structure due to other reasons and calcification.
In mechanical and degenerative low back pain; in general, there is pain that decreases with rest, increases with movement, often decreases with heat, increases with cold, increases or decreases depending on the position, and causes short-term stiffness in the morning. There is no deterioration in blood tests.
Inflammatory causes of low back pain
The term inflammatory refers to inflammatory involvement. Inflammatory causes include inflammatory rheumatism (Ankylosing Spondylitis), infectious causes (brucellosis, tuberculosis) and cancer-related involvement.
In low back pain due to inflammatory causes, pain increases with rest. The pain increases at night and decreases when you get out of bed and move. Morning stiffness lasting more than half an hour. Pain increases with hot applications. Blood tests showing inflammation (sedimentation, crp, etc.) deteriorate.
How is the treatment done?
Medication and rest
In degenerative and mechanical low back pain, anti-inflammatory drugs and cortisone may be necessary in the acute phase. In the chronic phase, simple painkillers may be sufficient. In acute (new onset) low back pain, a few days of complete bed rest is sufficient. After resting, the patient should gradually return to normal daily movements over time.
Exercise and Physical Therapy
Strengthening the muscles and maintaining a certain degree of flexibility are extremely important in counteracting the loads placed on the lumbar vertebrae. These require certain exercises to be performed. It is important to keep in mind that not all exercises are suitable for every patient, depending on whether the disease is acute or chronic, the form of the disease, the physical and social needs of the patient and the age of the patient. In other words, exercises should be tailored to the patient. Exercises should be given to the patient by his/her physician.
Various physical therapy applications (superficial heaters, deep heaters, analgesic currents, traction methods) can be applied to patients with low back pain. The pain relieving, muscle relaxant, tissue regenerating and repairing effects of these applications are utilized. The type and duration of physical therapy applications should be prescribed and applied according to the characteristics of the patient and the disease.
Is surgical intervention necessary in low back pain?
Surgical treatment in cases of low back pain is a necessary treatment method in cases of progressive loss of strength in the foot or leg in cases where multiple nerve roots are affected at the same time and the nerves leading to the bladder are also affected, known in medicine as cauda equina syndrome. The situation should be evaluated very well in surgeries performed only to relieve pain.
Various complementary medicine treatment methods can also be used to get rid of low back pain. These include acupuncture, spinal manipulation, meso, prolotherapy and ozone.
Rules for maintaining back health
- The person, object or thing being looked at should be turned fully body-facing.
- Do not stay in the same position for long periods of time. Sitting and standing time should not exceed 45 minutes.
- A pillow that supports the waist should be used when sitting.
- Care should be taken to squat when working on the ground.
- The lumbar region should be protected from sweat and cold
- An orthopedic mattress should be used for sleeping.
- It is best to lie on the side, bending forward and pulling the legs towards the abdomen.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Scoliosis?
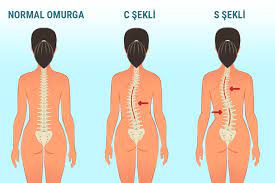
Scoliosis is defined as a curvature of more than 10 degrees to the right or left of the spine, which should normally lie in a straight line when viewed from the back. Scoliosis is not just a one-dimensional angular deformation, but a bony and structural distortion that affects the body in three dimensions, from the front and side.
Scoliosis is a disorder that can be seen at any stage of life. Genetic transmission is responsible for scoliosis. If the scoliosis angle is high, the visual effect of the body is very impaired. This cosmetic defect affects these young children at the beginning of puberty not only as a health problem but also visually, and it disrupts their confidence in their own bodies and causes psychological problems. Apart from the cosmetic defect, as the angle of curvature of scoliosis increases, complaints such as shortness of breath, bloating, rapid fatigue, shortness of breath due to compression of the lungs and heart in the chest cage, especially back and lower back pain, may occur. As a result, it can negatively affect the quality of life.
What are the Types of Scoliosis?
Idiopathic scoliosis (Scoliosis of unknown cause)
The most common type of scoliosis is ‘adolescent idiopathic’ scoliosis, the cause of which is not fully understood. The sideways bending of the spine may be ‘S’ or ‘C’ shaped. In addition to sideways bending, rotation of the vertebrae around themselves is seen in all idiopathic scoliosis, including the mildest forms. This rotation of the vertebrae causes asymmetrical protrusions on the back or waist. Genetic and environmental factors are emphasized in the etiology. It is 8-10 times more common in girls during adolescence.
Neuromuscular Scoliosis
The second most common type of scoliosis is neuromuscular scoliosis. The main cause of neuromuscular scoliosis is due to underlying muscle and nerve disease. Nerve diseases can originate in the brain and spinal cord, while muscle diseases can be seen in childhood and later in life. It can be seen in cerebral palsy (CP), polio (polio), meningomyelocele, muscular dystrophy, tethered cord syndrome.
Unlike idiopathic scoliosis, respiratory distress and sensory defects are more common in neuromuscular scoliosis.
Congenital Scoliosis
The third most common type is congenital scoliosis. It is a type of scoliosis caused by spinal anomalies that occur during the development of the child in the womb. Congenital scoliosis progresses rapidly in the early years. For this reason, the treatment process of congenital scoliosis that occurs in early periods may require surgical intervention at an early age. The cause of congenital scoliosis is not fully explained. Some conditions can be seen more frequently with congenital spinal deformities due to certain events that occur during the development of the embryo and fetus.
Scoliosis in Adults
Adult idiopathic scoliosis
In adult idiopathic scoliosis, severe pain may occur due to degeneration in the facet joints. Due to excessive deformation of the rib cage, respiratory functions may be affected and patients may experience fatigue and respiratory distress.
Adult degenerative scoliosis
Adult degenerative scoliosis is a type of scoliosis that occurs as a result of wear and tear on the spine with aging. It usually occurs in people over the age of 50. Osteoporosis, which also occurs at this age, can be one of the causes of adult degenerative scoliosis and can also cause an increase in curvature. Degenerative scoliosis caused by wear and tear can be seen in any of the neck, back and waist regions of the spine; however, the most common region is the lumbar region.
In people with advanced adult degenerative scoliosis, the stability and balance of the spine may be impaired. This may cause the spine and torso to tilt sideways in the anterior and posterior planes and the torso to tilt forward with a decrease in the anatomical angle of the lumbar region. These imbalances can lead to an increase in the severity of the curvature and can also affect the patient’s mobility and cause pain.
In adult patients with degenerative scoliosis, back pain, low back pain and pain along the distribution area of the nerve due to nerve compression (radiculopathy) and loss of strength in the muscles supplied by the nerve can be observed. In these deformities that may occur in the spine structure, spondylolysis may cause the spine bone to shift forward. Physiotherapy programs, stabilization, strengthening and stretching exercises can relieve muscle spasm and reduce pain. Scoliosis can also develop in adults with a diagnosis of rheumatic disease, osteoporosis and after trauma and infections.
What are the Symptoms of Scoliosis?
Scoliosis does not cause any health problems in the early stages, and back pain can be seen very rarely. Therefore, it can be difficult for families to recognize if they are not careful. Symptoms of scoliosis are visual features such as one shoulder being higher than the other, the hips shifting to the right/left or the hips standing high on one side, and uneven posture of the shoulder blades. The healthiest method, which parents should do regularly, is to lean forward with the child’s bare back and visually examine whether the spine is in a straight line. At the end of such a check, if scoliosis is present, a protruding elevation on the right or path of the back or in the lumbar region will be noticeable.
Another situation that families should be aware of is that scoliosis can be seen at the age of 10-16 and since it is not known when it will appear, this spine should be checked frequently. Particular attention should be paid to children with symptoms of adolescence. When scoliosis is suspected, a physician should be consulted immediately.
What is done during the diagnosis of scoliosis?
After a detailed history is taken and examined by the physician, imaging methods are used. It is possible to make a definitive diagnosis with standing spine radiographs. Rarely, advanced radiologic examinations of the spine (MRI films) are also requested to differentiate other causes. In recent years, body topographic analysis systems that do not involve X-rays and allow curvature monitoring have become more frequently used.
The most important thing in scoliosis is early diagnosis. For this reason, families should check the spine of their children between the ages of 10-16 and consult a physician immediately if there is any doubt.
What are the Treatment Steps in Scoliosis?
There are certain algorithms for the treatment of scoliosis. If it is detected early, if it is detected at a low angle, it is a candidate for conservative (protective) treatments. Treatments in scoliosis are observation, physiotherapy and rehabilitation practices, corseting and surgery.
The treatment of scoliosis is determined by the degree of curvature and the stage of growth. Currently accepted non-surgical treatment methods include scoliosis-specific exercises, special scoliosis programs and bracing. The main goal of scoliosis treatment is to prevent the progression of the curve, maintain the mobility of the child’s spine, control cosmetic deterioration and prevent surgery.
Exercise applications are extremely important in scoliosis. Three-dimensional scoliosis exercises, known as Schroth exercises, are planned individually for each individual according to the affected body part. The aim is to control the pelvis and the muscles and ligaments around the affected spine and to control body cosmetics. For this purpose, mobilization, spinal traction, flexibility and correct posture control and control of the spine in daily life activities are based. Regular exercises and the use of a correct and biomechanically controlled corset for an appropriate period of time increase the postural balance of the child and control the progression of the angle in scoliosis. Breathing techniques are also included in scoliosis exercise programs. In recent years, there are device-supported programs that allow spinal exercises to be integrated into a game-like environment on the computer. With Valedo, it is possible to work on exercises in standing, sitting and plank positions.
Correction is ideally performed after the age of 10 years, when the risser stage is 0-2 (early stages of bone development), the Cobb angle is between 20-40 degrees and before menarche or within a maximum of 1 year after menarche.
Surgical treatment is applied if the Cobb angle is above 40 degrees in individuals with a high risk of progression, where conservative methods fail. In scoliosis surgery, the spine is moved to the midline with plates and screws and the progression of scoliosis is controlled. In young children, the operation may need to be repeated at certain intervals to allow the spine to lengthen.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Pediatric Rehabilitation?

The pediatric rehabilitation program provides comprehensive multidisciplinary rehabilitation care for children. The goal is to minimize the effects of disabilities while maximizing the abilities of each individual child. This is achieved through effective rehabilitation of the highest quality provided in a family-centered environment.
Depending on the nature of the impairment and the needs of the child, treatment takes place in a variety of settings and utilizes the diverse skills of rehabilitation professionals to promote the highest level of function possible. The pediatric rehabilitation team aims to help each individual achieve full functional independence in self-care, mobility, communication, cognition and socialization. It is applied to treat disorders such as vision, hearing, swallowing and speech in children. It is also applied in the treatment of genetic disorders and muscle diseases.
In Which Conditions Is Pediatric Rehabilitation Applied?
Pediatric rehabilitation is also applied in cases such as congenital muscle coordination disorder or subsequent disorders, disruption of skeletal and muscular system balance in children and helps to treat disorders.
With pediatric rehabilitation, problems related to crawling, walking and manual grasping in children can be treated. In addition, pediatric rehabilitation treatment is also applied in the treatment of diseases such as cerebral palsy and spina bifida. Pediatric rehabilitation provides highly successful results in spinal cord damage, musculoskeletal disorders, head injuries or traumas, walking and crawling disorders.
What are the Techniques Used in Pediatric Rehabilitation?
Various treatment techniques are used in pediatric rehabilitation:
The most effective treatment technique used in pediatric rehabilitation is rehabilitation exercises. Rehabilitation exercises aim to give children muscle strength. Pediatric rehabilitation practices are also used for the proper functioning of the skeletal and bone system.
Standing table is among the tools used in pediatric rehabilitation applications. The child can stand with the support of the standing stand and the skeletal and muscular system can be strengthened.
It is very important to start treatment early to get more effective results with pediatric rehabilitation. At this point, parents have an important role. It is very important to follow their children’s development closely and to visit the doctor taking into account the problems they encounter. The symptoms that should be considered in the development process of children are as follows:
Things to pay attention to in a 1-month-old baby:
- All kinds of breast sucking problems
- No reaction to warnings from the environment
- Continuous and uninterrupted crying spells
- Very frequent and severe vomiting
- Transferral seizures
Things to consider in a 2-month-old baby:
- All kinds of breast sucking problems
- No reaction to warnings from the environment
- Continuous and uninterrupted crying spells
- Very frequent and severe vomiting
- Transferral seizures
- Loss of reflexes
- Laxity or excessive stiffness in the muscles
Things to consider in a 3-month-old baby:
- Shift and twitching of the eyes
- Cramping and discomfort when lying on your back
- Failure to start laughing
- Not knowing the mother
- Not looking the speaker in the face
Things to consider in a 4-month-old baby:
- Still unable to control his head
- Inability to focus the eye on a certain point
- Hands are not released but constantly made into fists
- Some reflexes should disappear by 4 months of age. These reflexes do not disappear,
Things to consider in an 8-month-old baby:
- Unable to turn and move on their own
- Hand coordination skills are not developed
- Attempting to kick with both legs
- Collapse of the body on the legs while sitting
Things to watch out for in a 10-month-old baby:
- The baby still cannot crawl
- Inability to stand up
- Not reacting to his name
- Inability to perform coordinations such as controlling saliva
Things to watch out for in a 1 year old baby:
- Not even starting to walk while holding on
- Inability to walk on tiptoe
Other Conditions that can be treated with Pediatric Rehabilitation
- Spina Bifida (separation or opening of the spine)
- Brain Stroke
- Multiple Sclerosis
- Congenital Anomalies
- Orthopedic Disorders
- Stress Injuries
- Muscular Dystrophy
- Swallowing Problems
- Nutrition Problems
- Daily Living Rehabilitation Activities
- Juvenile Arthritis (Joint inflammation)
- Rehabilitation after Fracture
- Preoperative Rehabilitation
- Humpback
- Osgood-Schlatter Disease (childhood knee pain)
- Wheelchair Use
- Use of Assistive Devices
- Hand and Arm Injuries
- Foot and Leg Injuries
Pediatric rehabilitation techniques are as follows:
- Activities of Daily Life Education
- Joint Treatment
- Developer Communication
- Basic Sign Language
- Nutrition Therapy
- Gait Analysis / Training
- Handwriting
- Neurodevelopmental Therapy
- Oral-Motor Interventions
- Orthotics / Prosthetics Training
- Pragmatic / Social Skills Training
- Sensory Integration
- Wheelchair Seating and Equipment Assessment
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Ozone?

Ozone is one of the most important gases in the stratosphere layer of the atmosphere. It provides a protective filter mechanism against the high-energy ultraviolet rays emitted by the sun and helps to maintain the biological balance in the biosphere. After the 1960s, the increasing contamination of drinking water with chemicals became an intense problem. After the realization of the cleaning and disinfecting effects of ozone, ozone has been used to clean water. In addition, ozone has been used in many areas of industry.
Ozone (O³) is a 3-atom molecule and is a very high energy form of oxygen (O²). Ozone is a gas at room temperature. It is a colorless gas with a characteristic odor that can be felt after stormy weather, in high places or on the seashore.
Ozone used in medicine is produced from pure oxygen in special generators.
Ozone Mechanism of Action
Ozone can neutralize all toxins (phenols, pesticides, detergents, chemical wastes and aromatic compounds) as well as killing microorganisms due to its strong oxidizing properties.
Depending on age, reactive oxygen species cause oxidative damage to cells. This is called increased oxidative stress. In recent studies, it has been shown that the products produced by low doses of reactive oxygen to the body with ozone application are involved in biological mechanisms, especially intracellular communication, in low amounts (physiological levels) and mediate therapeutic effects. As a result of repeated low-dose ozone applications, the antioxidant system is strengthened and resistance to oxidative stress develops.
In addition, reactive oxygen species enter the cell and increase the production of cytokine levels and growth factors that reduce inflammation. Ozone therapy is used as an auxiliary treatment method especially in diseases where the inflammatory process is intense and the immune system is at the forefront (wound healing, ischemic, rheumatic and infectious diseases.
Accelerates cell regeneration.
Ozone increases the oxygen-carrying capacity and elasticity of red blood cells and the fluidity of the blood, eliminating oxygen deficiency. It is also applied as an auxiliary treatment in vascular occlusion by causing vasodilation and vascular occlusion.
By interacting directly with fat cells, it causes a decrease in cholesterol and regional fat destruction.
It lowers blood sugar levels.
It reduces cartilage loss in arthritis and stimulates the production of intra-articular fluids and cartilage, resulting in a decrease in joint pain and an increase in mobility.
Ozone, known as the elixir of youth, is now very effective in the treatment of chronic diseases.
Diseases in which Ozone Therapy is Useful
- Osteomyelitis, pleural emphysema, abscesses with fistula, infected wounds, pressure sores, chronic ulcers, diabetic foot and burns
- Hypertension
- Diabetes Mellitus
- Advanced ischemic diseases
- Macular degeneration of the eye (atrophic form)
- Musculoskeletal diseases and joint calcifications
- Chronic fatigue syndrome and fibromyalgia
- Chronic and recurrent infections and sores in the oral cavity
- Acute and chronic infectious diseases (hepatitis, HIV-AIDS, herpes and herpes zoster infection, papillomavirus infections, onychomycosis and candidiasis, giardiasis and cryptosporidiosis), especially those caused by bacteria, viruses and fungi resistant to antibiotics and chemical treatments. Bartolinitis and vaginal candidiasis.
- Allergy and Asthma
- Autoimmune diseases (multiple sclerosis, rheumatoid arthritis, Crohn’s disease)
- Senile dementia (dementia due to old age)
- Lung diseases: emphysema, chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis and acute respiratory stress syndrome
- Skin diseases: Psoriasis and atopic dermatitis
- Cancer-related fatigue
- Early stage renal failure
Benefits of Ozone Therapy
- It accelerates blood circulation to cells and tissues,
- It strengthens the immune system and increases resistance to infectious diseases,
- It regenerates the vessels (arteries and veins) and improves blood pressure,
- Cleanses the blood and lymph system,
- It allows the skin to function like a third kidney or a second lung system,
- Cleaner, softer and more rejuvenated skin,
- By removing the toxin accumulated in the muscles, it relaxes and softens the muscles and increases their flexibility,
- It cures joint pains and muscle disorders,
- Normalizes hormone and enzyme production,
- Strengthens brain function and memory,
- It relieves depression and boredom,
- By oxidizing adrenaline, known as the stress hormone, it helps to relieve tension caused by depression by providing a general calmness.
What are the Treatment Methods?
Major Method: It is the most widely used method. With this method, 50-200 ml of blood taken from the person, the number of treatment sessions and the dose of ozone to be applied will depend on the general condition, age and the main disease of the patient.
Minor Method: Between 2 – 5 cc of blood taken from the person is mixed with a determined dose of ozone and injected into the person.
Ozone Delivery to Body Cavities: Rectal – Ozone is given to the person through the breech, vaginal and ear canal by spraying method.
Giving ozone gas into joints and muscles: In Musculoskeletal System disorders, a certain dose of ozone gas is injected into the joints and muscles of the person with a suitable needle.
Ozone bag: It is used in non-healing wounds and diabetic feet, skin lesions, infections, circulatory disorders, neuropathic pain and restless leg syndrome.
Ozone cup: Especially used in pressure sores.
Side Effects of Ozone Therapy
Ozone therapy has almost no side effects. The side effects reported so far may develop due to application errors and high doses of ozone according to the antioxidant capacity of the patient. For this reason, ozone therapy should always be applied in a gradual and progressive manner, starting with a low dose and gradually increasing it. In some cases, ozone therapy may be contraindicated. These conditions can be listed as: glucose 6 phosphate dehydrogenase enzyme deficiency, pregnancy, especially in the early stages, angiotensin-converting enzyme (ACE) inhibitor therapy, hyperthyroidism, bleeding disorder, uncontrolled cardiovascular diseases and asthma patients who react to ozone.
Cautions to be Considered
During ozone therapy, all antioxidant supplements containing Vitamin C and Vitamin E should be discontinued. High concentrations of these compounds in the blood affect the effectiveness of ozone as an oxidizing agent and therefore the course of treatment. The patient should be instructed not to consume large amounts of foods rich in these vitamins. As a result, vitamins or antioxidants should be given before or after ozone therapy and never during treatment. Patients should take their blood pressure and sugar medications at least 2 hours before any form of ozone therapy and should not be hungry during ozone therapy.
Ozone therapy is a complementary, supportive and reconstructive method with low risk and usually accompanied by standard medical treatments.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Ozone?

Occupational therapy, also known as occupational therapy, is a therapy and rehabilitation program that aims to improve the quality of life of people by improving their independence and life roles in daily life by acquiring work, occupation and activity. Physically disabled, disabled and mentally ill people gain self-confidence by improving their abilities impaired by illness through occupational therapy. The main aim of occupational therapy is to enable people to participate in daily life activities.
Occupational therapists achieve this goal by improving the ability of individuals and communities to do the activities they want, need or are expected to do, or by organizing the activity or the environment in a way that can better enable people to participate. Therefore, occupational therapy focuses on increasing the competence of people by regulating the person, the activity, the environment or some or all of these to increase social participation. For example; explaining the methods of transition from bed to wheelchair to the patient, cutlery with modified handles for people without hand grip, correct posture and movement habits that prevent back and neck health and occupational injuries in workplaces are included in the field of occupational therapy. Occupational therapy takes into account the mental, physical, emotional and cognitive aspects of the person. It aims to direct the disabled individual to work, to receive vocational training, to be more successful in the workplace.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is facial paralysis?

Facial paralysis is a disease characterized by weakness of the muscles on one side of the face. Facial paralysis occurs mainly for two reasons: firstly, as a result of damage to the body of nerve cells in the brain that supply the facial muscles, and secondly, as a result of damage to the main nerve of the facial muscles. To put it more simply, there are centers in the brain that control the nerve, and if the problem originates from this center, it is usually accompanied by symptoms such as dizziness, epilepsy, paralysis of one side of the body. It is very important to diagnose which type of facial paralysis it is.
What causes facial paralysis?
It can occur for different reasons such as infections, head trauma, cerebral vascular occlusion, head and neck tumors, facial nerve injury. However, in most of the cases, the cause cannot be found and this group is called “Bell’s Palsy”. The good news is that recovery rates are quite high in this group.
What are the symptoms of facial paralysis?
Loss of control in mouth, eye and forehead movements on the affected side is the main finding. However, there may be complaints such as decreased tears, twitching of facial muscles, a different taste sensation on the tongue, speech impairment, excessive saliva and tear production, pain in the ear or around the jaw.
If any of these conditions are accompanied by confusion, dizziness, balance problems, epileptic seizures, weakness in the arms or legs on one side of the body, it is understood that there is a brain-related problem and the treatment algorithm completely changes.
In patients with stroke-related facial paralysis, unlike Bell’s palsy, the ability to blink and wrinkle the forehead on the affected side is preserved.
What is done in facial paralysis treatment?
In facial paralysis diagnosed with Bell’s palsy, treatment is usually started with cortisone group drugs, which studies have shown to have a positive contribution to recovery. However, physical therapy applications such as acupuncture, muscle strengthening with therapeutic level electrical stimulations contribute positively to recovery. Corneal damage caused by dry eye must be prevented.
In facial paralysis with a cause, the cause should be treated correctly in addition to the applications listed in the treatment.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
z.
What is Cerebral Palsy (CP)?

Cerebral palsy, or CP for short, is a non-progressive, permanent movement and posture disorder due to damage to the developing brain. The prevalence of CP is 2-3 per 1000 live births.
What are the causes of Cerebral Palsy (CP)?
CP can be caused by prenatal (low or advanced maternal age, multiple pregnancies, genetic diseases, traumas, maternal diseases), intrapartum (preterm birth, low birth weight, prolonged birth, abnormal presentation and infections) and postnatal (jaundice, infections, trauma, intracranial hemorrhages) causes.
What are the types of Cerebral Palsy (CP)?
- Depending on the location and severity of the damage, CP pictures are formed in various degrees and appearances
- Spastic type: Spastic type is the most common type of cerebral palsy. Spasticity, in the most general sense, can be defined as muscle stiffness or resistance to passive movement. Changes in the normal structure of the muscles and stiffness cause movements to be affected and difficult to perform. Excessive spasticity leads to deterioration of skeletal structure and posture over time. It also negatively affects functional activities such as sitting, using hands and walking.
A spastic child is defined according to the part of the body affected under the diagnosis of Cerebral Palsy:
- Hemiplegia: In this type, the arm, trunk and leg on one side of the body are affected. In children with hemiparesis, crawling is asymmetric or absent. With rehabilitation, most patients become independent in activities of daily living and ambulatory.
- Diplegia: In this type, both legs have more spasticity than the arms. Diplegic patients become spastic after a limp period. Standing and walking are delayed. Children who gain sitting balance by the age of two may be able to walk. Stepping on toes is common.
- Tetraplegia: In this type, the whole body is affected. Inadequate head control, hands in fists and legs crossed in a crossed position is a common appearance. In 1/4 of children with tetraplegic CP, the disease progresses mildly and these patients become ambulatory and can perform activities of daily living with mild limitations. In half of them, the disease progresses moderately and these children cannot be fully independent but can achieve adequate functional capacity. In the remaining 1/4, the disease is severe and these children need lifelong care.
- Athetoid Type: It can be defined as uncontrolled movement. Involuntary movements occur in the child’s legs, arms, hands or face. In this type, sudden changes occur in the muscles. Muscles can change from a very loose state to a very stiff state. This prevents coordinated movements.
- Ataxic Type: There is impairment in maintaining balance. Due to poor head control and lack of trunk balance, development is slow and walking is achieved very late.
- Mixed type: When muscle tone is extremely low in some muscles and extremely high in others, the type of cerebral palsy is called mixed.
What are the signs and symptoms of Cerebral Palsy (CP)?
- Problems with movement on one side of the body
- Hard muscles
- Excessive or loose reflexes
- Involuntary movements or tremors
- Lack of coordination and balance
- Saliva
- Swallowing or sucking problems
- Difficulty with speech (dysarthria)
- Seizures
- Delayed motor skills
- Incontinence
- Gastrointestinal problems
Damage to a developing brain can cause problems other than the movement problems associated with cerebral palsy. Other conditions that may be present alongside cerebral palsy include
- Visual or hearing impairment
- Learning disorders
- Attention deficit hyperactivity disorder (ADHD)
- Inability to communicate through speech
How is Cerebral Palsy (CP) treated?
There is no complete cure for Cerebral Palsy (CP). However, treatment usually improves the child’s abilities.
In Cerebral Palsy (CP), early diagnosis and starting an early rehabilitation program is very important. Treatment is not a definitive and single solution and is a long-term process. In this process, the teamwork of Physical Therapy Physician, physiotherapist, occupational therapist, child development specialist, speech therapist and family is an indisputable issue. All these approaches should be applied together to an individual with CP. Exercise, robotic therapies, hydrotherapy and occupational therapy are the main building blocks of physiotherapy applications, which are the most important pillars of rehabilitation. Exercise applications are applied by physiotherapists according to the functional status of the child, using various techniques to support holding the head, sitting, standing and walking. This long and patient treatment process has been more easily accepted by both children and families with the development of robotic therapies. Thanks to arm and walking robots, repetitive, accurate walking patterns are created and these signals are transmitted to the brain. In addition, applications enriched with a number of games ensure that the treatment is continued with interest by children. Hydrotherapy not only increases the child’s compliance with the treatment, but also facilitates exercise by using the buoyancy of water and increases active participation. Occupational therapy, one of the main branches supporting rehabilitation, includes studies to increase the child’s participation in daily life activities. In addition, Sensory-Integration therapy, which enables the child to receive sensory information from his/her body and environment, organize this information and use it in daily life activities, is among the new applications.
All these applications are included in the rehabilitation process by adjusting their doses according to the type and severity of CP. In addition, this process can be supported by various muscle relaxant applications (such as Botulinum toxin applications) and surgical treatments.
The most important thing is that the individual with CP takes his/her place in the society and is included in life. For this reason, all these applications should be within a plan and with continuous rehabilitation support without disrupting the child’s education process.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Obesity Rehabilitation

Obesity is a condition of excessive fat storage in the body that restricts a person’s daily life and causes comorbidities. There are several different methods to determine excess fat tissue. The most common is the Body Mass Index (BMI). The fat cell is an endocrine cell and adipose tissue is an endocrine organ. As such, adipose tissue secretes a number of substances, including metabolites, cytokines, lipids and coagulation factors among others. Significant excess adiposity or obesity causes increased levels of circulating fatty acids and inflammation. This can lead to insulin resistance and cause type 2 diabetes in the patient.
What are the types of obesity?
The body mass index ratio is very important in defining obesity. People with a body mass index between 30 and 34.90 are overweight, those between 35 and 39.90 are overweight, and those with a body mass index of more than 40 are classified as morbid obesity and cause many comorbid conditions.
What are the diseases caused by obesity?
Obesity itself is a very serious disease that affects the whole life of the person; however, it also leads to comorbidities. The diseases triggered by obesity are as follows:
Obesity can cause type 2 diabetes by causing insulin resistance.
Blood pressure disorders are also among the diseases triggered by obesity. Complaints such as palpitations and shortness of breath negatively affect the quality of life.
Cardiovascular diseases can put a person’s life at serious risk.
The musculoskeletal system can be seriously damaged.
Obesity can also lead to uterine, pelvic and intestinal diseases.
Sleep apnea, which is the problem of respiratory arrest during sleep, is one of the most serious disorders caused by obesity.
What are the causes of obesity?
Obesity can have more than one cause. These include
Eating habits high in calories and fat are the most important cause of obesity. Fast food, fried foods and food products high in sugar should be avoided.
Sedentary life and lack of regular exercise are among the causes of obesity. It is of great importance to burn the calories taken into the body with exercise and movement so that they are not converted into fat and stored.
Obesity is not only caused by improper diet and inadequate exercise. Genetic factors and slow metabolism can also cause excess fat accumulation in the body.
How to prevent obesity?
In order to prevent obesity, metabolic disorders, if any, should be treated first. Then, a healthy diet and regular exercise should become an indispensable part of the lifestyle. Here are ways to prevent obesity:
Healthy and regular eating habits are very important for preventing obesity. Foods low in fat and calories and high in protein and vitamins should be consumed. In addition, portions should be reduced in the amounts that your body can spend and overeating disorder should be eliminated. The daily calorie intake and expenditure should be calculated regularly. In this way, you will take the most important step to reduce the risk of obesity.
It is very important to exercise regularly. Whether it is brisk walking, cycling, swimming or other similar activities, you should make sure that you do them regularly. Burning more calories than you take in from food should be the first goal of your exercise plan.
How is obesity treated?
In the treatment of obesity, first of all, it is ensured that excess weight is lost with the support of an expert dietician and exercise specialist.
The dietician ensures that the patient’s eating habits are completely changed and regulated. A low-calorie, high-nutrient, balanced eating habit is adopted. Most importantly, portions are reduced.
The exercise specialist prepares an exercise program suitable for the general body structure and health of the person. By ensuring that the exercises are performed regularly and consistently, it helps to lose excess weight.
How is obesity rehabilitation applied?
Obesity rehabilitation is a highly effective treatment program applied by physical therapists. The patient is first evaluated by a special team and a personalized treatment program is developed.
With obesity rehabilitation, it is not only possible to get rid of excess weight, but also to treat comorbidities. It is aimed to improve the general health of the person with smart exercise, massage, etc. applications, especially disorders in the musculoskeletal system.
In obesity rehabilitation, treatment is planned by taking into account the age, weight and general health status of the person. A full comprehensive therapy program is developed by including a diet and exercise specialist. Smart exercise tools enable the patient to exercise more easily and consistently.
With full compliance with the diet and exercise program, the patient can lose an average of 4 or 5 kilograms per month. The obesity rehabilitation process is completed by bringing the patient’s body mass index to normal levels. From the first month, the patient participates in the program with greater enthusiasm with the advantage of losing weight and having healthy muscles.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What are Muscle Diseases?

Muscle diseases (myopathies) are diseases that disrupt the structure or functioning of muscle cells, the units of muscle tissue that provide movement. They can occur at any age, from infancy to old age.
There are many types of muscle disease and many subtypes. Variables such as the genes that cause the disease, the muscles affected, the age at which symptoms first appear, and the rate of disease progression are used to determine these types.
Today, there are around 500 muscle diseases that have been identified and recognized but whose exact cause remains unexplained. The majority of muscle diseases are inherited, that is, hereditary. In this case, a genetic defect in a person’s constitution disrupts the structure or function of the muscle cell. Inherited muscle diseases mostly affect infants, children or adolescents and most of them have no known treatment. A very small proportion are acquired, later-developing muscle diseases.
What are the Symptoms of Muscle Disease?
In most muscle diseases, symptoms begin to appear in childhood or adolescence-teenage years.
Common symptoms
- Difficulty walking, frequent falls
- Weak muscles, muscle thinning
- Muscle cramps
- Difficulty standing up, climbing stairs, running or jumping
- Walking on tiptoes
- Falling and sagging eyelids
- Respiratory or swallowing distress
- Vision problems, double vision
- Weakness in facial muscles, mimic and chewing muscles
What are the Diagnostic Methods for Muscle Disease?
For the diagnosis, your doctor first performs a physical examination. Muscle strength, reflexes and coordination tests help to rule out other diseases related to the nervous system. The patient’s family medical history is then questioned in detail. Common investigations for diagnosis:
Blood tests: In muscle diseases caused by muscle breakdown, detailed blood tests such as the level of muscle breakdown enzymes (such as CK, CK-MB, AST, ALT), blood count, blood electrolyte levels are performed.
Electromyography or EMG: The electrical activity of the nerves in the arms and legs is measured. A needle electrode is used to examine the images of the muscles during contraction and relaxation.
Muscle biopsy: A small piece of muscle tissue is taken. This is examined in the laboratory to determine which proteins are missing or damaged. It helps to determine the type of muscle disease.
Electrocardiogram or ECG: Measures electrical signals from the heart and determines how fast the heart beats and whether it has a healthy rhythm.
Other imaging techniques: Imaging methods such as MRI and ultrasound, which show the quality and quantity of muscle in the body, can also be used to diagnose muscle diseases.
Genetic screening tests: Finding the genes that cause muscle disease. Genetic tests are not only helpful in diagnosis, but are also important for people who are planning to start a family or have a family history of the disease. Discussing the meaning of genetic test results with a specialist doctor or genetic counselor is of great importance for the health of the children to be born.
What are the Treatment Methods for Muscle Disease?
There is no definitive treatment for muscle diseases. Treatments that can reduce symptoms and improve the patient’s quality of life are applied.
Physical Therapy: Different exercises are used to keep the muscles strong and flexible.
Speech therapy: Patients with weak tongue and facial muscles can be taught easier ways to speak with speech therapy.
Respiratory therapy: Patients who have difficulty breathing due to muscle weakness are shown how to make breathing easier or how to use respiratory support machines.
Medicines that suppress the body’s immune system: Drugs in this group can slow down the damage to muscle cells.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Cardiac Rehabilitation?

Cardiovascular diseases are the leading cause of death in the world and in our country. Prevention and treatment of such an important health problem is of utmost importance. Almost all cardiac diseases require a rehabilitation program in a certain period.
Cardiac rehabilitation aims to optimize the physical, social, emotional and occupational well-being of individuals with cardiovascular system diseases. With the cardiac rehabilitation program, we try to ensure that he/she can continue his/her life actively despite his/her existing disease and improve his/her quality of life.
Which patients are included in the Cardiac Rehabilitation Program?
- After MI (heart attack)
- After cardiac surgery (stent, bypass operation)
- Heart valve disease
- Heart failure
- Other cardiac conditions (arrhythmia, pacemaker, angina)
- Risk conditions for heart disease (hypertension, diabetes mellitus, obesity)
How is Cardiac Rehabilitation Planned?
Cardiac rehabilitation is the work of a team including a physical medicine and rehabilitation specialist, cardiologist, physiotherapist, dietician, nurse and psychologist. When planning the program, the patient is first informed about his/her disease, evaluated in detail, risk factors related to heart disease are determined, musculoskeletal system examination is performed, and an exercise test is performed to determine exercise capacity. The aim is to create and execute a patient-specific, appropriate, effective and safe exercise program.
What is done in the Cardiac Rehabilitation Program?
This program can be carried out in the hospital, at home or in the gym depending on the patient’s characteristics and disease. An exercise program is created based on the detailed evaluation and exercise test. Vital signs (pulse, blood pressure, oxygen saturation, ECG), breathing and fatigue are checked and the patient is taken into an exercise program on a bicycle or treadmill. In order to strengthen the muscles, different exercise programs such as physical therapy methods, strengthening and balance, breathing exercises, in-water exercise program are included in the program 3-5 days a week. Afterwards (after 4-8 weeks), it is recommended to continue the habits gained during the exercise period at home and in the gym.
What are the Benefits of Cardiac Rehabilitation Program?
With the cardiac rehabilitation program, the individual’s endurance (endurance) increases, lung capacity increases, fatigue decreases, breathing improves, he/she can walk longer distances and climb stairs more easily. As a result, the quality of life improves, anxiety decreases, sleep is restored and the person can return to his/her profession. There are direct positive effects on the heart (improvement of the endothelium, stabilization of plaques) and blood pressure (blood pressure) is regulated.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Joint Calcification
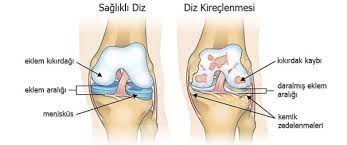
Knee, Shoulder and Hip Osteoarthritis can cause serious problems if not diagnosed and treated in advance. The hip joint is one of the largest and most important joints of the body. As each hip joint has to carry half of the body weight, this load increases even more during movements such as walking, running, climbing stairs, squatting and can increase up to several times the body weight. For this reason, some congenital or acquired disorders in the hip joints can cause serious problems later on, even if they are not recognized at an early stage.
Causes of Calcification
Congenital hip dislocation is the most important condition that occurs in the hip joint in early childhood. If this condition is not treated in time, it causes significant lameness with pain and difficulty in movement in the hip at an advanced age.
Rheumatic Diseases
Inflammatory or degenerative rheumatic diseases cause structural deterioration in the hip joint. Calcification of the hip joint is the most common cause of pain in adulthood.
Infections
Germs that spread from another part of the body or that come directly into the body can cause inflammation of the hip joint.
Tumors
Breast, lung and prostate cancers can spread to the hip joint and cause severe hip pain.
Vascular Causes
Hip pain can occur as a result of blockage of the blood vessels supplying the hip bones or impaired blood flow to them. In the cases listed above, it is first necessary to determine the cause of the pain. For this purpose, various imaging methods are used after a detailed clinical examination. The most commonly used imaging methods are classical X-rays, ultrasound, computer tomography and MRI.
Treatment After the cause of hip pain has been determined, treatment is initiated accordingly. Some patients require medication. After the acute phase of the disease has passed or following hip surgery, physical therapy and rehabilitation should be started. In appropriate patients, the recovery period is accelerated by having in-pool walking training together with exercise treatments.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Fracture Rehabilitation

The number of bones in an adult human is known to be approximately 206. Our bones have tasks such as providing movement through organs, keeping the body upright and protecting organs. Our bones, which have an important place in our daily activities, also have a fragile structure. Over time, we may face situations such as fractures and cracks in the bones with various effects such as falls and bumps.
The first important step of fracture treatment is completed by orthopedists and immobilization may be required during the healing period depending on the location of the fracture. Problems such as joint stiffness and muscle atrophy may occur due to immobilization, and the aim of fracture rehabilitation at this stage is to restore functionality.
Physical therapy should be started as early as possible during the immobilized period to dissipate edema, maintain range of motion, muscle strength and dexterity. The aim of the early rehabilitation program is to prevent scar formation, atrophy, contractures and adhesions, and to preserve the slippage of tendons and the length of muscle fibers. The aim of this program is to restore the joints affected by immobility to their former functional capacity as soon as possible. The early rehabilitation program aims to prevent scar formation, atrophy, contracture and adhesions, and to preserve the length of the tendons and muscle fibers. On the other hand, if the resorption of edema is prolonged until the healing process of the bone, soft tissue adhesions may develop and these adhesions may cause stiffness in the tissue of the person, causing pain and limiting movement. Unfortunately, it is a common practice to refer the patient to rehabilitation 2 months or much longer after the event, resulting in painful movement, muscle atrophy, contractures. Rehabilitation aims to prevent all these, adhesions, and to preserve the sliding of tendons and the length of muscle fibers. The treatment in this late period is different from the other one, and the main goals of the treatment are to maintain muscle dexterity, increase muscle strength, restore circulation, widen the range of motion of the joints, soften the fibrous tissue and eliminate the edema that still exists.
Basic Applications in Fracture Rehabilitation:
- Heat Application: They are applied to soften fibrous adhesions, increase circulation and reduce pain and spasm. Hot packs, paraffin, infrared lamps, hydrotherapy and hot springs can be used in fracture rehabilitation.
- Electrotherapy: TENS and other low frequency currents are effective in controlling pain. Ultrasound and short wave diathermy deep heating conversion modalities increase collagen stretchability. Therefore, they are applied before stretching exercises in post-fracture contractures.
- Exercise Program: In soft tissue rehabilitation, maintaining and increasing the range of motion and muscle strengthening are seen as the basic principles. Mainly 3 types of exercises are performed for these purposes: These are isometric exercise, isotonic exercise and isokinetic exercise. Since isometric exercises do not cause movement in the joint, they are applied from the early period after fracture reduction is achieved. Since isometric exercises cause more increase in maximal strength and isokinetic exercises cause more increase in total work capacity, the combined use of these two methods is more beneficial. An exercise program that will last for months should be organized so that it can be continued at home after hospitalization. Walking training is given especially in lower extremity fractures.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is acupuncture?

Acupuncture is an effective, scientific treatment method used in the treatment of many diseases, applied by inserting sterile hair-thick fine needles into important points determined on the body. Its foundations were laid in the Chinese-Uyghur region about 5000 years ago, the points and method used have come to the present day in almost the same way, in addition, microsystems such as the ear and hand have been developed over time, and today it has started to be used at increasing rates. In our country, it is only allowed to be applied by doctors certified by the Ministry of Health. Side effects such as local infection, foreign body reaction, sudden blood pressure change can be seen, but these risks become minimal in skilled hands.
Its almost side-effect-free, examination approaches that give the patient the chance to touch the patient, believing that the disorders concern the whole body and looking at the patient with a holistic approach are important advantages. With this point of view, we use acupuncture treatment as a powerful weapon that strengthens our hand while trying to heal patients who apply to us in many disorders, especially pain.
How does acupuncture work?
We know that acupuncture works, but we would not be wrong if we say that we do not yet know how it works. The main problem in solving the mechanism of action is probably due to the fact that we are trying to understand the mechanism of action of acupuncture from the perspective of modern science, that is, the observable science that Newton laid the foundations of. However, acupuncture argues that there is an unobservable energetic balance in the body and that most of the disorders are caused by deviations in this balance. It believes that when this disturbed body balance is restored, disease relief occurs. It is likely that the understanding of Quantum physics will increase support for the mechanism of action of acupuncture.
However, in many studies supported by modern medicine and science, it has been found that acupuncture releases endogenous painkillers such as endorphins through the nervous system, as well as causing positive changes in the level of hormones, increasing local blood flow, strengthening the immune system, and providing muscle relaxation. In other words, we can say that it uses the body’s own healing and medication mechanisms at the bioelectrical level.
How is acupuncture applied?
After a detailed examination, appropriate point combinations are selected according to the disease or discomfort detected. Sterile thin needles between 1 and 4 cm are inserted into these selected points. The needles are kept at the point where they are inserted for approximately 20 to 60 minutes. The most important point here is the point selection and then the correct application technique. Laser, electroacupuncture and local heating agents called moxa can be used as different techniques. Slight pain may be felt when the needle is inserted, but there is no pain during the session.
Which diseases is acupuncture used to treat?
It is frequently used in our hospitals for pain treatment. Used in more than 100 diseases and more popular in weight loss and smoking cessation treatments, acupuncture is also very effective in pain treatment. Especially in widespread waist, neck and back pain, pain in which one side of the body is completely affected, pain that cannot be found, pain that spreads to the head are the areas of use that we receive the most applications in the clinic. In addition to situations that create negative energy such as anxiety, fear, stress, lack of self-confidence, perfectionism, it accepts external factors such as cold, hot, humid air as the cause of disease and according to the philosophy of acupuncture, it is accepted that disorders occur when the harmony of the energy circulating in the channels that we cannot see in our body is disrupted. In the treatment, the current in these channels is regulated.
It is applied in our hospital in the treatment of low back and neck pain, facial paralysis, sleep and digestive problems, diseases such as fibromyalgia and irritable bowel syndrome where many symptoms are seen together, and restless leg syndrome. In addition, we also use it in weight loss and smoking cessation treatments.
How to lose weight with acupuncture?
In weekly sessions, an average of 1-2 kilograms can be lost with acupuncture. In the sessions, body acupuncture is applied first and lasts an average of 30 minutes, then permanent small needles are placed in the ear to stay for a week. With these needles, the satiety center is stimulated and the stress that may occur is reduced. In this process, the patient is recommended a suitable diet program and exercise together. It is known that acupuncture treatment ensures that the diet is comfortable, accelerates metabolism, suppresses the excess stress and appetite that normally occurs while dieting, and it is believed to show its effect in this way. Other treatments in the treatment of patients with arthritis, especially in the knee waist and neck areas, where we want them to lose absolute weight, can make the effect last longer and even permanently remove the excess load on the joints.
How to quit smoking with acupuncture?
Again, as in weight gain treatment, it is done by applying ear acupuncture together with body acupuncture. It may take an average of 7 sessions. It reduces the withdrawal symptoms and stress that occur when smoking is quit, suppresses the desire to drink and hand habit.
Weight and smoking addiction that disrupts the holistic health of the body will definitely cause pain in the long term. Therefore, acupuncture treatment is useful in preventing these problems and provides the opportunity to treat the cause of the disease, not the complaint.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Pulmonary Rehabilitation?

Pulmonary rehabilitation is all of the studies carried out to enable the individual to maintain his/her life as close to normal as possible despite the existing lung disease. Any patient with chronic respiratory disease who has shortness of breath, decreased exercise tolerance or restriction in activities of daily living despite adequate medical treatment can be included in the pulmonary rehabilitation program. Patients with chronic respiratory failure such as COPD (chronic obstructive pulmonary disease), asthma, cystic fibrosis, bronchiectasis, interstitial diseases, neuromuscular diseases (amyotrophic lateral sclerosis, spinal cord injury, spinal muscular atrophies), thoracic cage disorders and patients in the period of separation from the respiratory device can be included. Patients can also be enrolled in a pulmonary rehabilitation program before and after lung surgery. Pulmonary Rehabilitation, which is now accepted as a standard component of the medical treatment of chronic respiratory diseases, is a comprehensive set of practices that includes approaches such as exercise training, behavior change and patient education, which are individually determined following patient assessment, aiming to improve the physical and psychological conditions of chronic respiratory patients and improve health.
What is the Purpose of Pulmonary Rehabilitation Program?
Reducing symptoms and disease-related complications
To enable the patient to use his/her capacity in activities of daily living
Improving exercise tolerance
Ensuring self-confidence and independence
Reducing psychosocial symptoms (anxiety, depression)
Reducing hospital admission and length of stay
Ensuring return to work
Which Patients Can Receive Pulmonary Rehabilitation Program?
Pulmonary rehabilitation can be applied to all respiratory patients with persistent shortness of breath, restriction in activities of daily living, decreased quality of life and/or restricted exercise capacity. Pulmonary rehabilitation can be applied to respiratory patients of all ages in hospital, outpatient or at home, depending on the characteristics of the rehabilitation units. Pulmonary rehabilitation program can be successfully applied in COPD (chronic obstructive pulmonary disease), asthma, bronchiectasis, interstitial lung diseases, cystic fibrosis, chest wall diseases, neuromuscular diseases, before and after lung transplantation, lung cancer, obesity-related lung diseases.
How is Pulmonary Rehabilitation Planned?
Pulmonary rehabilitation is a teamwork of physicians, physiotherapists, dieticians, psychologists, occupational therapists, nurses and speech therapists. Patients are evaluated in detail, some laboratory tests (hemogram, blood gases…), pulmonary function tests, ECG and ergospirometric exercise test are performed. According to the findings obtained after these evaluations, an individual program is drawn for the treatment of problematic areas.
What is done in Pulmonary Rehabilitation Program?
- Patient education and smoking cessation work
- Bronchial hygiene techniques and controlled breathing techniques
- Exercise programs
- Oxygen support
- Diet planning
- Psychosocial support
What should be the duration of a pulmonary rehabilitation program?
Pulmonary rehabilitation program should be implemented for at least 8 weeks (24 sessions in total). Exercise habits should be maintained as gains are lost when exercise training is stopped. Patient education and smoking cessation, bronchial hygiene techniques and controlled breathing techniques, individualized exercise programs, diet planning, psychosocial support can be provided. These programs are planned for 8-12 weeks, at least 3 days a week, with each session lasting 1-2 hours on average. Patients can be admitted to the program as inpatients or outpatients.
Why is exercise necessary in respiratory diseases?
Patients with chronic respiratory problems with shortness of breath can exercise safely with pulmonary rehabilitation programs. In chronic lung disease patients, inactivity in daily life caused by shortness of breath and/or fatigue leads to a progressive decrease in bone and muscle content, heart and lung function and mobility. With exercise, muscle strength increases, muscle endurance increases, longer distances can be walked, muscles and joints move better, relaxation is achieved, feeling stronger and more energetic, heart function improves, and shortness of breath decreases.
What exercises are performed in pulmonary rehabilitation?
Respiratory exercise programs include strengthening and endurance exercises for both upper and lower extremities. Strengthening exercises are more important in patients with significant muscle atrophy or weakness. With devices such as IMT and PEP, respiratory muscles are strengthened and secretions accumulated in the bronchi are removed.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is hydrotherapy?

Hydrotherapy is a physical therapy and rehabilitation practice, also known as in-water therapy or pool rehabilitation. With the effect of the buoyancy of the water, it carries 10% of the person’s actual weight. This prevents the person’s muscles from being overloaded and movements are easier. Patients who do not load on the joints can easily use their joints thanks to the buoyancy and perform their exercises more painlessly and actively.
What are the benefits of hydrotherapy?
With the effect of the buoyancy of the water, the load due to the body weight of the person is reduced and movements that are normally difficult or painful to perform can be performed. When the load on the joints and muscles is reduced, patients can perform their exercises more painlessly and actively. In addition, due to the softening and relaxing effects of hot water on joints, soft tissues and muscles, it has positive effects on excessive muscle contractions, cramps, pain and joint stiffness. It helps to increase the strength and endurance of the muscles by using the resistance feature of the water. Hydrotherapy is also used in the treatment of edema and circulatory disorders due to its stimulating effects on the circulatory and lymphatic system. The patient’s morale, motivation and self-confidence increase as they are able to accomplish movements and activities that they normally cannot do and perform their exercises in an easier and more enjoyable way.
What are hydrotherapy methods?
Hydrotherapy can be applied in different ways. There are application methods such as in-pool exercise therapy, sitting bath, hot water baths combined with aromatherapy, steam room, contrast (hot/cold) bath applications, shower applications.
In which diseases is hydrotherapy applied?
Hydrotherapy is effectively used in the treatment of neurological disorders such as stroke, spinal cord injury, traumatic brain injury, cerebral palsy, multiple sclerosis, Parkinson’s disease, Guillain-Barre Syndrome, muscular dystrophies and balance disorders. Hydrotherapy is also used in the rehabilitation of musculoskeletal and sports injuries, fractures, arthritis, fibromyalgia, osteoporosis and obesity, and rehabilitation after prosthesis and other orthopedic operations.
In which cases is hydrotherapy contraindicated?
Hydrotherapy is not recommended in cases of fever, active infection, open wounds, uncontrolled epilepsy, severe respiratory and cardiac problems and allergies to in-pool chemicals.
How is hydrotherapy applied?
In-pool exercise therapy, the most common use of hydrotherapy, is performed with the help of a trained and experienced hydrotherapist. The hydrotherapist enters the treatment pool with the patient and assists or supervises the patient’s exercises. The duration and frequency of the session is determined according to the patient’s condition or needs.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Spina Bifida?

Spina bifida is a congenital anomaly that occurs when the spinal cord and vertebral column do not close during the fetal period. It is the second most common cause of disability in childhood. It is one of the most complex congenital anomalies that can be encountered in human life. It is a complex syndrome affecting the musculoskeletal and genitourinary systems. The frequency is 1-2 per 1000. Folic acid use can reduce this incidence by approximately 70%.
It is a closure defect of the spinal cord and spine in the first weeks of embryonic life. The terms myelomeningocele, spina bifida, spina bifida cisitica and myelodysplasia are used synonymously. The defect is usually recognized at birth by the presence of an external sac in the back or lumbar region. The sac usually contains structures related to the spinal cord. Although the defect can occur at any level of the spine, it is most common in the lumbar region.
What are the Clinical Types of Spina Bifida?
- A) Spina Bifida Sistica
It is the cystic form of spina bifida. There are three types: meningocele, myelomeningocele and myeloschisis.
- Meningocele is a cystic enlargement. The defect is covered with skin, neurological structures are within the canal and neurological damage may be absent because they are not damaged much.
- Myelomeningocele is a herniated sac containing the spinal cord membranes, nerve roots and the spinal cord itself. It is the most important and most common type of spina bifida. Neurological problems are common. When the baby is born, it should be referred to surgery and the defect should be closed.
- Without myelosia; It is the most severe form, the nerve tissue is completely exposed.
- B) Spina Bifida Oculta
It is a bone defect only in the posterior part of the spine without involvement of the spinal cord. There may be a dermal pit, hair bundle or increased pigmentation in the sacral region. It can occur in many healthy people.
What are the Risk Factors for Spina Bifida?
Although there are many risk factors, the exact cause is not clear. Normal prenatal development of the neural tube starts on day 16 and is completed on day 28. Closing defects occur during this period. In other words, the defect is formed before the mother knows she is pregnant.
- Folate deficiency, increasing maternal folate levels significantly reduced the occurrence and recurrence of neural tube defects.
- Vitamin B12 deficiency
- Maternal age; common in mothers over the age of 40 and under the age of 19
- Genetics
- Exposure to toxic substances, especially pesticides
- The mother’s high body temperature during pregnancy, excessive heat in the first trimester of pregnancy should be avoided.
- Excessive coffee consumption, especially in the year before pregnancy, but caffeinated tea has a protective effect.
- Drugs; methotrexate, trimethoprine, sulfonamides, antidepressants, antiepileptics
- High risk in women with pregestational diabetes
- Obesity
What are the Clinical Symptoms?
- Loss of strength in the arms or legs, paralysis depending on the area involved
- Flaccid or spastic paralysis
- Sensory loss
- Hydrocephalus
- Taut cord
- Neurogenic bladder and bowel
- Scoliosis
- Hip dislocation, hip and knee contractures, foot deformities
- Injuries
- Obesity, short stature, early puberty
- Increased risk of osteoporosis accompanied by fractures
- Severe impairments in visual perceptual skills, attention
- Sexual dysfunction and fertility
- Increased frequency of depression
- High latex allergy
What is involved in the treatment of Spina Bifida?
Prenatal treatment
Maternal serum alphaprotein (AFP) and detailed USG are commonly used to determine the presence or possibility of fetal spina bifida. Serum AFP is measured 16-18 weeks after fertilization. Detailed USG can reveal the presence of spina bifida at 14-16 weeks of gestation. If the diagnosis of spina bifida is confirmed, the pregnancy can be terminated or families who do not terminate their pregnancy are prepared for a safe delivery. Such babies should be delivered by cesarean section in a comprehensive center.
Neonatal Treatment
First of all, the defect should be closed within the first 48 hours after birth to reduce the risk of infection and to preserve the existing neurological function. A shunt may be required in patients with hydrocephalus. Most patients have a neurogenic bladder. Urological and nephrological treatment should be started immediately after birth to prevent kidney damage.
What is done in Spina Bifida Rehabilitation?
Early rehabilitation includes bladder and bowel care, prevention of contracture, hip dislocation and spinal deformity, normal walking with orthoses and wheelchair use. Families are taught early on how to position, hold and transfer the baby, and range of motion exercises for those with hip and knee contractures. Rehabilitation should be done according to the level of lesion, the age of the child and accompanying problems.
What are the Common Problems in Spina Bifida?
Hip Problems and Treatment: Hip deformities in children are caused by weakness and imbalance of the muscles around the hip. If not treated properly, it can lead to pelvic tilt and later scoliosis. Surgery to correct hip deformities is mostly performed to correct hip contractures.
Scoliosis Treatment: Progressive scoliosis may be due to congenital spinal malformations, muscle imbalance and some neurologic disorders. Spinal orthosis and functional strengthening exercises may be given to correct sitting balance, control the curve during growth, and delay surgery in patients with scoliosis less than 50 degrees. Surgery for scoliosis is controversial. Surgery may improve sitting balance in those with limited sitting function.
Fractures Common in the lower extremities. They are frequently seen after falls in ambulatory patients. In those who cannot walk, it is mostly caused by bone resorption. Since there is no pain sensation, it may not be very noticeable. However, there may be erythema, swelling and local temperature increase. Fractures heal quickly in children with spina bifida. It should be treated with non-surgical methods.
How is walking in spina bifida?
The possibility of walking in children with spina bifida depends primarily on the level of lesion, severity of orthopedic deformities, cognitive functions, surgery, motivation, obesity and age. With appropriate support, surgery, rehabilitation and orthotics, many children with spina bifida can walk.
What are the Problems in Adult Patients with Spina Bifida?
- Pain is a common complaint. Especially back, neck and leg pain is observed. Shoulder and elbow pain is mostly due to overuse.
- Scoliosis does not progress after adolescence, but may cause posture and sitting disorders, pressure sores, loss of gait, respiratory dysfunction and pain
- Osteoporosis
- Increased neurological problems may develop as a result of shunt obstruction, stretching of the spinal cord
- Pressure sores, burns come as a result of sensory loss
- Kidney failure
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Nerve Compression

The impulses that allow us to move are transmitted from the brain and spinal cord to the relevant muscles via nerves. Nerves, which we can liken to a thin electrical cable, are responsible for the transmission of sensations as well as movement.
What is Nerve Compression?
Under normal conditions, all movements of the arms, legs, hands and feet occur perfectly and do not cause any complaints thanks to the harmonious functioning of sensation and movement; however, in some cases, the nerves to the muscles of the hands and feet are compressed while passing through thin channels and nerve compression may occur.
The most common nerve compression is known as “Carpal Tunnel Syndrome” and affects the wrist and fingers.
This condition, which occurs when the median nerve to the first four fingers of the hand is pinched at the wrist level, is common in people who use their hands a lot due to their profession and housewives.
What are the Symptoms of Nerve Compression?
The most important symptom is hand numbness that wakes you up at night. Sometimes there may also be pain, but numbness is usually in the foreground; patients state that they feel relieved when they shake their hands. These complaints recur during the day and over time, the strength of the fingers decreases and the objects held in the hand begin to fall. A similar condition develops in the ankle and toes, especially in those who wear shoes with pointed toes, high heels and work in heavy jobs, and is called “Tarsal Tunnel Syndrome”. Similar complaints occur in the ankle and toes.
How is nerve compression treated?
In both nerve compression disorders, a definitive diagnosis must first be made. After the initial examination, nerve conduction should be measured with a sensitive system called EMG. As a result of this examination, physical therapy methods are used together with medical treatments in cases that are not very advanced and have not yet developed loss of strength. A suitable splint is given to rest the hand and in some cases injection therapy may be applied. Physical therapy is used to relax the pinched nerve and accelerate its recovery.
The most commonly used physical therapy tools include water therapy, ultrasound, paraffin, laser and magnetic field treatments. Afterwards, appropriate exercises are used to strengthen the muscles and increase elasticity. In advanced cases, surgical methods are used. Surgery is performed on the wrist or ankle to relieve the passage of the nerve. After the surgery, a physical therapy and rehabilitation program of 15 to 20 sessions is applied to relieve joint stiffness and strengthen the muscles. Then, in order to prevent recurrence of the same condition, occupational factors are tried to be corrected, and training and exercises are performed to correct errors in the use of the hand and foot.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is osteopathy?

Osteopathy comes from the Greek “osteon” (bone) and “pathos” (suffering). “In fact, osteopathy aims at and defines the well-being of the whole body. Osteopathy, a natural treatment method, has been recognized as a scientific treatment by the World Health Organization. Osteopathy can be applied in the diagnosis and treatment of diseases. It is a method applied using hands. Osteopathy is applied under 3 main headings: Parietal osteopathy which regulates the rhythm of the musculoskeletal system, visceral osteopathy which regulates the relationship between the internal organs and the vegetative nervous system, and cranial osteopathy which regulates the flow of fluid in the brain and spinal cord. Osteopathy focuses on treating causes rather than effects. It aims to find the cause that started the complaint. In other words, it treats shoulder pain and limitation after a foot sprain from the top of the foot.
How is osteopathy applied?
Osteopathy is a manual treatment method according to the diagnosis made by trained physicians after the osteopathic examination. The body is allowed to treat itself with maneuvers performed without the use of drugs or anything medical.
What is the logic of osteopathy?
Osteopathy is a method developed by Dr. Andrew Taylor Still. “Still believed that any disorder, even if not recognized at first, was the result of another existing disorder in the body. This belief is the fundamental basis of holistic treatments today. For example, a problem with a ligament that allows the small intestine to hang from the body can cause you to have a stiff lower back when wearing socks. Or your leg muscles may shorten due to wearing high heels and you may experience headaches that do not respond to treatment with fascia connections. As a solution, you can treat the headache with exercises that lengthen your leg muscles. If you are in a draft and your body is tilted to one side, you have a spasm in your psoas muscle. You can correct this with a simple osteopathic psoas massage.
In which diseases is osteopathy useful?
- Waist, neck, back pain and hernia
- Migraine and tension headaches,
- Posture disorders such as scoliosis, kyphosis
- Elimination of postoperative pain and adhesions
- In chronic fatigue, sleep disorders
- In sports injuries,
- Circulatory problems (blood and lymphatic system)
- Impaired gait, balance and coordination
- Fibromyalgia syndrome
- Arthrosic changes such as joint stiffness, calcification
- Joint blockages, spine and costa blockages,
- Visceral osteopathy is used as supportive treatment for constipation, diarrhea, incontinence, indigestion, gas, abdominal pain, spastic colon, ptosis and dysfunction of the digestive organs.
- Cranio-sacral osteopathy can be used in swallowing, vomiting and head deformity in infants.
- Allergic and chronic diseases,
- Acute pain
At what intervals is osteopathic treatment performed?
Osteopathic treatment is planned according to the patient and the treatment of the disease. It is usually done once a week. In between treatments, the patient is advised on exercise and proper nutrition.
Are there any side effects of osteopathy?
Osteopathy is a very gentle treatment and has no side effects when applied correctly. Pregnant women can be safely treated with craniosacral osteopathic techniques for low back pain.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Neck Pain

Neck pain is a very common health problem and can occur in people of all sexes and ages. Although neck pain is less common than low back pain, neck pain occurs in one third of the population. Most of them are mild and heal spontaneously in a short time. Rarely, it can be very painful or even severe enough to cause disability.
Neck pain can also radiate to the back of the head, around the shoulders, arms and anterior chest. Neck pain may be accompanied by numbness in the arm and hand, dizziness, imbalance and headache.
The incidence of neck pain increases with age. Tensions in daily life and work stress increase neck pain. It has been found that there is a relationship between neck pain and the patient’s job. Pain is more common in those who work at work. Working in a fixed position for a long time (desk workers, assembly workers, musicians) also increases neck pain.
In most acute neck pain, no specific cause can be found, but mechanical causes dominate in 95% of cases.
Causes of neck pain;
1-Connected to bone structures
- Congenital Torticollis, Klippel-Feil syndrome
- Traumatic Fractures, slips, hernias
- Calcifications, canal stenosis
- Rheumatic: Ankylosing spondylitis, rheumatoid arthritis, polymyositis, polymyalgia rheumatica
- Tumors
- Infections
2-Connected to soft tissues
- Posture disorders
- Fibromyalgia and myofascial pain syndrome
- Nerve and vascular problems
3-Reflected pain
4-Endocrinological and metabolic
- Osteoporosis
- Parathyroid disease
- Paget disease
4-Psychological
How are neck pains classified according to duration?
1-Acute: lasts less than 1 month.
2-Subacute: lasts between 1-3 months.
3-Chronic: lasts longer than 3 months.
History of neck pain
History is as important as physical examination in neck pain. A careful and chronological history should be taken and pain should be questioned in detail. It should also include traumas (physical and psychological) and operations, habits, family history, social status, work and hobbies.
Mechanical neck pain increases with physical activity, decreases with rest and warmth, and is short-lived even if there is morning stiffness. Rheumatic pain increases with longer rest, is relieved by light physical activity and is associated with morning stiffness of more than 1 hour. Cancer pains start insidiously, increase at night, and do not decrease with medication, even if they are relieved by getting up and moving.
A physical examination is performed by the physician. During the physical examination, the patient’s posture and neck are examined, soft tissues are checked, and how much the patient can move his/her neck is evaluated. In addition, special stimulating maneuvers and neurological evaluation are performed if there are signs of nerve compression.
What are the diagnostic methods in neck pain?
- The probability of identifying the cause of neck pain does not exceed 20% in the 20-50s and 12-15% in all ages. Therefore, in the majority of cases, auxiliary examination methods are not needed during the initial evaluation.
- Infections, rheumatic problems, cancers, common diseases of the bone should be subjected to laboratory examinations.
- EMG and nerve conduction studies
- It is most commonly performed in cases with neck pain in the possibility of nerve root compression. It shows which nerve root is compressed and its severity and differentiates diseases involving the muscular and nervous system.
- Imaging methods
- It is important to remember that none of the more advanced diagnostic examinations such as radiography, CT, MRI, EMG or bone scintigraphy can replace the history and physical examination in patients with neck pain and that treatment should be planned according to the complaints of the patients, not according to the results of these examinations.
In which cases should imaging examinations be performed?
- Advanced age
- Recent trauma
- Prolonged cortisone use
- Presence of cancer
- Presence of infection
- Fever
- 10% weight loss within 6 months
- Presence of intractable pain
- Neurological symptoms
What are the principles of treatment for neck pain?
The first step in treatment is to relieve the pain and reduce the spasm to break the vicious cycle of pain-spasm-pain in order to relieve the patient, to take measures to prevent recurrence and to correct biomechanics. The main methods used in treatment are as follows:
Bed rest and cervical collar
The patient should first be informed about the possible causes of his/her pain and educated about his/her disease. It has been found that resting for 2-3 days in acute pain and 7 days in radicular pain is sufficient and resting for more than 1 week leads to decreased movement in the joints, soft tissue shortening, and decreased muscle strength and cardiovascular fitness. Therefore, activity modifications should be made instead of bed rest in acute neck pain.
The use of cervical collars should be used for a short period of time and should not exceed 1.5 months in non-traumatic acute neck pain. In long-term use, exercises should definitely be performed as loss of strength and volume may occur in the neck muscles.
Drug Treatment
What are the aims of drug treatment?
- Reducing pain
- Increase physical function and movement
- Restoring sleep patterns disturbed by pain and other complaints
- Restoring social life disrupted by pain and discomfort
- Prevent work loss due to pain and physical disability
- Tackling pain-related anxiety, tension and depression
- Painkillers, muscle relaxants, antidepressants, corticosteroids, corticosteroids, antiepileptics can be used for neck pain depending on the patient’s condition and the patient.
Physical Therapy applications
Physical therapy sessions and exercise programs, which occupy the most important place in treatment, have been used for many years because they reduce complaints and can be applied safely.
In physical therapy, heat application, currents to reduce pain such as TENS or interference, ultrasound, laser, hiltherapy, traction, cupping, massage, taping, dry needling, trigger point injections, mobilization and manipulation applications can be performed.
Exercises
What are the main goals of exercise for neck pain?
- Ensuring painless and full range of motion of neck and shoulder movements
- Ensuring full strength, endurance and balance of the muscles
- Preventing loss of physical function
- Avoiding repetition
- Ensuring physical harmony
- Facilitate the return of patients with chronic neck pain to a more productive life and improve quality of life
In the acute phase, exercises are aimed at reducing pain and protecting the damaged structures from further damage. In the subacute phase, it aims to restore the function of damaged and supporting structures. In the chronic phase, it aims to eliminate psychological problems in recovery and decrease in physical function.
Range of motion, stretching, strengthening, posture, coordination and aerobic conditioning exercises are beneficial in neck pain.
Spa treatment provides a decrease in pain threshold and muscle spasm and an increase in quality of life.
Is surgical treatment necessary?
Surgical treatment (surgery) is required in the following problems related to the neck.
- Cervical hernia compressing the spinal cord with progressive loss of muscle strength, sensation and reflexes
- Tumor or abscess in the spine
- Despite treatment, complaints persist for more than 3 months, are unbearable and impair quality of life
- Spinal fracture and severe spinal displacement
- In the presence of serious neurological problems due to spinal cord compression
Useful advice for people with neck pain
- Never lift, pull or push heavy objects. Divide the loads you carry equally between both hands.
- Do not carry loads with your head. Do not lift loads above head level.
- Never lift, pull or push heavy objects. Divide the loads you carry equally between both hands.
- Do not keep your neck constantly bent forward or fixed in the same position.
- Do not put the phone between your neck and shoulder while talking.
- When sitting, keep your back straight and lean back.
- If necessary, reinforce your neck with a neck pillow that fits your neck curve.
- Do not fall asleep with your neck hanging out of bed.
- Do not use excessively high pillows.
- Organize your working conditions and circumstances well.
- Change position every 30 minutes, especially at the computer and desk.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Pains

Shoulder pain is a common musculoskeletal problem. In the general population, shoulder pain ranks third after back and neck pain. Shoulder pain ranks first among the reasons for consulting a doctor, especially in people who work using their arms. One of the most important reasons why shoulder pain is common is that the shoulder joint is the most mobile and complex joint of the human body. Around the shoulder joint are soft tissues consisting of capsules, ligaments, tendons, bursae and muscles. It is mainly the soft tissues around the joint that provide a solid structure of the joint. In this case, soft tissue lesions are common in the shoulder.
What are the causes of shoulder pain?
The most common cause of shoulder pain is shoulder pain caused by the structures of the shoulder itself. Impingement syndrome involving the tendons of the shoulder and rotator sheath syndrome come first.
Frozen shoulder, tendinitis (bicipital tendinitis), calcific tendinitis caused by lime deposits on the tendons, osteoarthritis (calcification), shoulder laxity or semi-dislocations of the shoulder (subluxation), strain pain due to the muscles around the shoulder called myofascial pain syndrome are the most common problems. Shoulder pain can also be seen due to damage to the nerves of the muscles around the shoulder and weakness and weakness in the shoulder are more prominent. The shoulder is affected in most inflammatory rheumatic diseases (rheumatoid arthritis, spondyloarthropathy, polymyalgia rheumatica). In addition, tumoral disorders and infections originating from the bones and soft tissues in the shoulder area can also cause shoulder pain.
Less common causes are pain arising from structures outside the shoulder. Cancers of the upper part of the lung, liver, stomach, gall bladder, spleen problems, heart diseases can also cause shoulder pain. It should be kept in mind that neck hernias cause pain radiating to the shoulder, so the causes of neck pain can often be confused with the causes of shoulder pain.
What is impingement syndrome?
The most common cause of shoulder pain is impingement syndrome. Impingement syndrome occurs when the tendons of the muscles that allow us to lift our arm and the sac in this area are squeezed between the bone structures that make up the shoulder. It is more common in professions that use the hand up, housewives, and athletes who play sports such as swimming and volleyball. As a result, this problem is a disease of misuse or overuse of the shoulder. The importance of this syndrome is that if the necessary treatment and precautions are not taken, it can result in complete rupture of the tendons.
Complaints often occur as a result of using the shoulder and arm. Over time, the pain becomes constant. It turns into a pain that keeps the patient awake, especially at night. It reaches a level that affects the patient’s daily life activities such as dressing and undressing.
How is impingement syndrome treated?
In the early stages, cold application (ice packs) as well as painkillers and anti-rheumatic drugs are used. Injections to the shoulder (local anesthetic, steroid, ozone, mesotherapy) are important in reducing pain and regressing inflammation. Physical therapy and rehabilitation applications are extremely important in the treatment of impingement syndrome. Thermal modalities (hot application), electrotherapy (TENS, iontophoresis), ultrasound and high-intensity laser therapy (hiltherapy) and exercise programs accompanied by a physiotherapist are tried to be taken under control. At the end of this treatment program, it is very important to use the shoulder correctly and to continue shoulder strengthening exercises without causing impingement. Surgical intervention may be considered in patients who do not get sufficient results with preventive treatment methods.
What are Rotator Sheath Tears? What is the treatment?
Rotator sheath injuries are the most common injuries in the shoulder. Two types of tears, partial and full-thickness, have been described in rotator sheath tendons. The pathophysiology of rotator sheath tears is explained by intrinsic and extrinsic theories. Intrinsic causes include intrinsic avascularization, smoking, cholesterol and age-related degenerative changes. Extrinsic causes include subacromial impingement, repetitive activity, acromion structure and traumas. As a result of rotator sheath injury, a series of changes may occur in the tendon, starting with tendinosis and ending with a full-thickness tear. The frequency increases with age. In the older age group, some patients with full-thickness RC tears may be asymptomatic and more than 50% of individuals >70 years of age have a RC tear. Early diagnosis of rotator sheath lesions can not only facilitate the treatment program, but also reduce the patient’s quality of life due to pain and progressive limitation of movement. Treatment may include preventive (conservative treatments) and surgical treatments. Conservative treatments may include physical therapy applications, intra-articular injections (hyaluronic acid, ozone) and drug therapies.
What is frozen shoulder?
Adhesive capsulitis is a common cause of shoulder pain. It develops due to synovitis and capsular contraction in the shoulder joint. Along with widespread pain and tenderness in the shoulder, it restricts the movements of the shoulder joint in all planes. Shoulder pain severe enough to keep you awake, pain that makes it difficult to perform daily tasks, and difficulty in lifting or rotating the arm beyond a certain point. In advanced cases, they may have difficulty in performing daily functions such as personal hygiene and taking anything from the closet. Frozen shoulder is a disease that can last 2-3 years. It has three periods. The first is the painful period and can last up to 1 year. This period can often be confused with other shoulder and neck problems. The second period is the period when the shoulder is completely frozen. The pain decreases but shoulder movements are restricted to the extent that the patient cannot perform daily life activities. The third period is the thawing period.
How is frozen shoulder treated?
Treatment includes physical therapy modalities, manipulation and exercise, as well as medication and injections into the shoulder joint or soft tissues. Physical therapy modalities (heat applications, electrotherapy, ultrasound, hiltherapy) reduce pain and support the healing process. Appropriate exercise programs accompanied by a physiotherapist, exercises on exercise devices (cpm), exercises in water are used to open the shoulder joint movements and reuse the arm in daily life. Surgery can be applied in cases that do not improve with conservative treatments.
What is calcific tendonitis? How is its treatment planned?
It is a condition that causes severe pain in the shoulder. For an unknown reason, it is a condition caused by the collapse of crystals on the tendon, which we can call lime deposition in soft tissue. Shoulder pain starts suddenly and severely after a strenuous activity. It is usually diagnosed with X-rays. In the period of severe pain, in addition to drug treatment, ice application and injection applications to the calcific lesion have a very important place. In chronic cases, physical therapy rehabilitation programs in which ultrasound therapy is at the forefront are applied. There is also ESWT (shock wave therapy). In very resistant cases, surgical removal of these calcifications may be required.
What should be done if the shoulder is dislocated too often?
If a shoulder has recurrent dislocations without any trauma, these patients benefit greatly from physical therapy and rehabilitation programs that include strengthening of the appropriate muscles according to the direction of the dislocation. The first problem that should be considered in young patients and athletes with shoulder pain is the tendency to dislocation, which we call instability due to looseness of the ligaments in the shoulder.
What is osteoarthritis in the shoulder joint?
Since it is not a load-bearing joint, osteoarthritis in the shoulder joint is not as common as osteoarthritis in the knee joint. Pain and limitation of movement can be seen with the movement of the shoulder joint. Physical therapy applications, intra-articular injections (hyaluronic acid, ozone) and exercise programs are extremely important in the treatment.
How is shoulder pain evaluated? Which tests and imaging methods can be requested?
The majority of shoulder pain is caused by soft tissues. Magnetic resonance imaging (MRI) of the shoulder provides detailed analysis to evaluate the soft tissues and bone structures in the shoulder. X-rays may be requested in elderly patients where calcification is expected and in case of trauma. Tomography of the shoulder is less common, but may be ordered, especially in the evaluation of the detailed bone structure. EMG examination may be required in patients with nerve involvement, and blood tests may be ordered especially if rheumatic disease, infection or tumoral condition is suspected. Imaging related to other organ systems may be requested, especially if reflected pain is considered (ultrasound, ECG, echo, chest radiography).
What is the importance of physical therapy and rehabilitation in shoulder pain?
In most pathologies that cause shoulder pain, the main treatment is physical therapy and rehabilitation. In cases requiring surgery, physical therapy programs are included before and after surgery. In the long-term control of shoulder disorders, protecting the joint, avoiding strenuous activities and regular exercise are extremely important in preventing recurrence.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is neck flattening?
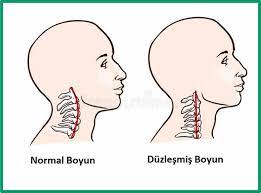
There are seven vertebrae in the neck. Normally they are arranged in a “C” shape. For various reasons, this alignment can turn into an “I” shape, or even an inverted “C” in advanced cases. This condition is defined as neck flattening.
What are the symptoms of neck flattening?
The most common symptom of neck flattening is neck pain. The pain may radiate to the back and shoulders. It may also be accompanied by headache. If there are also symptoms such as pain radiating to the arm, numbness, tingling, weakness, it is likely that there may be a neck hernia along with straightening. Dizziness, nausea and loss of balance may also accompany the pain.
What are the causes of neck flattening?
- Decreased physical activity
- Working long hours at a desk
- Sitting in front of a screen for long periods of time
- Wrong posture position
- Using computers and phones for a long time
Some diseases can also cause neck flattening:
- Degenerative disc disease (calcification)
- Due to previous neck surgeries
- Congenital disorders
Traumas - Tumors and infections
How is neck flattening diagnosed?
- X-ray: It gives good information about bone structure. However, it is not sufficient to evaluate soft tissues.
- Magnetic Resonance Imaging: In this examination, called MRI for short, radio waves can be used to examine many body tissues, including soft tissues.
- Computed Tomography (CT): X-rays from angles are used to create a 3-dimensional shape of tissues and organs in the body.
How is neck flattening treated?
In the treatment of neck flattening, it is very important that patients are sufficiently informed and aware. The habit of exercising should be established. Treatment methods such as superficial or deep heat applications, relaxation movements, electrotherapy, massage with certain medications, acupuncture, neural therapy, ozone applications, mesotherapy, electromagnetic therapy are also methods applied in cases of neck flattening.
Continuity of sportive activities such as yoga, pilates and swimming, which provide relaxation and strengthening of all body muscles, should be ensured.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Cruciate Ligament Injuries and Treatment

One of the most common knee injuries is a sprain or tear of the anterior cruciate ligament. Athletes who participate in high-performance sports such as soccer and basketball are more likely to damage their anterior cruciate ligament. If you have injured your anterior cruciate ligament, you may need surgery to regain full function of your knee. This will depend on several factors, such as the severity of your injury and your activity level.
The anterior cruciate ligament (ACL) is the ligament between the thigh bone and the shin bone. The anterior cruciate ligament is a pair of cruciate ligaments (the other is the posterior cruciate ligament) in the human knee. Because they are arranged in the shape of a cross, they are also called cruciate ligaments. The anterior cruciate ligament is one of the four main ligaments of the knee, and the anterior cruciate ligament provides 85% of the holding force at 30 degrees and 90 degrees of knee flexion. The anterior cruciate provides control of the leg. It prevents the leg from throwing itself forward uncontrollably and ensures correct gait.
What are the causes of anterior cruciate ligament injuries?
About half of all injuries to the anterior cruciate ligament damage the articular cartilage, meniscus or other ligaments in the knee. The main cause of cruciate ligament injuries is sprains. Anterior cruciate ligament injuries occur when the knee or leg is sprained while the foot is stationary. It can also occur after direct blows to the knee, sudden falls from a height and traffic accidents.
Sprains are classified according to severity:
- Grade 1 sprains: The ligament is slightly damaged but can still help stabilize the knee joint.
- Grade 2 sprains: This usually means that the ligament is partially torn.
- Grade 3 sprains: This is when the ligament is completely torn. The ligament is divided into two parts.
What are the symptoms of anterior cruciate ligament injuries?
- Different complications occur with anterior cruciate ligament injuries. These include:
- When moving, the knee feels and sounds like it is snapping.
- Locally, severe pain is felt in the knee and the whole leg.
- In anterior cruciate ligament ruptures, edema, bruising or redness may occur in the knee due to internal bleeding.
- Because of the edema, the mobility of the knee is reduced and it is difficult to move it.
- In anterior cruciate ligament injuries, difficulty in walking and temporary limp may be observed.
- Sudden numbness in the leg during walking prevents the leg from moving.
- In some cases, there may be a feeling that the knee is moving out of place.
What should be the first intervention in anterior cruciate ligament injuries?
Anterior cruciate ligament injuries are predominantly seen in athletes. A cruciate ligament injury, which occurs when the leg frees itself while the foot is on the ground, causes severe pain in the patient. If the patient realizes that they have an anterior cruciate ligament injury in their leg, it makes first aid easier.
An anterior cruciate ligament injury causes the sensation that something has snapped inside the leg. There is also severe pain and numbness in the leg. The patient may even feel as if the leg has been severed. If you have such complaints, the possibility of an anterior cruciate ligament injury is quite high.
The first thing to do in this case is to stop moving. The patient should be carried to the hospital on a stretcher or lap without stepping on the ground with his/her foot.
Cold compresses or elastic bandages can be applied to reduce pain in anterior cruciate ligament injuries.
In anterior cruciate ligament injuries, the swelling, pain or redness in the leg can be stopped in about 1 week without any treatment. You can then walk normally by stepping on the ground.
How are anterior cruciate ligament injuries diagnosed?
To diagnose anterior cruciate ligament injuries, the patient’s medical history is first listened to. At this point, it is very important that the patient can express the problem correctly. What the patient first felt at the time of the incident, whether there is a feeling of a rupture in the leg, whether his/her foot is free or not are factors that facilitate the diagnosis of the disease.
X-rays are then sufficient for a definitive diagnosis. If there is a rupture in the ligament between the thigh and tibia, it can be diagnosed with certainty.
How is Physical Therapy Performed in Anterior Cruciate Ligament Injuries?
Anterior cruciate ligament injuries are treated with physical therapy applications. In the first stage of the disease, physical therapy is not fully effective as there is significant edema and pain in the knee. In order to get full results, physical therapy applications may need to be continued for 10 to 15 days.
A more effective and intensive physical therapy plan is applied 15 days after the injury. Thus, the patient can participate in physical therapy applications much more effectively and recovery can be realized much faster.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is knee arthritis (gonarthrosis)?

Osteoarthritis (arthritis) is the wear and tear of weight-bearing joints due to aging. The knee is one of the most weight-bearing joints in the body and therefore one of the joints most affected by osteoarthritis. Calcification of the knee joint is called gonarthrosis. Calcification starts from the cartilage and affects the bone under the cartilage, the joint capsule and the ligaments around the joint. There is even thinning and hardening of muscles that cannot be used due to pain.
Who has knee arthritis (gonarthrosis)?
Knee arthritis (gonarthrosis) occurs in middle and older ages. It is more common in women over 50 years of age. The disease can also occur at an earlier age. Patients are usually overweight. Previous joint operations, traumas, sports injuries, inflammatory rheumatism, and some congenital disorders are the most important causes.
What are the symptoms of knee arthritis (gonarthrosis)?
The most important symptom is pain. The pain, which initially increases with the use of the joint and passes with rest, may become permanent as the disease progresses. Swelling, bone spurs and deformities appear in the joints. As the bone surfaces rub against each other, crunching sounds can be heard. The range of motion of the joints decreases and loss of function occurs in the affected joint.
How is knee arthritis (gonarthrosis) diagnosed?
Most of the time it can be diagnosed with a simple X-ray. In early cases of arthrosis, X-rays may be normal, in which case MRI (magnetic resonance imaging) may be useful.
What are the methods used in the treatment of knee arthritis (gonarthrosis)?
Various painkillers, glucosamine preparations, herbal support products can be used in the treatment of gonarthrosis. Viscosupplementation products such as hyaluronic acid can be injected into the knee to improve joint fluid quality, facilitate joint movements and relieve pain. Corticosteroid injections are an effective treatment during periods of exacerbation. Regenerative medicine modalities such as prolotherapy, mesotherapy, and stem cell therapy are recently emerging injection therapies.
The most important factor in the treatment of gonarthrosis is to avoid obesity. The abnormal loads created by excess weight on the joint cause irreversible damage to the cartilage tissue and lead to arthrosis at a much earlier age than expected. It is also very important to lose weight after the onset of the disease; by losing weight, the progression of the disease can be slowed down and symptoms reduced.
Regular and non-strenuous exercise is important for joint health. 20-30 minutes of low-intensity exercise 5 times a week is beneficial for both general health and joint health. Sports such as swimming, walking, cycling and golf can be practiced even at advanced ages.
How is physical therapy performed in knee arthritis?
Hot or cold applications, electrotherapy (TENS, electrical stimulation, etc.), ultrasound therapy, short wave therapy, personalized exercises are among the basic components of physical therapy.
Hot and cold applications; cold application is usually performed during the exacerbation period when edema is evident. Hot applications are preferred in chronic knee arthritis pain. Hot application can be done with methods such as hotpack and infrared.
Treatment with water (hydrotherapy): In-water exercises in treatment pools reduce the load on the joint with the help of the buoyancy of the water and make it easier to exercise. In addition to stretching, muscle strengthening, aerobic exercises, walking, stair climbing training can be started in the pool and as the patient’s condition improves, the patient can be transferred to a normal exercise room outside the water.
Manual therapy can reduce joint pain and stiffness, but it is more beneficial if combined with active exercise methods.
Although massage is not among the main treatments for osteoarthritis of the knee, it has muscle relaxant, muscle stimulating and joint stiffness reducing properties as a supportive treatment.
Electrotherapy is one of the important techniques used for the treatment of knee arthritis. Nerves and muscles are stimulated with electrical currents by electrodes attached to the skin. This is called transcutaneous electrical nerve stimulation. Pain sensation is reduced by stimulating the nerves. Electrical stimulation of the muscles can prevent muscle wasting.
In ultrasound therapy, deep tissues can be heated with the help of sound wave energy. Strong sound wave vibrations have effects other than heating. They have a modifying effect on the inflammatory process. It can reduce pain and stiffness in knee arthritis.
Short-wave diathermy is another physiotherapy method that is frequently used for heating deep tissues. Short wave diathermy uses electromagnetic waves with a frequency defined for this purpose. It has a positive effect on pain, muscle spasm and joint stiffness.
Taping techniques can be used for non-surgical knee arthritis treatment. With kinesiologic taping method, pain can be reduced as well as stimulating the muscles and supporting the joint structure.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Restless Leg Syndrome?

Restless legs syndrome (RLS), also known as Willis-Ekbom disease, is a chronic (ongoing), progressive movement disorder characterized by abnormal sensations that occur with the urge or need to move the legs. Patients characteristically have difficulty describing their symptoms. They often describe it as an unstoppable urge to move the legs, a pain-burning-tingling sensation that is not very painful, but quite uncomfortable. This discomfort occurs at rest, worsens at night and often wakes them from sleep, leading to chronic sleep disturbance and emotional stress. When diagnosed correctly, the patient’s complaints regress and the condition can be controlled.
How does restless leg syndrome develop?
It has been proven that dopaminergic activity is impaired in the development of restless leg syndrome. PET and SPECT studies have shown pre- and post-synaptic dopamine receptor abnormalities in the basal ganglia of the brain.
What is the Prevalence?
Since most of the cases are undiagnosed, the prevalence of the disease is not known with certainty. According to epidemiologic studies, restless leg syndrome can be seen in 1-15% of the population. Most of the patients who consult a doctor are middle-aged and elderly. However, in 35-45% of cases, complaints begin before the age of 20 years and the prevalence in childhood and adolescence is around 2%. While symptoms are usually mild in the early period, they worsen with age and the need for treatment emerges at the age of 50-60 years. It has been reported to be approximately 2 times more common in women. In addition, the prevalence of RLS increases in the population with low income levels, smokers and those who do less than 3 hours of sports per month.
What are the Types of Restless Leg Syndrome?
Primary Restless leg syndrome
Primary or idiopathic RLS is the form without all clinical conditions known to cause the secondary form. Laboratory, neurologic, neurophysiologic and neuroradiologic tests should be normal. The idiopathic form accounts for 70-80% of all RLS cases. Hereditary transmission is remarkable in these patients. It has been reported that the disease can be seen in approximately 50-70% of first-degree relatives of patients with idiopathic RLS and women are more commonly affected. In this hereditary form, the disease starts at an earlier age, is usually diagnosed before the age of 45 and has a considerably slower course compared to secondary forms.
Secondary restless leg syndrome
It is known that various clinical conditions can lead to restless leg syndrome. The most common of these clinical conditions are iron deficiency, pregnancy, diabetes (type 2), end-stage renal failure and rheumatic disorders. Iron metabolism disorder, which is the common point of secondary causes, is an important factor in the development of restless leg syndrome. Patients with restless legs syndrome may also experience limb (arm and leg) and joint pain. For example, low back pain was found to be 38%, joint pain 50%, and soft tissue rheumatism 30% in these patients.Although restless leg syndrome is associated with many rheumatic diseases, the best known is rheumatoid arthritis. In one study, it was observed in 25% of patients with RA. In addition, the frequency of RLS in patients with fibromyalgia syndrome was reported to be 31%, 24% in SjS and 22% in scleroderma. 32.7% of MS patients have restless leg syndrome.
How is restless leg syndrome diagnosed?
The diagnosis of restless legs syndrome is mainly based on clinical history. Most patients have difficulty expressing their symptoms. Some of them describe their complaints as burning, itching, stinging, pricking, stinging and chilling pain in the legs, the need to move them and restlessness. The complexity and difficulty in identifying the symptoms make the diagnosis difficult. Symptoms usually begin with discomfort in one leg. In severe cases, both legs or other parts of the body such as the buttocks, trunk, arms or even the face may be affected. In all cases, however, the legs are affected and it is usually expected that the legs will be affected earlier and more severely than other parts of the body.
Discomfort in the legs starts with rest. This discomfort is not obvious at first, but becomes more pronounced with prolonged rest. Symptoms may occur while sitting or lying down. There is no specific body position for the onset or relief of symptoms. The feeling of restlessness in the legs is expected to go away with movement. Flexion-extension movements of the legs or stretching-stretching maneuvers can be effective. However, symptoms may often require getting out of bed and walking, hot or cold baths.
Since the diagnostic criteria for RLS are clear, there is no difficulty in making a diagnosis in suspected patients. However, it needs to be differentiated from some clinical conditions with similar clinical features such as pain in the extremities, movement disorders and sleep problems. Apart from these, a number of laboratory tests are recommended to clarify secondary RLS and associated conditions. These include ferritin, BUN, creatinine, fasting blood sugar, magnesium, TSH, vitamin B12, folate, glucose tolerance test.
How is Restless Leg Syndrome Treated?
Physical Therapy
In patients with mild symptoms of restless legs syndrome, non-pharmacologic treatment methods should be tried before prescribing medications that may have various side effects. Mild to moderate physical activity such as stretching exercises and warm baths before going to sleep may help. During rest, activities that increase mental activity such as computer games and puzzles are recommended. In addition, arrangements such as keeping the bedroom cool, using comfortable pajamas, going to sleep at the same time and waking up at the same time, and establishing a regular sleep pattern such as not sleeping during the day are recommended. Patients should avoid caffeine, nicotine, alcohol, antihistamines, antiemetics with antidopaminergic activity, antipsychotics and antidepressants, which are known to exacerbate symptoms. Sedentary activities that require prolonged rest, such as air travel or watching movies, can be done in the morning, while activities that reduce symptoms, such as housework or exercise, can be done later in the day. Medical ozone treatments also have positive results in controlling the condition.
Drug Treatment
Although non-pharmacologic treatment works well in patients with mild symptoms, patients with moderate to severe symptoms often require medical treatment.One of the main goals of treatment is to provide adequate and restorative sleep at appropriate and desirable times.The first dopaminergic drug used in restless legs syndrome is levodopa (with a decarboxylase inhibitor). It is recommended to start with as low a dose as possible and gradually increase the dose according to need. The most common side effects observed with dopaminergic agents are gastrointestinal side effects such as nausea, vomiting and dyspepsia. Since only 10-20% of the doses used in Parkinson’s disease are used, serious side effects such as dyskinesia are not expected. Gabapentin is a molecule with proven efficacy in this disease in randomized controlled trials. It is a good alternative especially in patients with mild, painfully perceived, painful peripheral neuropathy.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What are Tendonitis and Bursitis?

Tendonitis or bursitis is inflammation of the shoulder, elbow, wrist, knee, hip and ankle. Usually inflammation occurs over a long period of time. However, in some cases, sudden inflammation problems can also occur. This is due to overuse and abuse. For example, some people may have to constantly carry heavy loads with their shoulders due to their profession. This can lead to inflammation of the shoulder bones. People who carry very heavy loads with their hands may also develop inflammation in their elbows and wrists. People who are constantly standing are at high risk of developing inflammation in their knees and feet. People who have to work sitting down all the time may also develop inflammation in their hips.
Tendonitis In tendonitis, tendons and muscles become thinner and easily damaged. This can cause inflammation. Tendonitis can cause severe pain.
Bursitis: Inflammation of the small sacs between the tendons or skin between bone and muscle. This inflammation can cause severe pain.
What are the causes of tendonitis and bursitis?
- Repetitive repetition of the same movement can lead to tendonitis and bursitis. Examples include typing on a keyboard for a long time, walking, cutting and chopping.
- Not choosing the right shoes can also cause tendonitis and bursitis. Shoes that make the foot uncomfortable cause tendonitis and bursitis.
- Blood and kidney diseases can also cause tendonitis and bursitis.
- Tendonitis and bursitis in the legs, hips and elbows are much more common in old age.
- The use of certain antibiotics and medications can also cause fiber tears, leading to tendonitis and bursitis.
How are tendonitis and bursitis diagnosed?
In tendonitis and bursitis, the patient is first physically examined. The cause, severity and history of the disease are learned. Imaging techniques such as X-ray and MRI can be used for this. Blood tests may be required to measure inflammation.
How are tendonitis and bursitis treated?
Tendonitis and bursitis is a condition that seriously affects the bone and muscle structure. The methods applied in the treatment of these disorders are as follows:
- The first step in all bone and muscle diseases is rest. In this way, muscles and bones should not be overloaded, heavy lifting should be avoided and care should be taken not to be hit.
- Ice application is a very effective treatment method for pain relief. Applying ice compresses to the painful area 3 or 4 times a day for about 15 minutes helps to reduce the pain.
- In tendonitis and bursitis, medication can be used to relieve pain and inflammation.
- Repetition of the movements that cause tendonitis and bursitis may interfere with the treatment of the disease. For this reason, it may be necessary to use supportive tools and apparatus in the area where the pain occurs. For example, the use of a walking stick can relieve the load that causes pain, preventing healing and recurrence of discomfort.
- Tendonitis and bursitis can be treated with physical therapy. Smart exercise programs, massage, cold and hot applications can be applied by expert therapists in the field.
- If the disease cannot be treated with physical therapy techniques, surgical intervention may be necessary. However, surgical intervention is the last step in the treatment of tendonitis and bursitis. In some cases, cortisone injection may be sufficient. In cases where cortisone does not help, surgical intervention may be necessary.
How to take precautions against the risk of tendonitis and bursitis?
Here are some things to consider against the risk of tendonitis and bursitis:
- The risk of tendonitis and bursitis is very high in people who do intense sports and exercise. For this reason, you should take care to do warm-up and stretching movements before doing sports or exercise. This minimizes the risk of tendonitis and bursitis.
- Doing sports or exercise too fast can also cause tendonitis and bursitis. For this reason, exercise should be started slowly and accelerated as you warm up.
- Taking a long break from exercise and then starting again can also cause tendonitis and bursitis. For this reason, it is much more beneficial to exercise regularly for 25-30 minutes every day instead of doing intense exercise once a week.
- Using the right equipment and sports equipment also minimizes the risk of trauma.
- Staying in the same position all the time also causes tendonitis and bursitis. For this, the position should be changed at regular intervals and you should walk.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is curvature of the spine?

Lumbar slippage refers to the displacement of one vertebra in the lumbar region forward or backward over another vertebra and is called spondylolisthesis in medical language. Curvature of the spine are detected in 10% of people who consult a doctor because of low back pain.
How does a curvature of the spine occur?
Curvature of the spine can occur due to congenital abnormalities of the lumbar vertebrae. It can also be caused by degeneration, i.e. the wear and tear caused by the aging of the spine and surrounding connective tissues. It may occur due to traumas such as falls and traffic accidents. Inappropriate sports and strenuous movements can also be the cause of slipped discs.
What are the symptoms of curvature of the spine?
The most common complaint in curvature of the spine is low back and hip pain. There may be lower back and leg pain and numbness that increases with walking and decreases with stopping, resting and bending forward. Muscle tension, weakness and cramps may also occur in the legs.
How is curvature of the spine diagnosed?
In addition to a careful physical examination, curvature of the spine are almost always diagnosed with direct radiographs. Films may need to be taken in different positions to determine whether the slippage increases with movement of the spine. Computed tomography can be used to detect the condition of the bones or stress fractures that cannot be seen on direct radiographs. In addition, MRI to show the degree of slippage and the pressure on the nerves can be guiding in the treatment.
How is a curvature of the spine treated?
The main treatment for curvature of the spine is conservative (non-surgical treatment). Restriction of movements that increase pain and slippage, weight loss, painkillers, use of corsets, physical therapy applications are the main treatment methods. 10-15% of cases do not respond to conservative treatment and require surgical intervention. Surgical treatment may be required to stop the progression of neurological deficits, stabilize the lumbar spine and restore the integrity of the spine in patients with a degree of slippage above 50%.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Clinical Pilates?

The Pilates method is based on the unity of mind and body from ancient Greek philosophy. Pilates is based on a combination of eastern mind-body-spirit theories with western theories of biomechanics, motor learning and core stabilization. Pilates exercises, which require mental effort and are performed at a controlled pace, focus on the activation of specific muscles, quality of movement, stability and control of movement.
It has been included in rehabilitation programs more and more in recent years.
It is applied to prevent disorders that may occur in the musculoskeletal system or to treat and support the disorders that have already occurred.
What are the Principles and Importance of Pilates?
Although Joseph Pilates did not specifically write principles for his method, there are principles that are accepted as the basis of the system.
Respiration
As Joseph Pilates recognized, it can be shown as the structure of the body, mind and spirit.
Concentration
Concentrate on the posture of the body and achieving the correct posture and state of the exercise. Mental concentration is maintained during the session.
Center
Each person’s personal center of gravity is structured differently, and where the center of gravity clearly lies affects how the exercise feels and whether it will be difficult or easy to achieve. The center also refers to the infinite balance of energy that is released from all movements.
Control
Control is considered to be the order of execution of the movement. A high level of control often brings fewer and smaller errors, precise alignment, better coordination, better balance and the ability to perform more than one exercise from multiple attempts, less effort and avoid unnecessary muscle tension.
Accuracy
Precision distinguishes Pilates from many other exercise systems. Precision is defined as the precise execution of movement.
Fluid Movement
Fluid movement requires a deep understanding of the movement and precise cooperation of muscle movement and proper timing.
What are the Benefits of Pilates Exercises?
Pilates exercises can be used to strengthen muscles, increase flexibility and endurance, improve balance, improve and correct posture.
With correct breathing techniques, blood circulation is supported and thus positive effects on mood are achieved.
What are the Characteristics of Pilates Exercises?
Pilates consists of multiple muscle synergies including isometric, eccentric and concentric muscle contraction. It emphasizes lumbopelvic stabilization, stability, segmental mobilization of the spine, shoulder, elbow, hip, knee, ankle mobilization and stability, coordination and balance.
Which ailments can Pilates be used for?
It has been modified for individuals of all ages, after pregnancy or trauma, as well as for elite athletes and dancers. It can be used for strengthening purposes for beginners in rehabilitation programs.
Pilates exercises can be used in cases of chronic pain, scoliosis treatment, osteoarthritis (calcification) treatment, fibromyalgia (soft tissue rheumatism), osteoporosis (osteoporosis), mobility in hospitalized patients, activity development in gymnasts, flexibility development.
How to Plan Pilates Exercises?
In reformer pilates, springs and pulleys of different resistances are used. In Met exercises, hoops, balls and rollers are used. Individualized planning can be made. In general, it is planned 2-3 days a week for 45 minutes.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is adhesive capsulitis?
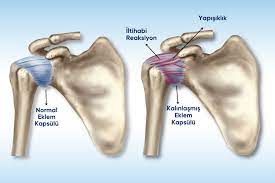
Frozen shoulder (adhesive capsulitis) is a serious health problem that can severely impair quality of life and is associated with progressive limitation and pain. It occurs as narrowing, thickening and inflammation of the shoulder joint capsule and restriction of joint movement due to decreased intra-articular fluid. Although it is mostly seen in one shoulder, it can sometimes affect both shoulders. It is more common in women and is more common between the ages of 40-65.
How Does Frozen Shoulder Occur?
Although frozen shoulder may occur due to various reasons, an underlying cause may not be detected in most cases. Sometimes frozen shoulder may occur years after an old shoulder injury. It can develop after conditions such as a heart attack, which can cause the shoulder joint to remain immobilized for a long time, or traumas such as falls and bumps. Calcification of the shoulder joint, shoulder impingement syndrome and muscle-tendon tears, inflammatory rheumatism and diabetes can be initiators for the development of frozen shoulder.
What are the Symptoms of Frozen Shoulder?
- The most important symptoms of frozen shoulder are pain and limitation of movement. The clinical picture usually progresses in three stages:
- Stage one It starts with severe pain around the shoulder. This is followed by progressive joint stiffness. The pain becomes more severe, especially at night. This period lasts between 2-9 months.
- Second stage: The pain gradually decreases, but movement restriction and stiffness persist. Restrictions in activities of daily living such as eating, dressing and undressing become more pronounced. This phase lasts 4-6 months.
- Third stage This is the resolution phase in which pain and limitation gradually decrease. This phase lasts for about 6 months to three years.
How is Frozen Shoulder Diagnosed?
Frozen shoulder is diagnosed with a careful patient history and physical examination. The condition of the shoulder joint is checked with a direct radiograph. In some cases, more advanced imaging methods such as ultrasound and MRI and laboratory examinations may be used.
How is Frozen Shoulder Treated?
The aim of frozen shoulder treatment is to relieve pain and restore range of motion and functionality. For this purpose, painkillers and anti-inflammatory drugs, muscle relaxants, intra-articular local anesthetic or cortisone injections may be useful. It is important to maintain joint range of motion from the early period. For this purpose, a rehabilitation program including physical therapy and exercise applications should be started. Superficial cold and heat applications, ultrasound, laser, pain relief current treatments, dry needling, acupuncture, kinesio taping, hydrotherapy and massage are among the treatment methods used in the treatment of frozen shoulder. Exercise program for joint range of motion should be started and continued from the early period.
Surgical intervention may be required in some resistant frozen shoulder cases where conservative treatment fails. It is important for the success of the treatment to start rehabilitation in the early period after arthroscopic intervention.
If frozen shoulder is not treated, complaints may continue for years. In most patients, limitations in the shoulder joint may become permanent.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is a trigger point?

Trigger points are painful and sensitive points on the muscles that usually develop on the basis of tight bands. These tense bands are also popularly referred to as earaches. In addition to pain and tenderness, trigger points can seriously impair quality of life by causing stiffness and limitation of movement. If it lasts for a long time, it can trigger similar conditions in other parts of the body by creating weakness in the muscle. This painful condition, which can coexist in one or more muscle groups, is called myofascial pain syndrome.
Why does a trigger point occur?
Trigger points are usually located at the midpoints of muscle fibers. These are the points where nerves enter the muscles and transmit their signals. Excessive and severe contraction of muscle fibers occurs due to causes such as overuse, stress, trauma or strain due to postural disorders. When muscle fibers that cannot fully relax remain contracted continuously, there is a lack of oxygen in the area and an inability to remove harmful substances. This creates a pain signal and leads to increased contraction, creating a vicious circle. The initiating cause may be long-term injuries due to repetitive microtraumas, or injuries due to a sudden load on the muscle may also be responsible for trigger point formation.
What are the symptoms of trigger points?
Trigger points occur mostly in the head, neck, shoulder girdle, back and lower back. They may not always cause pain. Sometimes they can remain silent for years without causing any symptoms. Although the most important symptom is pain, they can cause a wide range of symptoms and signs such as weakness, fatigue, limitation of movement, posture disorders, edema, nausea, dizziness, sleep disorders and depression.
The pain may be described as a dull ache, or it may occur as a headache, neck, back, lower back, shoulder and hip pain, sometimes radiating to the arms or legs. The pain may be constant or intermittent. It is usually debilitating and restrictive.
One of the important symptoms of trigger points is reflected pain. It can be seen in different parts of the body such as the jaw, ear, throat, wrist, fingers, knee, ankle and foot and can cause movement limitations.
Conditions such as fatigue, excessive exercise, cold weather, prolonged immobility, emotional tension, stress and viral infections can lead to increased complaints.
How is trigger point treatment performed?
The aim of myofascial trigger point treatment is to relieve pain, provide adequate muscle strength and eliminate the resulting limitations. First of all, factors that may cause discomfort, such as posture disorder, excessive and inappropriate use, stress should be tried to be prevented. Pharmacologic agents such as anti-inflammatory drugs and muscle relaxants can be used to relieve pain in trigger point treatment.
Different treatment methods can be applied in trigger point treatment:
- Trigger point injection
- Dry needling
- Acupuncture
- Spraying-stretching
- Massage
- Physical therapy applications (Ultrasound, TENS, interference, laser, superficial heat application)
- Ischemic pressure application
- ESWT (shock wave therapy)
- Hiltherapy (high-intensity laser therapy)
- Exercise
How is trigger point injection performed?
It is an effective and common treatment method in trigger point treatment. Local anesthetics, steroids or botulinum toxin can be used for this purpose. First of all, the points that trigger pain are identified. After skin cleansing, a needle is inserted into the trigger point and medication or saline is applied. The procedure takes a few seconds and the effect on pain occurs within minutes. The procedure can be repeated several times on different days if necessary. If supported with stretching exercises on the affected muscle, the success rate of the treatment increases.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Hip Osteoarthritis?

Osteoarthritis, or arthritis as it is commonly called, is a common health problem, especially in older people. Degenerative joint disease and arthrosis are other names given to this condition. One of the joints where calcification-type joint disease is common is the hip joint.
Calcification is basically a cartilage disease. However, in advanced stages, other structures of the joint are also affected and as a result, the joint develops insufficiency, i.e. the inability to function normally. Osteoarthritis of the hip joint can be defined as the wear of the cartilage covering the surface of the bones forming this joint for various reasons and the deformation of the bones over time. Since the hip joint is one of the weight-bearing joints in the body, it is one of the joints most frequently subjected to wear and deterioration. Although it is generally seen over the age of 60, it can occur at an earlier age in cases such as congenital hip dislocation, traumas, arthritis and childhood hip bone diseases.
What are the Symptoms of Hip Osteoarthritis?
Although hip arthritis is less common than knee arthritis, it can make life more difficult for patients and affect their quality of life more. The most important complaint is pain. Pain and difficulty in daily activities such as sitting up and down, climbing up and down stairs, getting in and out of the car, wearing socks are important symptoms. As the disease progresses, pain and difficulty can be felt even in simpler activities. In more advanced periods, pain may also be felt during rest. The degree of pain is not constant. It may be more in some months or days, or there may be painless periods. In cases where the mobility of the joint is severely restricted, walking difficulties occur.
How is hip arthritis diagnosed?
With a careful physical examination, it is possible to have an idea about where the hip pain originates from. X-rays are usually taken to differentiate pain that reflects or radiates from other areas and to visualize the condition of the hip joint. In some special cases, ultrasound, computed tomography or magnetic resonance imaging may be required. Blood tests may also be required if the doctor deems appropriate.
How is hip arthritis treated?
The aim of treatment is to relieve pain, slow the progression of arthritis and improve the patient’s quality of life. For this purpose, appropriate lifestyle changes are recommended according to the patient. Some of these measures include losing excess weight, avoiding sitting and staying in the same position for a long time, not sitting cross-legged, not preferring chairs or seats lower than knee level, having a toilet riser installed in the toilet if necessary, wearing comfortable shoes with appropriate soles, heels and heels that reduce impacts, and using a cane if necessary.
Exercises to increase muscle strength and maintain range of motion should be an important part of treatment. It will be useful to continue appropriate sports such as swimming and walking.
In addition to relieving pain in hip arthritis, some medication is used to slow down the progression of the disease. However, these medications must be used under the advice and supervision of a doctor.
Physical therapy applications are one of the most frequently used treatment options in the treatment of hip arthritis. Electrotherapy, ultrasound, laser, short wave, superficial heat applications, hiltherapy are the most commonly used physical therapy methods. In-water exercises and spa treatment are also effective treatment methods in the treatment of hip arthritis.
Ozone, hyaluronic acid, platelet-rich plasma and cortisone injections into the hip joint can be used in appropriate cases.
In cases where the disease progresses, surgical treatment methods are used. The most common method is hip replacement surgery. In this method, the deformed hip joint is replaced by an artificial hip joint. Rehabilitation of the patient after hip replacement surgery is very important in terms of returning to normal life. A special rehabilitation program is organized for the patient. In this program, the patient is gradually trained to load, walk, climb up and down stairs. In the meantime, exercises aimed at stretching, increasing joint range of motion and strengthening the muscles are performed. Physical therapy methods are utilized if needed. In-water exercise therapies are among the effective treatment methods that can be applied in this period.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Achilles Tendonitis?

The Achilles tendon is the largest tendon in the human body. It runs from the back of the ankle to the calf muscles. Although it is the strongest tendon in the body, it can be easily damaged. Achilles tendonitis, a condition usually seen in athletes, is an inflammatory disease that develops due to sudden strain or overuse of the tendon.
What Causes Achilles Tendonitis?
There is no direct injury in the formation of Achilles tendonitis. The causes of Achilles tendonitis can be listed as overuse, sudden increase in activity level, constant use of high heels and overweight.
Achilles tendonitis can also occur in cases such as improper training, keeping warm-up movements short, playing sports in uneven areas, too high foot arch and leg inequalities. In addition, the risk of Achilles tendonitis is higher in hemodialysis patients, diabetic patients and people with anatomically high posterior protrusion of the heel bone.
Causes that Trigger Achilles Tendonitis Attack:
- Too fast action after rest
- Sudden increase in speed during running
- Adding stair climbing or hill running to routine sports activities
- Overuse of the muscle
- Extra effort on the foot
- Sudden or severe contraction of the calf muscle
What are the Symptoms of Achilles Tendonitis?
- Worsening pain after exercise and running,
- Pain and stiffness along the Achilles tendon in the morning
- Increased pain and tenderness in the area where the tendon is attached after excessive activity
- Morning tenderness at the point above where the Achilles tendon attaches to the heel bone
- Overall reduction of stiffness as the tendon warms up with the use of the muscle,
- Tendon thickening and swelling
How is Achilles Tendonitis Treatment?
The general principles of treatment should include rest, cold application and anti-inflammatory treatment in the acute period. Along with shoe modifications, the use of orthotics such as heel pads and Achilles stretching exercises are important. Ankle strengthening exercises should be added to achilles stretching exercises after the acute condition has passed.
First six weeks:
- Immobilization until the pain subsides
- Antinflammatory therapy (NSAIDs, cold application)
Physical therapy methods such as ESWT, high-intensity laser therapy, ultrasound and TENS can also be used to treat pain.
- Gentle stretching exercises: Achilles and hamstrings, 3-4 times/day
- Usually the pain subsides in 2 weeks, after which you can return to daily activities;
- Isometric/isotonic strengthening
- Load transfer
- Balance/proprioception training
- In-water exercises and swimming are practiced.
After 6 weeks:
If it is painless, a return to sports can be achieved provided that the exercise program is continued.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Carpal Tunnel Syndrome?

Carpal tunnel syndrome, which can be defined as wrist canal impingement syndrome, is an important health problem especially in the active working population. It is a complex disease that can give a wide range of findings from mild nerve compression symptoms to severe muscle weakness leading to serious loss of function. It is the most common type of peripheral nerve compression called entrapment neuropathies.
Carpal tunnel is the name given to the canal formed by the bones in the wrist and a thick covering called carpal ligament on these bones. The median nerve, which is responsible for the movement and sensation of some of the fingers, passes through this channel along with the tendons that provide finger movements. Carpal tunnel syndrome occurs when the median nerve is compressed in this canal due to various reasons.
What are the causes of carpal tunnel syndrome?
In most cases, carpal tunnel syndrome occurs as an overuse injury. It is especially common in people who have to perform repetitive and demanding wrist movements. It is known that carpal tunnel syndrome is more common in people who use computers for long periods of time, play certain musical instruments, work with heavy and vibrating hand tools, engage in sports such as tennis, table tennis, drivers and housewives who are too busy with housework and manual labor. Other risk factors for carpal tunnel syndrome include obesity, diabetes, hypothyroidism, acromegaly, gout, some rheumatic diseases and pregnancy. Carpal tunnel syndrome that occurs during pregnancy is likely to improve after delivery.
In some people, the wrist canal is structurally narrow and may predispose to compression. Nerve compression may also occur in the carpal tunnel due to regional causes such as fractures, tendon inflammations, sebaceous glands, cysts and tumors.
What are the symptoms of carpal tunnel syndrome?
Early symptoms of carpal tunnel syndrome include numbness, tingling and loss of sensation in the fingers. These sensory symptoms are often accompanied by pain in the fingers, wrist and arm. One of the typical symptoms of carpal tunnel syndrome is that the symptoms are particularly pronounced at night and the patient wakes up with numbness, tingling and pain in the hands. In order to relieve the symptoms, the patient shakes his/her hands and feels the need to rub his/her wrists. This can lead to serious sleep disturbance problems over time.
In cases that are not detected and treated in the early period, the impingement may progress and cause complaints to become permanent throughout the day, rapid fatigue in hand and finger movements, decreased grip strength and pain may spread to the elbow, shoulder and even neck area. In cases of severe impingement, atrophies (muscle wasting) of the palm and thumb muscles and severe muscle weakness and sensory disturbances may occur.
How is carpal tunnel syndrome diagnosed?
A careful patient history is very important in the diagnosis of carpal tunnel syndrome. This is followed by a comprehensive physical and neurological examination. In the meantime, some special tests are used to stimulate nerve compression. Electrophysiologic tests (EMG) are the most useful auxiliary method to show the location and severity of nerve compression. With this method, the conduction velocities of the nerves are measured and objective data about the compression are obtained.
Carpal tunnel syndrome can often be confused with painful conditions originating from the spine, shoulder and elbow, especially neck hernias. In order to make a differential diagnosis of such conditions, auxiliary diagnostic methods such as X-ray, ultrasound and MRI (magnetic resonance imaging) can be used when necessary. Blood tests may also be needed to investigate some underlying diseases that may cause impingement.
How is carpal tunnel syndrome treated?
Carpal tunnel syndrome is a condition that can be treated without surgery in most cases. Since it usually occurs due to overuse, the first step in treatment is to restrict excessive and forceful use of the hand and wrist area. Supportive wrist splints are also utilized during this period. These splints can be worn only at night or during the day if the complaints are severe. Painkillers and anti-inflammatory medication, regional steroid injections and in some cases B-complex vitamins can be added to the treatment.
Physical therapy applications used in the treatment of carpal tunnel syndrome include ultrasound, laser, pain relief and muscle strengthening current treatments, mobilization, manual therapy, dry needling and taping. Exercises to increase flexibility and muscle strength should be started as part of the physical therapy and rehabilitation program and continued for the recommended duration.
Surgical treatment is considered in patients whose complaints do not improve with these conservative treatments or who have severe conduction disorders and significant neurologic deficits. With surgical treatment, the ligament on the carpal tunnel is cut and the canal is freed. After the operation, an exercise program is continued to provide joint range of motion and to strengthen the muscles.
What should be done to prevent carpal tunnel syndrome?
- Avoid jobs and activities that strain the wrist.
- Use wrist bracelets and splints to support the wrist if necessary.
- Avoid working with the wrist constantly bent.
- Take breaks during work. Do stretching exercises during these breaks.
- If you use a computer, use wrist-supportive mouse pads and keyboard supports.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Muscle Tears

In the shoulder joint, there is a muscle group consisting of four muscles and tendons called the rotator cuff. This muscle group provides stability of the shoulder joint and enables rotational movements of the arm.
What are the causes of shoulder muscle tears?
Since the shoulder joint is one of the most active joints of the body, it is prone to trauma. Rotator cuff tears are usually seen in individuals over the age of forty. Although it mostly develops on the basis of chronic repetitive trauma due to tendon wear and tear, it can also be seen in young individuals due to acute trauma or sports injuries.
There are some risk groups for rotator cuff tears. Individuals who play sports that require repetitive shoulder movements such as golf, tennis, rowing and people who work in professions that require the arm to work above shoulder level such as painters and ceiling workers are at risk.
Symptoms of Shoulder Muscle Tears
Shoulder pain, limitation of movement and sleep disturbances due to nocturnal pain are the most common symptoms of shoulder muscle injuries. Shoulder pain increases especially at night when lying on the affected shoulder. The pain is between the shoulder and elbow. Activities of daily living that require the use of the arm, such as combing hair, washing the head, dressing, etc. are painful and difficult to perform.
How are shoulder muscle tears diagnosed?
Although methods such as X-rays and ultrasonography are used in the diagnosis of rotator cuff tears, the most commonly used diagnostic method today is MRI (magnetic resonance imaging). With MRI, the location of the tear, its degree, the number of affected muscles and the amount of wear in the shoulder joint can be determined.
How are shoulder muscle tears treated?
Treatment of shoulder muscle tears is divided into two as conservative (non-surgical) and surgical treatment methods. When planning the treatment, many factors such as the onset and severity of the patient’s complaints, the patient’s age, occupation, lifestyle and patient expectations should be taken into consideration.
The aim of conservative treatment is to relieve pain, provide shoulder range of motion and strengthen the shoulder muscles. In the early period, intermittent cold application and pain reducing and anti-inflammatory drug treatments can be applied. Intra-articular injections can be performed in cases where the pain is severe and the limitation of movement is evident. In this period, it is recommended to start exercises in a way that does not increase the pain.
Physical therapy methods are also used in the treatment of shoulder muscle tears. For this purpose, a physical therapy and rehabilitation program including methods such as cold application, ultrasound, pain relief and muscle strengthening current treatments, dry needling, taping and Hilterapy (high intensity laser therapy) can be applied.
Appropriate exercise programs are started and continued to strengthen the muscles of the shoulder region.
Surgical repair methods may be considered for those who do not benefit from conservative treatments and have a full-thickness muscle tear. Surgical treatment can be performed arthroscopically or openly. After the operation, exercise therapy should be continued to restore range of motion and to strengthen the muscles in the region.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Impingement Syndrome
Shoulder pain is one of the most common painful conditions after back and neck pain. It is a serious health problem that can significantly affect a person’s daily life and working capacity. Shoulder impingement syndrome is the most common cause of shoulder pain. In addition to painful conditions such as bursitis and tendonitis, a wide range of diseases including serious muscle tears are included in this definition.
What is Shoulder Impingement Syndrome?
The shoulder joint is one of the most mobile joints of the human body. It is actively used intensively during daily life movements. The shoulder blade, collarbone and arm bone are the bone structures that make up the shoulder joint. Shoulder impingement syndrome occurs when the muscles that provide forward, backward and lateral movements of the arm are squeezed between these bone structures and the ligaments that connect them.
What are the Causes of Shoulder Impingement Syndrome?
Shoulder impingement syndrome occurs in most cases as an overuse injury. It can occur due to causes internal to the tendon of the muscle or external to the tendon. In some cases, both of these causes can coexist. External causes include congenital or acquired abnormalities of the bone structures in the area and calcification of the ligaments due to various causes. Internal causes are the wear and tear of the tendons in the area, which may lead to partial and then complete tears due to decreased blood supply over time.
Working in occupational groups that make repetitive overhead movements (e.g. painters, construction workers), some sports (e.g. throwing and throwing sports, swimming, basketball, volleyball), sudden and forceful movements (e.g. falls) and wear and tear in joint structures due to aging are known risk factors for impingement syndrome.
What are the Symptoms of Shoulder Impingement Syndrome?
Pain during arm movements is the most common symptom of shoulder impingement syndrome. The pain that occurs especially in overhead movements may become persistent over time and may keep you awake at night. The pain may spread from the shoulder to the front and side of the arm. Lying on the affected shoulder exacerbates the pain. As a result, shoulder movements become extremely painful and restricted and the patient may become unable to perform daily life activities such as dressing and undressing, brushing teeth and combing hair. In the following periods, weakness in the shoulder and arm muscles may occur.
How is Shoulder Impingement Syndrome Diagnosed?
Shoulder impingement syndrome is diagnosed with a careful patient history and physical examination. Straining movements, sports, traumas such as falls and bumps are questioned. In physical examination, the presence of impingement is investigated with the help of some special tests. Depending on the clinical condition of the patient, imaging methods such as X-ray, ultrasound or MRI (magnetic resonance imaging) may be needed. Other imaging and laboratory examinations may be used when necessary to exclude other causes of pain in the shoulder area.
How is Shoulder Impingement Syndrome Treated?
In the treatment of shoulder impingement syndrome, it is recommended to avoid movements that strain the arm in the early period. Especially movements and activities above the head level are restricted. During this period, intermittent cold application and pain-reducing and anti-inflammatory drug treatments can be applied. Intra-articular steroid injections can be performed in cases where the pain is severe and the limitation of movement is significant. Since complete immobilization of the shoulder will cause stiffness in the shoulder joint and weakness in the muscles, it is recommended to start exercises that will not increase the pain in this period.
Physical therapy applications have an important place in the treatment of shoulder impingement syndrome. For this purpose, a physical therapy and rehabilitation program including methods such as cold-hot applications, ultrasound, painkillers and muscle strengthening current treatments, manual therapy, dry needling, taping and Hilterapy (high intensity laser therapy) is applied.
Exercise therapy is an indispensable part of the treatment of shoulder impingement syndrome. Especially strengthening the muscles of the shoulder region is very important for the success of the treatment and prevention of recurrence of the problem.
Surgical treatment may be considered in patients who do not get results despite the treatments or in patients with complete rupture of the tendons in the imaging studies. Surgical treatment can be performed arthroscopically or openly. The structures causing the impingement are corrected with the operation. If there is a tendon tear, it is repaired. After the operation, exercise applications are used to restore the range of motion and to strengthen the muscles in the region. Physical therapy can be applied when deemed necessary.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Multiple Sclerosis (MS)

MS (Multiple Sclerosis) is a disease that occurs when multiple plaques form in the brain and spinal cord as a result of a disorder in the immune system. MS (Multiple Sclerosis), which can occur at a young age, affects approximately 3 million people worldwide. MS develops in attacks and can only be kept under control with appropriate treatment and regular follow-up.
What is the role of physical therapy in Multiple Sclerosis?
Muscle weakness, vision loss, altered sensory and pain perception, fatigue, emotional and cognitive changes are very common in Multiple Sclerosis (MS). These symptoms lead to balance and walking problems and changes in quality of life.
Especially walking problems and loss of balance limit activities of daily living.
Regular exercise and physical activity are important in preventing diseases, feeling well and supporting quality of life at all stages of life.
In order to improve the quality of life of the patient, to ensure that he/she can do his/her job or profession comfortably and to live his/her life without being independent from someone else, different PTR programs specific to each MS patient should be applied. In addition to the rehabilitation programs prepared to increase the hand and foot skills of the patient, Neurological Rehabilitation programs for the musculoskeletal system should be planned and applied individually by physiotherapists.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Canal Stenosis?
The lumbar spine consists of 5 bones, called vertebrae, arranged on top of each other. These bones surround the canal called the spinal canal, through which the spinal cord passes. There are pads called discs that allow movement between the vertebrae that make up our spine and absorb the load from the upper levels and ensure that it is properly transmitted to the lower levels, and joints and very strong ligaments that connect the vertebrae to each other. With advancing age, the discs lose their flexibility, the ligaments and joints thicken, and the bone structures can become coarser. All these changes lead to narrowing of the spinal canal and compression of the spinal cord and nerves passing through it, preventing them from functioning normally. The most important function of the spine is to protect the spinal cord and the nerves that exit the spinal cord, but it also allows for trunk movements and provides a connection point for the ribs.
What are the Symptoms of Canal Stenosis?
The most important complaint of narrow canal patients is pain, pain radiating from the lumbar region to the legs, tingling and numbness, cramps and loss of sensation, and if the disease is very advanced, there may be gait disturbance with loss of strength. The most typical clinic of the patients; neurogenic claudication, which we call neurogenic claudication, is numbness and tingling after walking a little way, with weakness in the legs and inability to take steps, and these complaints are reduced by sitting or leaning forward,
In the most advanced stages of the disease, a condition called cauda equina syndrome may occur with symptoms such as urinary and fecal incontinence, sexual dysfunction, weakness, loss of sensation and numbness in the legs. This is a condition that requires urgent surgery.
How is Canal Stenosis Diagnosed?
After a detailed physical examination and a well-taken history of the disease, the diagnosis can be made to a great extent. In order to confirm the diagnosis and plan the treatment, the patient may undergo tests such as plain or forward and backward bending radiographs, magnetic resonance imaging (MRI), computed tomography (CT) and lumbar myelogram, which show the stenosis in the spinal canal and spinal cord compression in great detail.
How is canal stenosis treated?
If there is no indication for surgery after the diagnosis of lumbar narrow canal, non-surgical treatments should be initiated first. The first step in the treatment of lumbar narrow canal is medication, training in activities of daily living and appropriate exercises. Various physical therapy applications are performed according to the condition of the pain. If there is no response to these treatments, spinal injections or blocks may be performed. If non-surgical treatment methods are not successful and progressive loss of sensation and strength occurs, surgical treatment should be considered. After surgery, the physical therapy and rehabilitation program should be reorganized and continued according to the patient.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Bone Marrow Edema

Bone marrow is the hollow part of the inner part of the bones that is mostly responsible for the production of blood cells. An increase in the amount of fluid in the bone marrow due to various causes is called bone marrow edema. The pressure created by the edema can cause pain.
What is bone marrow edema syndrome?
Bone marrow edema syndrome, formerly known as “transient osteoprosis”, “transient osteoporosis of the hip”, “transient migratory osteoporosis”, etc., is a disease of unknown cause. It is mostly seen in bones close to load-bearing joints such as the hip joint, knee and ankle. It is more common in women, especially in the last trimester of pregnancy. In men, it can be seen in middle age. It is a non-progressive clinical condition that is usually self-limiting.
Why does bone marrow edema occur?
Bone marrow edema is sometimes closely associated with trauma or bumps. Another common cause is joint arthritis. When the articular cartilage is damaged, its structure becomes thinner and the load on the bone increases. This increase may cause edema in the areas of the bone adjacent to the cartilage over time. Again, the risk of bone marrow edema increases in women during pregnancy. In addition, bone marrow edema may develop due to tumoral causes, radiotherapy treatment, gout, rheumatic diseases, sickle cell anemia, and cortisone use.
What are the symptoms of bone marrow edema?
Bone marrow edema is usually characterized by pain in the hip, knee or ankle, consistent with the area of onset. The pain increases with load on the joints (pressing, walking) and decreases when the load decreases. The patient tries not to put any load on the affected leg. A limping gait called antalgic gait is observed. In patients with hip involvement, pain may radiate to the groin and the front of the leg. Weakness may be observed especially in the muscles on the front of the leg. Sometimes the affected leg may be thinner than the other (muscle atrophy). Range of motion is usually unaffected.
How is bone marrow edema diagnosed?
In addition to clinical findings, magnetic resonance imaging (MRI) is important in the diagnosis. X-rays and computed tomography usually do not provide sufficient information. Bone densitometry (bone density) measurement helps to show a decrease in bone density on the affected side.
How is bone marrow edema treated?
Bone marrow edema usually has a good prognosis. Surgical treatment is rarely needed. Reducing pain and resting the affected side is very important in treatment. Pain medication can be used for pain relief. When necessary, it should be ensured that the patient does not step on that side with assistive devices such as canadians and crutches. The painful period may last for 6-8 weeks. In order to prevent bone resorption, drugs that prevent bone destruction can usually be added to the treatment for a while.
In the treatment of bone marrow edema, physical therapy and rehabilitation are used to prevent and treat both pain and long-term rest-related problems. Pain-relieving current therapies and superficial heat applications are used to reduce pain. Hiltherapy (high-intensity laser therapy) is an effective treatment to reduce edema in the bone marrow. In order to prevent muscle atrophy, weakening and limitation of joint movements due to immobilization, exercises that do not load the affected leg should be applied.
Complete recovery from bone marrow edema syndrome can take 6 months to 2 years. It may rarely recur in the same or another joint.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Tiptoe Walking
Tiptoe walking is defined as a child walking on their toes without the heel or other parts of the foot touching the floor. It occurs in 5% to 12% of healthy children and usually affects more boys than girls.
As children grow, they walk with a gait that consists of three different stages: initial heel strike, midfoot contact and toe-off. During the development of the first heel strike gait, some children walk on their toes. However, toe walking is not a mandatory stage that all children will progress to and most children have a heel strike by 18 months of age. Some children continue to walk on their toes and parents are encouraged to seek advice from health professionals when they continue to toe walk. However, there remains a lack of consensus on when to seek advice.
Anatomy
Our calf is made up of two main muscles.
- Gastrocnemius muscle. This is the larger calf muscle. Its two parts form the bulge that appears under the skin.
- Soleus muscle This small, smooth muscle is located below the gastrocnemius muscle.
Both muscles join at the base of the calf to become the Achilles tendon. The Achilles tendon then attaches to the calcaneus (heel bone). When the calf muscles contract, the Achilles tendon pulls the heel. The calf muscles and Achilles tendon work together to help lift the heel when walking.
In some children who walk on their toes, this muscle-tendon combination may be shorter at birth or may shorten over time, preventing the child from touching their heel to the ground and walking with their foot flat on the ground. However, in most children who walk on their toes, the muscle-tendon combination is long enough for the child to be able to walk on their heels if reminded to do so.
Why do children walk on tiptoe?
In the vast majority of children, toe walking is “idiopathic”, meaning that the exact cause is unknown. When these children are evaluated by a doctor, their physical examination and neurological tests are normal. In a smaller number of cases, it can be caused by an inability to heel strike due to underlying neurological or neuromuscular disease.
- Cerebral palsy
- Muscular dystrophy
- Spinal cord abnormality
- Congenital talipes equinus
- Autistic spectrum disorder
- In children with intellectual disabilities,
- In developmental speech and language disorders
What are the symptoms of tiptoe walking?
Most toddlers who tiptoe can walk flat-footed when asked. However, older children (usually children over the age of 5) who continue to tiptoe walk are unable to walk on their heels. These children may complain about problems wearing shoes or playing sports or participating in recreational activities involving roller skating or ice skating. Toe walkers do not have some complaints, but their parents are concerned about the impact of their walking patterns on their future functioning as teenagers and adults.
What are the examination questions in toe-walking children?
- Did you have pregnancy complications or was your child born prematurely?
- How old was your child when they reached developmental milestones such as smiling, sitting and walking?
- When did the toe walking start? (For example, did it start when your child started walking independently or at an older age?)
- Does he/she toe walk on both sides or only on one side? (Toe walking on only one side sometimes indicates a neurological problem).
- Is there a family history of tiptoeing?
- How much time is spent walking on tiptoes?
- Can your child walk straight if desired?
- Does your child suffer from foot or leg pain, weakness in the legs or difficulty keeping up with children of the same age?
What is done during the examination in children who walk on tiptoe?
The physical examination usually starts with observing the child’s gait. Your child’s feet are checked for abnormalities, including differences between the left foot and the right foot, differences in length and size in both legs, range of motion in the hips and knees, any skin abnormalities in the lower limbs and lower back.
Any contractures or excessive tension in the muscles of the arms or legs, strength of the main muscles, reflexes, sensation in the arms and legs are tested. If no problems are detected by history and examination, nerve and muscle tests such as X-ray, CT and MRI scans and EMG are usually not necessary.
What is the treatment for children who walk on tiptoe?
Treatment for toe walking depends on the age of the child and whether the child can walk normally. Young children and children with no limitation in ankle dorsiflexion are usually treated with non-surgical interventions. Older children who continue to tiptoe and have limitations in ankle dorsiflexion are sometimes treated with surgical procedures.
Non-Surgical Treatment
Observation; Regular monitoring is recommended. If it is getting out of habit, it can stop on its own.
Stretching exercises are usually prescribed in case of reduced ankle dorsiflexion.
A series of short leg casts can be done to gradually stretch and lengthen the muscles and tendons in the calf and break the habit of foot walking.
Orthotics; wearing an ankle-foot orthosis (AFO) can help stretch and lengthen muscles and tendons. An AFO is a plastic brace that extends the back of the lower leg and holds the foot at a 90-degree angle. Typically, it is used over a longer period of time (months instead of weeks).
Intramuscular botulinum toxin type A, usually those with neurologic abnormalities that cause increased muscle tone – botulinum A toxin injection can also be given to temporarily weaken the calf muscles. Injected into the gastrocnemius, soleus or both
Surgical treatment
In children over 5 years of age who walk on tiptoe, the calf muscles and Achilles tendons may be so tight that walking flat-footed is not possible. For these patients, surgery can be performed to lengthen the Achilles tendons. Lengthening the tendons will improve range of motion and allow the foot and ankle to function better.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is hallux valgus?

Hallux Valgus or thumb protrusion is the name given to the protruding deformity that occurs in the majority of women after the age of 30-40 and is caused by the inward rotation of the big toe and the outward rotation of the comb bone in the first toe.
This protruding condition and pain in the big toe affects life negatively by making it difficult for patients to wear shoes and walk. As a result of the compression disorder, painful callus development can be seen on the sole of the foot.
What are the Symptoms?
- Deformity In big toe protrusion, or Hallux Valgus, the most common complaint of patients is the protrusion of the first toe on the foot.
- Pain: In hallux valgus, finger movement and walking cause pain.
- Redness Depending on the shape of the shoe and the narrowness of the front part of the shoe, patients develop redness of the thumb (bunion).
- Discomfort: An uncomfortable sensation in the big toe caused by wearing shoes with pointed toes or shoes that are not suitable for the structure of the foot.
Who is at risk of having this condition?
Hallux Valgus is a health problem that is usually genetically transmitted between family members. While narrow high-heeled shoes play a role in the development in some patients, the disease can be seen in a group of patients despite wearing comfortable shoes without wide heels.
However, this disease can also be associated with other diseases.
- In people with flat feet
- Those with high curvature problem
- In patients with Achilles tendon shortness
- People with weight problems
- It appears in people with various rheumatic problems.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Baker cyst?

Baker’s cyst is a soft mass filled with joint fluid that occurs at the back of the knee and initially does not cause pain, but as it grows, it causes pain and limitation. Baker’s cyst is soft and causes sharp pain during physical activities such as stretching and bending the knee. Baker’s cyst is more common in women than in men and its incidence increases over the age of 40.
What causes Baker’s cyst?
After calcification and trauma to the knee joint, excessive joint fluid produced by the synovium accumulates in a sac behind the knee and a Baker’s cyst forms.
How to recognize a Baker’s cyst
Baker’s cyst, which causes a sharp pain on movement, causes discomfort when the leg is fully extended, stretched or bent. On examination, it is palpated as a swelling behind the knee. Sometimes there may be extreme swelling and pain in the leg after the cyst bursts. This may be confused with deep vein thrombosis. Definitive diagnosis can be made with joint ultrasonography and MR.
What are the Symptoms of Baker Cyst?
- Stiffness behind the knee
- Swelling behind the knee or in the leg
- Knee pain
- Rigidity, hardness
- Baker Cyst Treatment
Generally, appropriate exercise and physical therapy methods are followed up and the cyst is expected to disappear spontaneously. If it does not disappear spontaneously over time, drug treatment is applied. Another treatment method applied in the treatment of Baker’s cyst is aspiration. With this method, the fluid inside the cyst is removed. Aspiration is performed with the help of ultrasound. Finally, the cyst is removed by surgery. However, Baker’s cyst surgery is generally not preferred. Baker’s cyst surgery is seen as a last resort and is preferred in cases that have been drained many times but recur repeatedly.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Knee Replacement Rehabilitation

Knee replacement surgery is an operation that involves replacing the damaged joint with an artificial joint in patients whose knee joint has been damaged for certain reasons. Knee replacement is applied to relieve pain and movement limitations that do not respond to non-surgical treatments, to provide stability and to improve quality of life.
When is a knee replacement needed?
- If there is severe wear and tear in the joint due to osteoarthritis (calcification)
- In the presence of rheumatic diseases such as rheumatoid arthritis or ankylosing spondylitis that completely restrict the movement of the joint
- In bone tumors
- Knee prosthesis may be needed in patients with damage after knee joint infection and trauma.
Preoperative rehabilitation in knee replacement
It is important to start rehabilitation before the operation to increase the success of knee replacement. Starting rehabilitation in the preoperative period facilitates postoperative rehabilitation and accelerates the patient’s recovery and independence in activities of daily living. For this
- Teaching proper positioning of the knee
- Reduction of range of motion limitations,
- Strengthening exercises especially for the anterior thigh muscles
- Stretching exercises for shortened or strained muscles
- Teaching postoperative rehabilitation program
- It is important to teach breathing exercises and coughing to prevent pulmonary complications and to ensure secretion removal.
- Rehabilitation after knee replacement surgery
Goals of postoperative rehabilitation;
- Preventing negativities related to bed rest
- To provide adequate and functional range of motion
- Strengthening the muscles around the knee
- Ensuring independence in walking and activities of daily living
- To improve the patient’s quality of life.
Early mobilization of the patient in coordination with the surgeon is important for the success of postoperative rehabilitation. Here, a program should be implemented according to the type of prosthesis applied and the method of the operation. Reduction of pain, prevention of possible complications and joint positioning training are other points to be considered in the early period. A continuous passive motion device (CPM) is utilized in this period.
In-bed exercises are started on the first postoperative day. In the early period, exercises such as squeezing and relaxing the hips by counting to three, counting to three by pressing the back of the knee to the bed, counting to three by pulling the ankle towards itself and forward while the leg is extended, counting to three and releasing it, lifting the leg straight up and holding it to three and releasing it.
The patient is first seated on the edge of the bed. Then he/she is lifted to his/her feet with a walker. The amount of load to be given at the beginning varies according to the type of prosthesis applied. Discharge is planned when knee flexion reaches 90 degrees and the patient is able to transfer and mobilize independently. The patient and his/her family are taught what to pay attention to at home, what activities the patient can do and how to perform the exercises.
After discharge, the outpatient rehabilitation program continues. Crutches are gradually introduced and continued until approximately the sixth week. After the sixth week, resistance exercises are started. Crutches are first reduced to one, then unassisted walking training is started. It is recommended to continue exercises for at least one year after the operation.
Hydrotherapy, i.e. in-water exercise program, is also actively used in rehabilitation after knee replacement. During rehabilitation, attention should be paid to pain and edema control, and cold application and physical therapy methods should be applied when necessary.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Pediatric Knee Pain
Joint pain is common in childhood. Joint pain can occur in inflammatory and non-inflammatory conditions. The most common musculoskeletal complaint in children in primary care is knee pain (33%) and other joint pain (ankle, wrist and elbows 28%). Most complaints are usually benign and can be attributed to trauma, overuse or developmental variations, such as hypermobility and benign nocturnal limb pain of childhood (previously known as ‘growing pains’).
Bones, which are tiny at the time of birth, complete their growth and development through a series of complex processes until around 17-18 years of age. The arms grow mostly from the shoulders and wrists, while the legs grow 70-80 percent from the knees. This rapid growth can be the cause of the pain that children often complain of. The pain is mostly caused by edema that occurs after strain and tension in soft tissues such as muscles, tendons and ligaments around the bone, rather than the growth rate of the bone. However, it is still useful to have a specialist examine it, as infections, trauma and tumors can often be encountered in this area.
Causes of knee pain in children?
Growing pain (Benign nocturnal limb pain of childhood)
Children usually complain of pain in the evening or at night after daytime activities, but in the morning their complaints usually go away. For the treatment of growing pains, which occur mostly in the muscles above and below the knee, rest, massage or simple painkillers can be used. If no results are obtained and problems such as pain, swelling, redness and difficulty in walking persist throughout the day, children should be evaluated by a specialist.
Trauma and Pineal Plate Injuries
The bones in the arms and legs, which are long bones, need to grow in proportion. Any disproportion can be a sign of a problem in the knee joint. The epiphyses, which are the growth plates at the end of the bones, are not yet ossified during childhood. Therefore, this structure, which is still cartilage, can be damaged as a result of excessive sports or strain. In addition, traumas such as excessive sports or injuries can cause damage to the meniscus, ligaments and growth plates in this area. As a result of all these, the growth plate in the knee is affected, and inequalities or deformities may occur in the growth of the lower leg bones. In traumas caused by falls or blows to children, symptoms such as pain, swelling, bruising, tenderness and limitation of movement are seen. Unlike growing pains, traumas cause localized pain and are accompanied by bruising and swelling. Sometimes conditions such as slipping of the head from the growth plate at the femoral head in the hip (slipped femoral head epiphysis), perthes disease or synovitis of the hip also cause reflected pain in the knee. However, in all of these cases, the history is different and the pain is accompanied by a limp. Normal radiographs are used to determine whether there is a fracture or dislocation after trauma. Depending on the persistence of symptoms and signs, an MRI scan may be necessary.
Anterior Knee Pain and Patello-Femoral Malalignment
Anterior knee pain is very common and the most severe is dislocation and dislocation of the kneecap. Anterior knee pain describes pain felt around and below the kneecap, which is worse after prolonged periods of sitting (also known as cinema pain) and climbing stairs. It is more common in adolescent girls and is usually improved with VMO (vastus medialis obliqus) strengthening exercises aimed at realigning the strong lateral pull of the vastus lateralis on the patella. Recurrent dislocations may require surgical intervention.
Osgood Schlatter Disease
It is a disorder of the formation and growth of the proximal tibial apophysis that occurs during ossification in adolescents. In patients with anterior knee pain, tenderness and swelling are concentrated at the upper end of the tibia, which comes with exercise. It is relieved by rest. X-rays show fragmentation of the apophysis, but are not necessary to make a diagnosis as it is usually clinically evident. Treatment is symptomatic with rest, ice, analgesia and sometimes physiotherapy. Sports activities may need to be stopped or reduced.
Osteochondritis disecans This condition is caused by necrosis of a focal area of subchondral bone, most commonly affecting the lateral aspect of the medial femoral condyle. When the overlying cartilage loses its support structure, a fragment can fall into the joint. Repetitive microtrauma is thought to be an important initial factor. Symptoms are chronic, often vague and may include pain with activity, stiffness after rest, locking of the knee.
Radiographs are usually diagnosed if “tunnel radiographs” are obtained. An MRI scan is used to understand the extent and guide treatment. In general, in girls aged 11 to 13 years, they are treated conservatively and usually improve with a period of activity restriction. In older children, it is more difficult and may require arthroscopy or open surgery.
Infection
In bone and joint infections (osteomyelitis, septic arthritis), which are more common in children than in adults, the picture is much more severe than in growing pains. Children’s general health deteriorates. In infections, symptoms such as fever, chills, chills, swelling, redness, local or general increase in temperature, limitation of movement and difficulty in walking are added to severe pain. Inflammation trapped in the joint causes rapid and irreversible destruction of the articular cartilage, and rapid diagnosis and surgical evacuation is crucial. Intravenous antibiotics are required until the clinical picture is established (usually until CRP is normal) and then oral antibiotics for a total of two to six weeks.
Benign or malignant tumors; Benign or malignant bone tumors in childhood are more likely to be located in the long bones, especially in the long bones of the legs. Benign bone tumors reach a certain size as the child develops. Tumors located close to the joint may cause pain similar to growing pains as a result of pressure on muscles and tendons. However, while pain in benign bone tumors occurs with movement or contact, pain in malignant tumors is continuous. Tumors around the knee are often benign and in this case the pain. Pain that occurs at night and is relieved by aspirin is classic for an osteoid osteoma, but night pain and rest pain may be a more worrying sign of a neoplastic lesion. Malignant tumors such as osteo-sarcoma, although rare, tend to be located around the knee joint. They are usually associated with short-term worsening pain, mass, bone destruction and soft tissue reaction and swelling. Again, tumors around the hip may present with knee pain.
Blood Diseases
One of the problems that can be confused with growing pains is blood diseases and leukemia. In hemophilia, a blood disorder characterized by non-stop bleeding, swelling and bruising may accompany the condition. In leukemia, the child may experience constant pain that does not go away with rest.
Rheumatic diseases
Another disease that is similar to growing pains is rheumatic diseases. Rheumatic diseases, which have been on the rise in children in recent years, can often present with pain in the joints. Rheumatic pain in children can be both prolonged and severe. Muscle fatigue, fever and aphthae in the mouth may also indicate rheumatism. As in adults, reactive arthritis in children can be associated with viral infections. There is usually a previous history of viral infection. It can be caused by a cold, flu, sore throat. Inflammatory arthritis also usually comes with a limp that is more common than acute pain. The pain is felt as morning stiffness or stiffness after long periods of inactivity. A warm environment improves the symptoms. It increases in the cold.
Children with joint pain may experience impaired physical, emotional and social functioning as well as sleep disturbances and fatigue. Increased stress and low mood in children and their caregivers are the most important risk factors for the development of chronic musculoskeletal pain in children. Young children may adapt to joint pain by reducing joint use and not complaining about the pain. This is particularly important for the developing skeleton of children and the abnormal gait, muscle spasms and impaired load distribution and positioning that joint pain can cause. Therefore, observation and a full examination are essential for good assessment.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
Flat Feet Rehabilitation

Our feet are organs that can adapt to any type of ground and can easily carry the loads placed on them. The ability of the feet to function correctly depends on the extrinsic and intrinsic muscles working in an orderly manner.
The feet make a stretching movement from the heel to the front part of the foot during each stepping movement, and this stretching movement helps the feet to carry the body and walk more painlessly and for a longer time. This is a kind of springing movement. This springing movement is provided by the internal arches on the inner sides of both feet, which prevent the foot from collapsing. The absence of these internal arches is called flat feet (pes planus).
There are two types of flat feet. The first type is flexible flat feet, which is the most common type in the society. In this case, the problem is not in the bones, but rather in the muscles and ligaments, and when the person steps on the ground, there seems to be an internal arch, but when the weight is applied, the foot flattens. The second type is rigid flat feet, which is rarer than the first type and is detected and treated with advanced examination and treatment methods. In this type, the foot has a hard and tense appearance whether the patient steps on the ground or not.
What are the Symptoms of Flat Feet?
If the pain increases when standing for a long time and spreads to the leg, if the feet get tired quickly, if the pain usually starts at the heel and causes contractions in the calf muscles, if foot pain prevents doing sports anymore, if the inner parts of the shoes wear out much earlier than expected, a physician evaluation in terms of flat feet will be appropriate.
How is Flat Feet Treated?
If flat feet are detected after the physician’s examination and examinations, some measures and treatments are taken to improve the quality of life of the person. The first of these stages;
- It is information for the person to choose shoes with wide and soft soles.
- Custom-made soles and orthotics are recommended to support the inner arch of the foot.
- The physician recommends medications that prevent the reaction and pain in the tissues due to flat feet.
- Physical therapy options that can be applied under the leadership of exercises that support the internal arch of the foot.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Our feet are organs that can adapt to all types of ground and can easily carry the loads on them. The correct functioning of the feet depends on the extrinsic and intrinsic muscles working in an orderly manner.
The feet make a stretching movement from the heel to the front part of the foot during each stepping movement, and this stretching movement helps the feet to carry the body and walk more painlessly and for a longer time. This is a kind of springing movement. This springing movement is provided by the internal arches on the inner sides of both feet, which prevent the foot from collapsing. The absence of these internal arches is called flat feet (pes planus).
There are two types of flat feet. The first type is flexible flat feet, which is the most common type in the society. In this case, the problem is not in the bones, but rather in the muscles and ligaments, and when the person steps on the ground, there seems to be an internal arch, but when the weight is applied, the foot flattens. The second type is rigid flat feet, which is rarer than the first type and is detected and treated with advanced examination and treatment methods. In this type, the foot has a hard and tense appearance whether the patient steps on the ground or not.
What are the Symptoms of Flat Feet?
If the pain increases when standing for a long time and spreads to the leg, if the feet get tired quickly, if the pain usually starts at the heel and causes contractions in the calf muscles, if foot pain prevents doing sports anymore, if the inner parts of the shoes wear out much earlier than expected, a physician evaluation in terms of flat feet will be appropriate.
How is Flat Feet Treated?
If flat feet are detected after the physician’s examination and examinations, some measures and treatments are taken to improve the quality of life of the person. The first of these stages;
- It is information for the person to choose shoes with wide and soft soles.
- Custom-made soles and orthotics are recommended to support the inner arch of the foot.
- The physician recommends medications that prevent the reaction and pain in the tissues due to flat feet.
- Physical therapy options that can be applied under the leadership of exercises that support the internal arch of the foot.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Speech and Language Therapy?

In the treatment of speech and language disorders, various techniques are used to help the child speak better. Speech and language disorders are different concepts. In language disorder, sounds cannot be produced correctly. In speech disorders, on the other hand, sounds cannot be put together to form words and the person starts to have problems speaking.
Many different techniques can be used for speech and language disorders
Articulation disorder
The correct and harmonious use of the lips, tongue, teeth, jaw and palate to convey thoughts to other people is called articulation. Articulation disorders, on the other hand, refer to errors in speech, modification or sound production that occur as a result of improper use of this system. It is normal for children to use certain sounds incorrectly at certain ages. However, if a child who is 3 years old still produces a sound that he/she should have acquired incorrectly, he/she may have an articulation disorder. Saying “y” instead of “r” or “p” instead of “k” are the most common articulation disorders. Articulation disorders affect the intelligibility of a child’s speech when communicating with another person.
Stuttering
Stuttering affects the fluency of speech. It begins in childhood and in some cases lasts a lifetime. The disorder is characterized by disruptions in the production of speech sounds. Most people sometimes produce short discharges. For example, if your child says “ba-ba-bar-dak” or “bbbbbardak” instead of “cup”, this is a sign of stuttering. In most cases, stuttering occurs in certain situations that are difficult for the person. The activities that are difficult vary according to the individual. For some people, communication difficulties only occur during certain activities, such as talking on the telephone or speaking in front of large groups. For many others, however, communication difficulties can occur across a range of activities at home, at school or at work. They are disorders that need to be treated in terms of the person’s educational and career success and social relationships.
Voice disorder
It is the deterioration of a person’s voice quality, loudness or pitch. The fact that the child’s voice sounds guttural or as if he/she has a cold is among the indicators of voice disorder. Frequency and intensity changes can be seen in the voice while speaking. The high voice can be lowered towards the end of the speech. The quality, intensity and pitch of the voice can also be successfully corrected with speech therapy.
Language disorder
This is when children have difficulty communicating due to problems producing sounds, words and sentences. Children with language impairment communicate using fewer sentences than others their age. They may use sounds incorrectly, have difficulty forming words by combining sounds, or construct sentences incorrectly. In addition, language delay is among the problems of language impairment. It is among the problems that can be corrected with speech and language therapy.
What are the application areas of speech and language therapy?
When a person cannot produce correct or fluent speech sounds or has a voice problem, then they have a speech disorder. Examples of speech disorders include difficulties pronouncing sounds, articulation disorders and stuttering.
If a person has trouble understanding others (thinking language) or is not understood when they share their thoughts, ideas and feelings (expressive language), then they have a language disorder. Various medical conditions, such as stroke and aphasia, can also cause speech and language impairment.
Speech and language disorders can occur in both children and adults. It can be the result of a medical problem or have no known cause. Medical problems can include physical problems such as cleft palate or cleft lip, muscle weakness in the speech articuli. Both congenital speech disorders and acquired speech disorders can be treated with speech and language therapy. In short, speech and language therapists are used to treat problems such as stuttering, articulation disorder, voice disorder and language disorder.
Speech and language disorders in children with Down syndrome and autism can also be treated.
How many sessions does speech therapy last?
There is no standardized duration of speech and language therapy. Depending on the type, cause and level of the speech disorder in the person, the therapy is determined and applied individually for the person or the child. Depending on the success or failure of the therapy, the needs of the person are determined and the therapy plan is reorganized individually. The success of the therapy is directly proportional to the experience of the therapist, the willingness of the patient and the support of the relatives. All these criteria determine the duration of the therapy session.
What is the best age to start speech therapy?
By the age of 3, a child’s speech should be intelligible to people outside the family. In short, he/she should have the ability to express himself/herself, make sounds correctly and use words correctly. At the age of 3, if a child cannot express himself/herself adequately, cannot make sounds correctly and cannot use words correctly, he/she may need speech and language therapy.
After speech and language therapy, the child will have the ability to fully express himself/herself, make the correct sounds and form words correctly. In this way, communication, education and development will progress in a healthy way and in harmony with their peers.
How is speech and language therapy applied in adults?
Speech and language therapy can be successfully applied not only to children but also to adults. Only in adults, speech and language therapy may not produce results as quickly as in children. This is because the speech disorder is already established in the person.
However, since compliance with the speech and language therapy program is much higher in adults, problems such as stuttering and lisp can be treated successfully, although it may take a little longer.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Lymphedema?

When blood is pumped into the body by the pumping power of the heart, it is distributed throughout the body through the arteries. As it comes back to the heart, the more liquid part comes to the heart through the veins and the darker part comes to the heart through the lymph vessels. If there is a prolem in the veins, varicose veins occur, if there is a problem in the lymph, lymphedema occurs.
Lymphedema: It can be defined as the accumulation of protein-rich fluid as a result of impaired lymphatic circulation, sometimes congenital and sometimes after infections and surgeries.
What are the Causes of Lymphedema?
Lymphedema can sometimes be congenital and is known as elephantiasis. Lymphedema is also common after breast surgery, abdominal and pelvic organ surgery, joint replacement, radiotherapy and infections. The more lymph nodes removed and the larger the area of radiotherapy, the higher the risk.
When does lymphedema develop?
Congenital lymphedema can occur at any time of life. Post-surgical lymphedema develops immediately after surgery or gradually after 1-2 years.
What are the Symptoms of Lymphedema?
Feeling of tightness or fullness in the arm, pain, heaviness, tingling, swelling and redness, difficulty in movement in the arm, hand and wrist, squeezing of the watch, ring or bracelet, feeling of tension in the skin, related distress and restlessness.
When it swells gradually, it may not be noticed by the patient, relatives or doctor unless it is measured. When it is noticed visually, the diameter difference may have reached a level that needs to be treated.
If the swelling increases too much, discharge may occur in the area with lymphedema and this is called tears of the skin. These are areas open to infection.
How Can I Prevent Lymphedema?
It is not possible to predict the development of lymphedema. However, it is useful to inform the patient before surgeries with a risk of lymphedema.
- Do not neglect any swelling, contact your physiotherapist immediately.
- Keep your arm clean, take care of your skin.
- Apply moisturizer to the skin after bathing and during the day. Moisturizer should not contain alcohol, perfume, mineral oil, talc, lanolin.
- Do not have a manicure. Push the cuticles back instead of cutting them.
- Avoid repetitive movements such as rubbing, pulling, pushing with the arm at risk.
- In case of abrasions, scratches, insect bites on the skin, wash with soap, keep clean and protect. Use anti-bacterial cream. If there is an open wound, clean and close it. In case of mild burns, after cold application, wash with soap and water and protect.
- In terms of infection, be alert to symptoms such as redness, swelling, increased temperature, sensitivity and fever, and call your doctor immediately.
- Use an electric razor (not depilatory cream, wax or razor) to remove armpit and leg hair.
- Protect your arm from sunburn. Use sunscreen creams and avoid long periods in the sun.
- Make sure that the creams you use are not cosmetic. Inappropriate ingredients can cause allergies and sores.
- Be careful where there is a risk of insect bites, bee bites or cat scratches. If a bite occurs, clean the skin, raise the arm, apply cold and contact your doctor.
- Avoid things that irritate the skin.
- Always wear protective gloves when handling hot pots and pans coming out of the oven. Be careful with boiling water and food vapors from microwave ovens.
- Always check the temperature of the running water with your other arm before going to the bathroom, do not use water that is too hot.
- Do not scrub or washcloth in the bathroom.
- Avoid too hot environments such as saunas, spas or going out in extreme heat in summer.
- Try to stay away from any kind of heat!!
- Wear gloves when doing household and garden work.
- Wear a protective ring on your fingers when sewing.
- Do not get vaccinated in the risky arm, do not have your blood pressure measured, do not have your blood drawn.
- Avoid wearing tight clothing, gloves and jewelry.
- Avoid carrying bags and files with a risky arm.
- Underwear with wide straps that do not put pressure on the shoulders
- Do not hold your arm in a certain position for a long time. Movements such as holding the arm in a sling will cause limitation and swelling in your arm.
- Use a pressure armband when traveling.
What should I do if it swells?
Contact your doctor immediately, even if you have experienced this before, it would be appropriate to be evaluated by your physical therapist.
How to recognize lymphedema: The first thing to do when encountering a patient who is thought to have developed lymphedema is to try to understand the cause of lymphedema and to determine its type and stage as much as possible. If it started after a surgery, infection or radiotherapy, measuring the difference in diameter between two arms or legs is sufficient for diagnosis. If the cause is not clear, further diagnostic methods are used. Doppler ultrasonography, lymphoscintigraphy and MR can be used for diagnosis.
Is there a treatment for lymphedema?
Yes, there is a treatment for lymphedema. If you have recently swollen, the treatment will be shorter, if your arm has been swollen for a long time, the treatment will take longer. Therefore, starting treatment as soon as possible will increase treatment success.
How to Treat Lymphedema?
The aim of the treatment is to reduce the swelling and try to prevent it from occurring again. This process is a long process that the patient and the doctor should follow in harmony. But the results are positive for the patient.
- Proper skin care (moisturizer suitable for the arm should be applied in one direction from the bottom up, skin should not be dry) (2 times/day)
- The most effective treatment is manual lymph massage. Before the treatment, whichever extremity (arm or leg) is swollen is mapped and it is determined how to pass the blocked area. Then, starting from the place closest to the heart, the lymph vessels are drained towards the heart and the swelling is descended to the lowest part of the swelling. Afterwards, the patient’s swollen extremity is bandaged with a short tension bandage to drain the lymph for 24 hours.
- In the next phase of treatment, the patient or his/her relatives can be taught self-massage and manual lymph drainage (this should be done by trained and experienced people). Please do not let inexperienced people do it, your swelling may increase!)
- If the diameter difference is large (2 to 2.5 cm between the two arms), manual lymph massage and bandage treatment is started. The bandage treatment and the material used are specific. A multi-layered application is performed with a short tension bandage. It should be performed by an experienced physical therapy and rehabilitation physician. When the diameter decreases to different desired limits, the pressure cuff is applied.
- Pressure pumps (pneumatic compression applications)
- Exercises: the most important stimulator of lymph circulation is the muscle pump and with the right exercise, lymph circulation is accelerated and swelling can be prevented.
How does lymphedema affect us?
In case of lymphedema, infection or clot may develop in the arm or leg. Movement of the swollen arm or leg becomes difficult, over time there is limitation and pain.
Is there a treatment with medication?
In studies conducted all over the world, positive results have not been found that medication is effective in the treatment of lymphedema. Therefore, the use of medication is not recommended in treatment guidelines.
Is There a Lymphedema Diet?
Gaining weight increases the risk of lymphedema. Therefore, sugary, salty foods should be avoided and fiber foods should be consumed to prevent the body from retaining water and not gaining weight.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Cupping Treatment?

Cupping therapy, which is one of the modern physical therapy methods, has become popular as one of the complementary and traditional treatment applications in the world and in our country in recent years and is applied as a complementary treatment in different parts of the world in chronic diseases that do not respond to conventional treatment.
Although cupping therapy is applied in different ways, it is basically performed as wet (cupping) and dry cupping therapy. In both applications, the cups are placed on the skin by creating negative pressure and make room for new oxygenated blood in the extracellular space under the skin. In wet cupping (cupping) treatment, blood is taken out by scratching the skin.
Application Methods
In ancient times, horn, pottery, metal and bamboo were used as cups, but today disposable glass and PVC (hard plastic) ones are more preferred.
In cupping treatment, the cups are placed first, the skin swells with the negative pressure created and hyperemia occurs. The cups are removed after about 5 minutes. If cupping is to be performed, scratches are made in these areas and the cups are placed again by creating negative pressure and the liquid is excreted. Cupping is actually a combination of dry cupping and wet cupping.
Fire or a pump is used to create negative pressure on the applied area. It is thought that the flame will create uncontrolled pressure and cause capillary damage. The pump pressure system is a preferred method because the intensity of the vacuum is controllable.
The application technique is also very important in terms of effectiveness. The upper layer of the skin is epidermis and the lower layer is dermis. There are capillaries in the dermo-epidermal area. It is recommended that the scratches made on the skin (such as 0.1-02 mm) should be superficial, capillaries should not be traumatized as much as possible while opening the skin barrier, and especially the fluid in the interstitial area should be expelled. The amount of blood excreted during cupping varies according to the patient and the therapeutic effect is not related to the amount of blood. There are different cupping applications; in the moving cup, cream/oil is applied to the applied area, the cup is placed and moved to certain areas.
Cupping Application Types
Dry cupping – Wet cupping treatment (cupping) – Moving cupping treatment – Empty cupping treatment – Needle cupping treatment – Water cupping treatment – Hot cupping/moxa cupping – Herbal cupping, cupping massage (moving cupping)
Generally, the cups are placed on the neurolymphatic passage areas on the skin. These are the acupuncture points in Chinese medicine. Ibn Sina listed the areas where cupping is performed as follows.
- Back of the neck
- Forehead
- Between the shoulder blades
- Neck side
- Shoulder heads
- Above the calves
- Top of my head
- Under the chin
- Hips
- Knees
What should be considered before and after cupping treatment?
A protein-poor diet is recommended for one or two days before and after the application. Bathing is not recommended within 24 hours after the procedure. Since the increase in mesenteric artery circulation after a meal may reduce the blood flow to the skin, it is recommended to perform cupping on an empty stomach.
Who it is not performed for:
Age cupping (cupping) is not recommended for people with bleeding disorders, anemia, pregnant women, people with advanced heart and kidney failure, cancer patients, people under 2 years of age and over 60 years of age.
When to do it:
There is no clear information about the time in the hadiths in which the Prophet recommended cupping. However, he frequently performed cupping to stay healthy.
Due to the changes in blood pressure due to the gravitational force of the moon, it is recommended to perform cupping on the 17th, 19th, 21st and 23rd of the month according to the lunar calendar.
The amount of blood excreted during cupping varies according to the patient and it is thought that the therapeutic effect is not related to the amount of blood.
In Which Diseases Has It Been Found Effective?
Cupping therapy is used both in the treatment of diseases and in preventive medicine.
Lumbar disc lesion – Cervical spondylosis – Brachialgia paresthetica nocturnia – Persistent non-specific neck and back pain – Fibrositis – Fibromyalgia – Knee osteoarthritis – Dysmenorrhea – Thalassemia and hemochromatosis – Migraine – Trigeminal neuralgia – Carpal tunnel syndrome – Gout arthritis – Hyperlipidemia – Allergic rhinitis – Asthma – Asthmatic bronchitis – Hypertension – Heart failure – Arrhythmia and MI (a study in animals) – Herpeszoster – Viral hepatitis – Cellulitis – RA – Secondary ammonere – Stroke rehabilitation – Acne vulgaris – Atopic dermatitis
Side Effects :
Cupping therapy is a safe method without serious side effects when performed by physicians.
Side effects include iron deficiency anemia. dermatitis, herpes infection, skin pigmentation and laceration, increased pain.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is crooked neck disease (torticollis)?

A crooked neck (torticollis) is a head position caused by a contracted sternocleidomastoid (SCM) muscle that allows the neck to move laterally and anteriorly. The dramatic appearance is characterized by a tilt of the neck towards the side of the contracted muscle and rotation of the chin and face towards the opposite side.
What causes torticollis?
Congenital muscular torticollis is the most common cause of torticollis in childhood. It is usually diagnosed in the newborn or infancy. It may be due to a benign tumor of the SCM muscle or it may occur only as stiffness in the SCM muscle. In posture-related torticollis, there is no palpable stiffness or mass in the muscle. In addition to the muscular type, which is the most common type of torticollis, it may accompany some neurological diseases. It can also be seen due to visual and hearing impairments and in some internal organ diseases.
How does torticollis occur?
The most widely accepted view on the cause of congenital muscular torticollis is compression in the womb during pregnancy and childbirth. In 30-60% of torticollis cases, there is a history of difficult delivery. Compartment syndrome, which develops due to compression of the neck vessels during labor, is the main cause of the condition.
The incidence of congenital torticollis is around 3-4 per thousand. It is estimated to occur in approximately one in two hundred and fifty births. It is more common in boys and on the right side of the neck.
If appropriate treatment is not given, over time, positional flattening of the head and small face can be seen.
How is torticollis diagnosed?
Torticollis is diagnosed with a careful physical examination. The baby who presents to the doctor with a curvature in the neck should be investigated for other neurological disorders, spinal deformities, vision and hearing problems in order to differentiate them from other conditions that may cause curvature. The patient’s head and neck movements are examined. The SCM muscle is examined for stiffness, mass or shortening. The preferred imaging method is ultrasound examination of the SCM muscle. It is easy to perform and does not require anesthesia.
How is torticollis treated?
The aim of treatment in congenital torticollis is to prevent shortening of the affected muscle and to prevent future deformities by keeping the head in the appropriate position. Positioning and exercises practiced by the family play an important role in the treatment. Therefore, treatment starts with family education.
First of all, the family is informed about the condition and how the treatment and follow-up will be carried out. It is important to educate the family about positioning and transportation. The baby should be placed in bed with the normal side towards the wall, so that he/she can actively turn his/her neck in response to audible stimuli. Care should be taken to ensure that toys and audio-visual stimuli such as television are on this side. Breastfeeding and feeding should also be done on the same side, and while carrying the baby, one hand should be placed under the neck and the other arm should be passed between the legs to support the baby’s torso.
The most important part of the treatment is joint range of motion and stretching exercises, which should be done regularly, five times a day. Range of motion exercises are performed slowly and carefully by bending and rotating the neck forward, backward, sideways. Stretching exercises are performed by holding and releasing the baby’s head for 10 seconds by turning the baby’s head to the right/left and side with one hand while supporting the chest and shoulder with the other hand, and again by holding the baby’s chin with one hand while supporting the shoulder and head with the other hand and turning the baby in the opposite direction and holding and releasing for 10 seconds. Exercises should be done in 15 repetitions.
While doing the exercises, make sure that the baby’s tummy is full, comfortable and happy. Making the exercises a game by singing songs and nursery rhymes will increase the baby’s adaptation.
This exercise program should be continued for at least 1 year. In the meantime, the patient’s condition should be monitored with regular check-ups.
In patients who develop permanent shortening of the muscle and progressive asymmetry in the face due to delayed or inappropriate treatment, surgical treatment may be considered after the age of one year.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Swallowing Rehabilitation
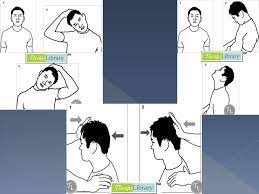
What is Swallowing?
Swallowing is a physiological function that allows food to pass from the mouth to the stomach. Many muscles and nerves are involved in this process. Swallowing generally takes place in 3 phases. The first stage is the preparation of food for swallowing with saliva and chewing. The second phase is when the food is pushed back with the help of the tongue and swallowing is triggered. The airway is closed during this phase. The last stage is the movement of the food down into the esophagus.
What is a Swallowing Disorder?
It can be defined as difficulty or absence in the transportation of food or liquids from the mouth to the stomach as a result of impairment at any stage of the swallowing process. In this case; there may be delay, obstruction or aspiration at any stage in the transportation of food to the stomach.
What is aspiration?
Aspiration is roughly defined as the passage of food or liquids into the windpipe instead of the esophagus, in other words under the actual vocal cords in the windpipe. It is very important to prevent aspiration, which can cause many problems, especially serious lung infections and even death.
Why is swallowing disorder treatment important?
In addition to negatively affecting the patient’s daily nutritional activities, it can increase the risk of life-threatening saliva aspiration and lead to malnutrition.
What are the Causes of Swallowing Disorder (Dysphagia)?
Swallowing problems can occur due to many diseases in every age group from newborns to the elderly. Stroke, traumatic brain injury, Parkinson’s, brain tumors, motor neuron diseases and progressive neurological diseases are among the leading causes of swallowing difficulties.
What are the Symptoms of Swallowing Disorders?
Coughing during or after eating or drinking, voice change during or after eating or drinking, needing more effort or time than necessary for chewing or swallowing, solid or liquid food leaking from the mouth or sticking to the inside of the mouth, chest congestion after eating, weight loss due to not eating enough food.
How is Swallowing Disorder Diagnosed?
In patients with dysphagia, the disease causing the dysphagia, physical examination and neurological examination of the patient, followed by special swallowing evaluation and further examinations (videofluoroscopy) may be needed both to identify the factor causing the dysphagia and for the treatment plan.
How is swallowing disorder treated?
Depending on the underlying disease, the cause of the dysphagia and the severity of the problem, different treatment methods can be tried. These methods range from changing the consistency of food, changing the time of feeding, changing food volumes, improving the structures around the mouth with sensory-motor development techniques and teaching special position techniques and special swallowing maneuvers. If the patient cannot be fed safely and effectively, tube feeding methods are tried. This is not a treatment method, but a strategy to protect the patient from adverse clinical pictures (dehydration, malnutrition, aspiration, etc.). Nasogastric tube feeding (nasal feeding) should be recommended in uneventful swallowing difficulties that are expected to improve in 3-4 weeks, and gastric tube feeding should be recommended in swallowing difficulties that are slow to respond to treatment and last longer than 1 month.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is dry needling treatment?

In general, the treatment performed by inserting needles, which are also used in acupuncture treatment, into trigger points and taut bands in muscle and connective tissues is called dry needling treatment. The term dry stems from the fact that no medication such as steroids, local anesthetics, mesotherapy products are administered to the body. It is generally used in painful conditions of the musculoskeletal system. There are many scientific studies on its effectiveness.
What is the mechanism of action of dry needle therapy?
The most important theoretical but generally accepted theory was made in 1977. According to this theory, trigger points are mostly related to nerve-muscle junctions and stimulation of these areas with a needle causes too much information to enter the central nervous system, which causes the painful stimulus inputs to the central nervous system, i.e. the brain and spinal cord, to be closed. The most important point here is that these conditions, which are popularly described as “earache” or “wind”, mimic the much more serious conditions of herniated discs and pinched nerves, and can be treated simply with a dry needle, which is virtually side-effect-free. For this reason, the differential diagnosis and evaluation of the physician is of great importance. Its effectiveness is around 70% in scientific articles. It is obvious that this rate will increase with the right patient selection and the right application technique.
What is the difference between acupuncture and dry needling treatment?
A similarity of up to 71% has been found between painful trigger points in the musculoskeletal system and acupuncture points. In traditional medicine and acupuncture treatment, these painful points are called “Ah-Shi (roughly translated as sore points) points”. However, acupuncture treatment is more widely used and is based on the energy flow in the 12 meridians in the body and their disorders, whereas dry needling treatment is used for musculoskeletal disorders.
Which diseases is dry needling therapy used for?
- Myofascial pain syndrome
- Fibromyalgia
- Tennis / Golfer’s elbow
- Headaches
- Arthroses are the main diseases.
Are there any side effects of dry needling treatment?
Side effects are very few. However, depending on the application technique, undesirable situations can be seen from benign side effects such as local pain, foreign body reaction, infection to serious side effects such as pneumothorax. For this reason, we strongly recommend that it be performed in competent hands and in health institutions authorized to perform this treatment.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Congenital Brachial Plexus Injury?
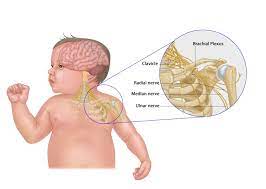
Birth is the shortest but most challenging journey of a human being. In those few minutes, we may encounter problems that determine our future, we may be battered and even lose our lives before we even start. If we have encountered difficulties but managed to survive, one of the problems we may encounter is ‘Congenital Brachial Plexus Injury’, which is defined as the damage to the plexus that comes out of the vertebrae in the neck region and forms the nerves of the arm. The damage here affects the shoulder blade, shoulder and arm muscles. Nerve damage can lead to muscle weakness in the arm or hand. Limitation of arm and hand movements occurs on the affected side. There is loss of sensation in all or some parts of the arm. Arm mobility varies depending on the type and severity of the damage.
What is Brachial Plexus?
The brachial plexus is a network of nerves located on both sides of the neck that provides movement and sensation of the shoulder, arm and hand. It has a complex anatomical structure. The nerves to the arm exit the spinal cord and pass between the vertebrae in the neck. There are four cervical nerve roots (C5-C8) and one thoracic nerve root (T1) in this nerve network. These roots merge into three trunks. The C5-C6 roots form the upper trunk, the C7 root forms the middle trunk and the C8-T1 roots form the lower trunk. Each trunk is divided into a section. Half of the sections generally move the flexor muscles (muscles that bend and raise the arm) and the other half move the extensor muscles (muscles that extend and lower the arm).
What Causes Congenital Brachial Plexus Injury?
During labor, the brachial plexus is under the influence of two forces. One of these is intrauterine pushing pressure and the other is traction applied by the clinician. Until recently, congenital brachial plexus injury was thought to develop as a result of excessive traction on the baby’s neck. However, it is now known that it can occur without traction or risk factors.
What are the Risk Factors for Congenital Brachial Plexus Injury?
Maternal risk factors:
- Maternal diabetes
- Maternal obesity or excessive weight gain
- Advanced maternal age >35 years
- First birth
- Pelvic anatomy disorder
- Uterus anomaly
- History of previous brachial plexus injury
Infant risk factors;
- Large baby (>4 kg)
- Breech protrusion, especially in small babies
- Shoulder dystocia is the failure of downward traction of the head to deliver the shoulders followed by additional maneuvers. Shoulder dystocia increases congenital brachial plexus injury approximately 76-100 times and is present in 50% of patients.
Congenital risk factors;
- Prolonged pregnancy
- Prolonged 2nd stage of labor
- Induced labor
- Assisting childbirth
- It is also seen after cesarean section. No risk factor was found in 30% of infants with congenital brachial plexus injury.
What is the Prevalence?
The frequency is reported to be 1-3 per 1000 live births. It is generally unilateral, more common on the right side.
What are the Clinical Involvements?
Upper trunk involvement (Erb-Duchenne): It is the most common type. Mostly C5-C6 spinal nerves are affected, but C7 may also be damaged. Babies with this type of injury cannot move their shoulders and have difficulty extending and rotating their arms. They have low shoulders and are described as having a tipper’s hand. Although there is often no activity in the arm immediately after birth, hand and finger movements may begin within a few weeks.
Lower trunk involvement (Klumpke): Isolated lower trunk injury is rare. C8-T1 nerves are affected. It may occur with pulling the arm up. This type of injury results in weakness in the hand and wrist, but shoulder and arm movements are usually preserved. Rarely, if the cervical sympathetic chain is also damaged in lower trunk involvement, Horner’s syndrome may develop. In Horner’s syndrome, the iris muscles that control the size of the pupil cannot function, and one eye appears smaller than the other.
Total (complete) involvement: In this type of injury, the upper, middle and lower trunks of the brachial plexus are involved to varying degrees. C5-C8 nerves are involved. In these babies, weakness occurs in shoulder, arm, hand and wrist movements. Claw hand, looseness in the arm and absence of sensation are remarkable on physical examination.
How is it evaluated?
The diagnosis is generally based on clinical findings. Especially in infants with risk factors, specialized physicians should be consulted in the presence of unilateral loss of movement and weakness in the arm. Evaluation may be performed to differentiate from other causes of arm weakness and to confirm the diagnosis. Cold dry skin on the affected arm indicates sympathetic dysfunction. Fractures, especially clavicle fractures, should be examined. In addition, the presence of problems that may accompany brachial plexus injury such as facial paralysis, torticollis, intraocular hemorrhage should be checked.
What are the necessary tests?
Shoulder, neck, chest, elbow radiographs
Shoulder MRI MRI examinations performed acutely and as early as possible make it easier to differentiate the type and location of the injury.
EMG: It is important to perform EMG in the first 7-10 days in patients with strong suspicion in order to provide information about the process, to select appropriate patients for surgery early, and to prevent unnecessary early surgery. In other patients, it should be performed in the first 3 months, at the earliest in the 1st month. EMG intervals are determined according to the severity of the lesion.
What is the Clinical Course?
Spontaneous recovery is observed in 80% of cases in the first 3 months. Complete recovery is observed in 60-70% of patients. Mild weakness is observed in 11%, moderate weakness in 9% and severe weakness in 14% of patients. However, it may vary according to the severity of the injury and the degree of involvement.
What are the Treatment Options?
Treatment should be started immediately after diagnosis. Rehabilitation and surgical methods can be used alone or in combination. One treatment does not eliminate the need for another treatment. To achieve the best results, a team consisting of the family, pediatrician, physical medicine and rehabilitation specialist, physiotherapist, orthopedist and neurologist should work together.
Aims of rehabilitation:
- Reducing joint stiffness in the affected arm
- Giving information to the family about the positioning of the affected arm
- Ensure active use of the affected arm
- Increasing and strengthening the baby’s arm movements
- To ensure that they acquire age-appropriate movements and skills
- Maintaining the mobility of the joint and preventing joint deformities that may develop
Elements of rehabilitation treatment:
- Family education
- Positioning
- Range of motion exercises
- Acquiring certain movements and behaviors through purposeful games
- Physical therapy modalities and devices
Family education
The family is provided with the necessary information; the control, follow-ups and stages of treatment and the different treatment options are explained. Training is given for regular practice of exercises at home. Range of motion exercises should be performed 3-5 times a day to prevent stiffness and deformities in the joints. The shoulder should not be lifted more than 90 degrees for the first 3 weeks. Exercises can be done during breastfeeding or diaper changes. The baby’s arm should be moved at maximum range of motion without pain and resistance. The patient should be evaluated every 2-4 weeks.
Positioning and dressing
The child should be placed on the abdomen, sides and back while awake and the affected arm should not be under the child or hanging sideways.
The baby should not be held under the armpit when being moved, and a towel is used to support the affected arm when being carried.
When the patient’s head is in any position, it should be kept in the midline and a c-shaped pillow should be used.
The child should not be lifted by holding the arms. To prevent overstretching of the affected arm, priority should be given to the affected side when dressing and to the healthy side when removing clothing.
In bathing, the affected shoulder and scapula should be supported with one hand and the baby should be bathed with the free hand.
During feeding, the affected arm should be held bent at the baby’s breast and the mother should be instructed to feed the baby from both sides
Other treatment options in the field of rehabilitation
Electrical stimulation: It is applied to specific muscles with electrodes placed on the skin to increase muscle mass and prevent muscle atrophy. The treatment can be applied by physiotherapists or family members at home with portable devices in patients deemed appropriate by physicians.
Kinesiologic taping: It is applied on the skin in certain areas by a physician/physiotherapist who has sufficient experience in the field to support the functions of the muscles around the shoulder. It can be applied together with other treatment methods.
Botulinum toxin injection: It is a substance obtained from a strong poison secreted by a bacterium that prevents impulses from the nerves from passing to the muscles. The force of contraction of a muscle injected with botulinum toxin is reduced or completely lost in proportion to the dose of the drug. The effect of the drug starts a few days after the injection and usually lasts approximately 3-6 months. Therefore, the injection may need to be repeated every 3-6 months to maintain the effect. The dose is adjusted by the physician according to the child’s age and weight and injected into the appropriate muscles.
Compulsory use therapy (CIT): Movement of the healthy upper limb is prevented with the help of gloves or a sling. The affected upper extremity is included in the RT program for 90% of working hours or 6-8 hours/day. The treatment can be administered under the supervision of a physiotherapist or family, with the child performing prescribed tasks.
Use of orthosis: It is generally used with the aim of positioning the arm after surgical interventions. Devices recommended by the physician may be suitable for this purpose.
When Is Surgery Performed?
It can be planned in cases of total paralysis or if the targeted functions of the muscles are not gained despite a certain period of time after being included in an effective rehabilitation program. Surgical procedures can be performed by a specialized plastic surgeon or orthopedic surgeon using muscle/nerve repair or muscle/nerve grafting methods. For congenital barakial plexus lesions, most autologists recommend neurolysis, nerve grafts, nerve transfers at 3 months if there is no improvement in the shoulder and elbow. Tendon transfers are usually preferred after 24 months.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is vertigo?

Although it is generally caused by upper respiratory tract infections, vertigo attacks can also occur due to genetic, traumatic and certain medications. It is not correct to consider the word vertigo as a disease term. Vertigo is a symptom. There are many diseases that cause vertigo, the most common causes of which are the balance organ in the ear, the central nervous system (damage to the brain), proprioception (the sense of perception of the position, position and movement of the joints in space) and visual impairment. Vertigo may be accompanied by physiological symptoms such as nausea, sweating, headache, as well as discomfort in crowds, fear of heights, motion sickness, sensitivity to light or discomfort in complete darkness, and finally social isolation by being afraid to go out.
How is vertigo treated?
The treatment of acute vertigo attacks has two components. The first is to control acute attacks and the second is to accelerate recovery and prevent new attacks. No ideal drug has yet been found in the treatment of vertigo. The drugs used are mostly for symptomatic treatment aimed at controlling acute symptoms and autonomic complaints. Specific treatment lies in addressing the underlying cause of vertigo.
Exercise programs are used for vertigo due to peripheral vestibular disorders. For this purpose, vestibular rehabilitation is applied.
What is Vestibular Rehabilitation?
Vestibular rehabilitation is performed to accustom the patient to dizziness with repetitive movements and to reduce dizziness. Depending on the cause, it is possible to reduce the patient’s complaints and accelerate recovery with the rehabilitation program. Vestibular rehabilitation exercises are postural control exercises, visual-vestibular interaction and conditioning activities that include getting used to the pathological response and can be summarized as gaze stabilization exercises (viewing exercises), visual exercises, somatosensory exercises, posturography training. The exercises are recommended to be performed 2 times a day for 4-6 weeks. These exercises and maneuvers are organized and applied according to the individual. The aim of vestibular rehabilitation is to reduce dizziness, to make the person feel safe, to prevent problems in active participation in daily life, to prevent falls and injuries, and to isolate from society and to avoid additional psychological disorders such as anxiety, panic disorder and major depression.
The disease groups for which vestibular rehabilitation is appropriate are as follows:
- Bening paroxysmal positional vertigo (BPPV),
- Vestibular loss: “unilateral: such as acoustic neurinoma or vestibular neuritis” bilateral: such as gentamicin toxicity
- Vestibular problems with fluctuating course: Meniere’s syndrome, perilymphatic fistula.
- Empirically in patients with uncertain diagnosis: post traumatic vertigo, multifactorial imbalance seen in the elderly
- For desensitization in psychogenic vertigo
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Mesotherapy

Mesotherapy
What is mesotherapy and for what purpose is it used?
Mesotherapy; It was first used in sports medicine treatment by Dr. Michel Pastor in France in 1952. While it is widely used in pain treatment in Europe, it is a very effective method in the field of physical therapy and rehabilitation, although there is an opinion that it is mostly used in aesthetics in our country.
Mesotherapy is a method of injecting drugs in mixtures into the middle layer of the skin (mesoderm) with microinjection technique using special 4mm needle tips at a dose lower than the normal use dose. Local anesthetics, vitamins (B1, B6, B5, B12, vitamin C), NSAIDs (pain and edema reliever), myorelaxant (muscle relaxant), pentoxifylline (circulatory regulator) drugs used for pain mesotherapy act by removing the substances that cause pain and edema in the painful area, regulating the circulation, strengthening the connective tissue and collagen structure in the load-bearing areas of the body exposed to chronic trauma.
Who can apply mesotherapy?
Doctors dealing with pain need to be specially trained and specialized for mesotherapy applications. Mesotherapy is performed in the form of sessions at certain intervals. . In order to get good results from the treatment, the sessions should be done regularly.
What are the advantages of pain mesotherapy treatment?
Direct application to the problematic area, Local and fast effect of the drug, Combination of drugs that can increase the effect of each other, Less dosage of the drug, Less side effects due to the drug, Being a painless treatment method, Less interventional compared to many pain treatment methods, Fewer sessions and longer session intervals, Not affecting daily life and work life, Slow absorption and staying in the area for a long time.
For which conditions is mesotherapy used?
Pain mesotherapy can be used for many problems such as muscle and joint pain, rheumatic and degenerative diseases (arthritis), ligament and tendon injuries, meniscus, trigger finger, neuralgia (nerve origin pain).
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Meniscus Tears
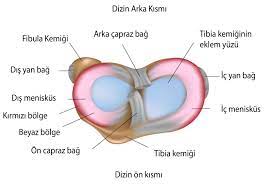
In the knee; there are two menisci, one on the inside (medial meniscus) and one on the outside (lateral meniscus). These structures provide ease of movement in the knees, one of the most mobile joints of the body, and increase the contact surfaces of the shin and thigh bones with each other, allowing the body weight on the bones to be distributed evenly. It also absorbs the shock force that occurs in the knee area as a result of a sudden impact and allows the internal knee fluid to spread to the articular cartilages.
Meniscus tears can happen to many people, especially athletes. Such as those who carry heavy loads, those who are constantly standing, housewives who are commonly engaged in housework, the elderly…
Since the medial meniscus is more immobile, it is more likely to tear. Lateral meniscal tears are more common in acute injuries that cause anterior cruciate ligament tears. Medial meniscus posterior horn tears are more common in elderly patients.
What are the Symptoms of a Meniscus Tear?
The first symptom of a meniscus tear is pain. The pain usually manifests itself in knee-bending movements such as climbing up and down stairs, using the toilet and praying. Depending on the size of the tear, it is accompanied by complaints such as locking, snapping, popping, clicking and swelling in the knees. Some patients may complain of pain when descending stairs.
Pain when pressing on the joint line on the side of the injured meniscus is the most sensitive examination finding. Fluid may be seen in the joints during the examination. Tests such as Mc Murray, Apley can be used in the examination.
If there is a meniscus tear and additional injury complaints in the examined patients, MRI examination is requested for detection.
How is a meniscus tear treated?
In sudden injury, the knee should be rested, ice application and compression, and elevation of the leg should be done in the beginning. In the long term, movement should be regulated, non-steroidal painkillers should be used and the patient should be taken to physiotherapy.
When necessary, patients can use crutches and the knee can be casted up to the ankle for 4-6 weeks. Patients should start isometric exercises to strengthen the muscles around the knee and hip after 4-6 weeks.
Surgical treatment is usually used in young patients and for vertical congitudinal tears in the outer third of the meniscus with good vascularization.
The patient’s age, general health status, lifestyle and the location of the meniscal tear are taken into consideration when choosing the surgical method. Partial meniscectomy is a commonly used method.
How is Physical Therapy Performed in Meniscal Tears?
An exercise program is effective in reducing symptoms in all meniscal tears, with or without surgery.
In the first weeks, the aim is to increase the range of motion and reduce pain and swelling. Static stretching exercises are performed to prevent atrophy of the thigh muscles and electrical stimulation may be given. When the patient starts to tolerate, active range of motion exercises are started.
Early and appropriate rehabilitation program after partial meniscectomy plays an important role in functional recovery.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Replacement Rehabilitation

Hip replacement surgery involves replacing the damaged joint with an artificial joint in patients whose hip joint has been damaged for certain reasons. Hip replacement relieves pain that has not responded to non-operative treatments, provides stability (after hip fractures and dislocations) and increases the range of motion, resulting in safe movement.
When is a hip replacement needed?
- If there is severe wear and tear in the joint due to osteoarthritis (calcification)
- In the presence of rheumatic diseases such as rheumatoid arthritis or ankylosing spondylitis that completely restrict the movement of the joint
- In cases of circulatory disorders in the head of the thigh bone
- In advanced stages of congenital hip dislocation
- In bone tumors
- Patients with residual damage after hip joint infection may need a hip prosthesis.
Preoperative rehabilitation in hip replacement
To increase the success of hip replacement, it is important to start rehabilitation before the operation. For this
- Strengthening exercises for the abdominal and back muscles
- Strengthening exercises for the hip and knee muscles
- Achievement of maximum pain-free range of motion
- Teaching postoperative walking program
- Teaching breathing exercises and coughing method to prevent pulmonary complications and to ensure secretion removal
- Strengthening of the gluteus medius muscle of the hip is necessary to avoid weighting the prosthesis.
- It is also of great importance to teach positions that prevent hip dislocation, transfer and walking activities and exercises of the first postoperative day.
Rehabilitation after hip replacement surgery
Mobilization of the patient on the 1st and 2nd postoperative day, especially with a wheelchair, is very important. In patients with cemented technique, full weight can be given with crutches for 6 weeks and with a cane between 4-6 months. In uncemented techniques, toe walking can be practiced for 6-8 weeks, partial weight bearing walking for 8-12 weeks, and full weight bearing walking after the 12th week. It is important that the patient undergoes this rehabilitation process under the supervision of a physical therapy and rehabilitation specialist and a specialized physiotherapist. The rehabilitation program is tailored to the patient:
In the first week, after positioning, prevention of deep vascular occlusion and measures to improve lung function, active or actively assisted flexion-extension exercises for the hip joint, isometric exercises for the hip and knee muscles, sitting on a high chair, walking with a walker, strengthening exercises for the abdomen, back and limbs should be performed.
In the second week, it is important to teach exercises that increase joint mobility and muscle strength in the hip, transition to crutches when walking independently with a walker is achieved, stair activities, and situations to be considered during activities of daily living.
Important points for patients with hip replacement
Lying down;
- Do not lie on your side on the operated hip
- Do not cross your legs, do not cross them
- Keep a pillow between your legs
- Lie flat on your back for at least 30 minutes a day
- Do not put a pillow under the prosthetic leg
Sitting;
- Do not sit on low chairs and armchairs
- When sitting, the knee level should not be lower than the hip
- Use a toilet riser
- Do not lean forward when sitting
- Do not cross your legs
Standing;
- Don’t bend down to pick something up
- When you bend down, your hand should not exceed knee level
- Do not turn your foot inward
- Do not bend more than 80 degrees when putting on pants, socks, shoes and use long-handled dressing aids
- When climbing stairs, follow the sequence of good leg – operated leg – crutches. Remember that the reverse is true when descending stairs.
Recommended sports: Swimming, cycling, golf, dancing, aquatic aerobics
Sports not recommended: Running, jogging, sports that require turning and sudden movements on a fixed foot, contact sports, heavy work.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
How does an ankle sprain occur?
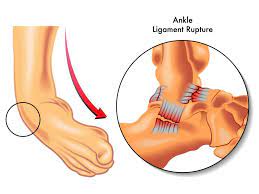
The ankle joint is one of the most commonly injured joints. The ankle joint is the joint that connects the leg to the foot. This joint is formed by three bones: These three bones are connected by very strong ligaments. These ligaments prevent the foot from making abnormal movements such as twisting and spraining. The outer lateral ligaments are located on the outer side of the ankle and prevent the ankle from moving inwards. The inner lateral ligaments are located on the inside and prevent the ankle from turning outwards. Ligaments are flexible structures. However, there may be tears in the elastic fibers of these ligaments after excessive strain.
External side ligament injuries are the most common injuries.
Sports injuries account for 15% of ankle injuries. Basketball, volleyball and soccer are the sports branches that pose the most risk. Ankle injuries can occur not only after sports activities but also during daily activities. Usually, ligaments may tear as a result of turning the foot inward or outward on an uneven surface. Looseness occurs in the joint due to incompletely healed and neglected ligament tears. This causes the foot to sprain again. If no protective measures are taken, sprains may recur frequently. Thus, the joint cartilages deteriorate.
When the foot sprain is called stage 1, there is no rupture of the ligaments, but stretching is seen, there is water collection (edema) around the ligament In stage 2, the ligaments are partially torn. As a result of the examination, it is determined that there is laxity in the ankle. In stage 3, it may not be possible for the ligament to heal on its own because it has ruptured. Surgical procedure may be required in the treatment of foot sprain in stage 3.
What are the symptoms of ankle sprain?
Swelling around the ankle occurs due to bleeding and edema after an ankle sprain. Ankle movements are painful. Although it is usually painful, the patient can step on his/her foot. A few days after the sprain, bruising can be seen where the swelling is due to the bleeding that occurs.
How to treat foot sprains?
In sprains, a doctor should be consulted without losing time. In the first stage, the aim is to relieve pain and reduce swelling. Ice application is the most effective method to reduce pain. It also contributes to the healing process by reducing edema and swelling. It is inconvenient to put ice directly on the skin. It is more appropriate to put it on a towel. Ice application is done for 20 minutes and this period can be repeated at 30 minute intervals. Rest; If possible, the injured ankle should not be stepped on for two to three days. Crutches can be used during this period. Elastic bandage Elastic bandage wrapped starting from the toes, provided that it is not too tight, helps to reduce swelling. Keeping the leg elevated; It is necessary to keep the foot above the chest level as much as possible for two to three days. This application also helps reduce swelling. Painkillers; Depending on the degree of pain, simple painkillers or drugs that have both painkillers and edema-reducing effects can be used. Ankle bracelets; Special ankle bracelets for sprains can be used to support the ankle during the healing process and to reduce pain. These allow the ankle to move up and down but prevent sprains. Sports can be done with some of them.
How does the healing process progress in ankle sprains?
When the foot sprain is called stage 1, there is no rupture of the ligaments, but stretching is seen. In the treatment, the patient’s foot is wrapped in an elastic bandage, it is recommended to rest and not walk too much. At the same time, ice application should be continued. The foot sprain usually heals within three weeks. In stage 2, the ligaments are partially torn. As a result of the examination, it is determined that there is laxity in the ankle. Depending on the degree of the injury, partial plaster, splint or special ankle braces can be applied. In this way, the patient’s ankle remains immobilized and the healing of the ligaments is accelerated. In addition, anti-edema and painkillers are given. If the patient rests for a sufficient period of time, the recovery period takes 3-6 weeks.
In stage 3, it may not be possible for the ligament to heal on its own as it ruptures. In the treatment of a foot sprain in stage 3, the ruptured ligament needs to be repaired or a ligament from elsewhere can be transplanted. Because the ligament is completely severed, the foot takes longer to heal after surgery.
After an ankle sprain, complaints such as pain and swelling usually subside within two weeks. After the painful period has passed, it is necessary to start practicing ankle movements in order to prevent any limitation in ankle joint movements in the future. Physical therapy support should be received during this period.
The recovery rate after ankle sprains is between 80-90% and surgical treatment is rarely required. However, it takes four to six weeks for the ligaments to heal completely. New strains that will occur before the ankle ligaments are fully healed will negatively affect the healing of the ligaments and create a basis for recurrent sprains in the future. Another cause of recurrent sprains is the deterioration in muscle balance due to muscle weakening. Recurrent sprains cause a feeling of insecurity and chronic pain in the ankle.
What can be done to avoid ankle sprains?
Heeled and uncomfortable shoes should not be worn, even if they are to be used, shoes that wrap the foot from the ankle should be preferred, Using special ankle bracelets during sports in cases of recurrent sprains, Warming up well before exercise Pay attention to the ground on which sports are done or walked Strengthening the muscles around the ankle.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Lateral Epicondylitis (tennis elbow), Medial Epicondylitis (golfer's elbow)?
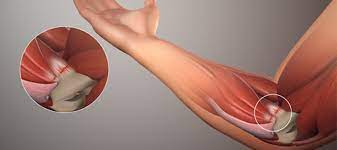
Lateral epicondylitis is often known as tennis elbow. It is a painful condition that occurs on the outside of the elbow where the muscle-tendon attaches to the bone. Tendons connect the muscle to the bone. The muscle associated with this condition is the extensor carpi radialis brevis. In lateral epicondylitis, there is degeneration and weakening of the tendon attachment site. It can cause pain in relation to movements in which this muscle is active (stretching, gripping, etc.). medial epicondylitis Golfer’s elbow is characterized by pain and tenderness in the bony prominence on the inside of the elbow. The tendons of the arm muscles responsible for bending the wrist attach to the medial epicondyle. Golfers’ elbow can occur due to overuse of these muscles. When the muscles are overused, the tendons are subjected to repetitive pulling force in the area where they attach. As a result, inflammation and small tears occur in the tendons, which causes pain.
Who has Lateral Epicondylitis (tennis elbow)?
Sports such as tennis are often associated with this condition. It is common between 30 and 50 years of age, but can also occur in younger and older people. Golfer’s elbow is most common in men between 20 and 49 years of age.
What Causes Lateral Epicondylitis (tennis elbow) and Medial Epicondylitis (golfer’s elbow)?
Overuse Activities that cause stress at the attachment site of the tendon increase injury to the tendon. These stresses can be repetitive holding, gripping activities, chopping, painting, twisting, squeezing.
Trauma: Injury can also occur with a sudden unexpected movement, force and activity.
What are the Symptoms of Lateral Epicondylitis (tennis elbow), Medial Epicondylitis (golfer’s elbow)?
The main reason why patients need treatment is pain. Pain is localized on the protruding bone known as “lateral epicondyle” on the outside of the elbow in tennis elbow. In golfer’s elbow, pain is felt on the inner (medial) side of the elbow. This area is tender to the touch. The pain may also increase with movements that place stress on the tendon (such as gripping, stretching, bending). The pain starts at the elbow with activity and may spread from the forearm to the hand. Sometimes there may be pain without any movement.
What are the Treatment Methods for Lateral Epicondylitis (tennis elbow) and Medial Epicondylitis (golfer’s elbow)?
Activity regulation: Activities that cause this condition should be restricted. Restriction of strenuous activities is recommended rather than complete rest. Modified holding techniques, using both hands during activity may reduce the problem.
Medication: Anti-inflammatory (pain and edema relieving) treatment helps to reduce pain.
Brace: The brace is worn over the posterior forearm muscles and below the elbow. The elbow brace reduces the tension on the tendons and allows healing.
Physical therapy: Doing strengthening and stretching exercises can help recovery. Especially when the elbow is fully extended, stretching the wrist can be beneficial. Ultrasound and heat treatments can also be used for physical therapy.
Injection: Steroid is a powerful anti-inflammatory that can be injected locally. It should not be done more than three times in 3-month periods. It is done in sessions
Pain mesotherapy: It is the injection of drugs in mixtures into the middle layer of the skin (mesoderm) with microinjection technique using special 4mm needle tips at a dose lower than the normal use dose. Mesotherapy is performed in sessions with certain intervals.
Surgery: Surgical treatment should be considered if the person becomes unable to perform daily activities and work due to pain and has not benefited from non-surgical treatment for more than 6 months. Surgical treatment involves removing diseased, degenerated tendon tissues. Physical therapy after surgery helps to restore the arm’s movements. Strengthening programs will be necessary to regain old activities.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What are Inflammatory Joint Rheumatisms?

Inflammatory joint rheumatism is a general term and not a single disease; there are nearly 200 rheumatic diseases. Of these, inflammatory rheumatism is the most common;
- Rheumatoid Arthritis (RA),
- Spondyloarthropathies (SpA) (such as Ankylosing Spondylitis (AS), Psoriasis Rheumatism (PsA), Reactive Arthritis and arthritis due to Inflammatory Bowel Disease),
- Connective Tissue Diseases (Systemic Lupus Erythematosus and Sjögren’s Syndrome etc.).
- In addition, diseases such as Behçet’s Disease, Familial Mediterranean Fever (FMF) and Gout are also defined as “inflammatory” rheumatic diseases.
What Causes Inflammatory Joint Rheumatism?
Most of these types of diseases are autoimmune and immune system-induced diseases. Most of these inflammatory ones are known for the mechanisms by which the immune system and / or inflammatory mechanisms work inappropriately and the body creates a disease against itself. Most diseases caused by a genetic predisposition are triggered by an external factor. Joint pains and symptoms that can cause permanent damage to the body can develop.
What are the general symptoms of inflammatory rheumatism?
- Swelling in the Joints
- Joint Pain
- Limitation of movement in the joints
- Morning stiffness
- Low back/hip or back pain (if there is inflammation of the spine such as spondyloarthropathy)
- Loss of function in joints
- Skin Rashes or Dry Eye (in Connective Tissue Diseases)
- Recurrent sores/shafts in the mouth (Behçet’s Disease)
- Recurrent Abdominal Pain and Fever (FMF/Familial Mediterranean Fever)
- Inflammatory rheumatism of the big toe (Gout)
Which Department Treats Inflammatory Joint Rheumatism Diseases?
A rheumatologist (rheumatologist) provides services for rheumatic diseases. A rheumatologist is a doctor who specializes in the diagnosis and medical treatment of arthritis and other rheumatic diseases. In a more limited sense, a rheumatologist is a doctor who has completed a specialization in internal medicine (5 years) followed by training in rheumatology (3 years); a rheumatologist focuses on diagnosing rheumatic disease before treating it. “Inflammatory joint rheumatism” is a general term and refers to all types of arthritis and rheumatism. In addition to inflammatory systemic (involving the whole body) and joint-specific rheumatic diseases, degenerative, metabolic and mechanical musculoskeletal problems also fall within the specialty of the Rheumatologist. Since the rheumatologist is an internal medicine specialist, he/she has the infrastructure to solve most of the internal organ (heart, kidney, lung, liver, gastrointestinal tract, etc.) problems that can be seen frequently in rheumatism patients due to the disease itself or treatments.
How is Inflammatory Joint Rheumatism Diagnosed?
First of all, the rheumatologist inquires about the medical history and complaints and takes an anamnesis. He or she then focuses on the Physical Examination, not only physically examining the joints, but also paying attention to systemic findings that may affect the whole body. Often, a single test is not enough to make a definitive diagnosis of inflammatory rheumatism. The rheumatologist may order several blood tests or imaging tests (X-ray, ultrasound or MRI) to confirm the clinical findings and to confirm the diagnosis.
What are the tests for inflammatory rheumatism?
- Rheumatoid Factor (RF): High levels (positive) of rheumatoid factor are associated with autoimmune diseases, especially inflammatory rheumatism.
- Anti-Citrullinated Cyclic Peptide (Anti-CCP) Antibody test: A positive anti-ccp antibody in combination with RF confirms rheumatoid arthritis and provides prognostic information. Individuals with this antibody are generally considered to have rheumatism.
- Anti-Nuclear Antibody (ANA) test: This test is done to see if the body produces autoantibodies, the presence of which highlights a possible autoimmune disease and consideration of Connective Tissue Disease.
- Anti-ds DNA Antibody: An autoantibody specific for Systemic Lupus Erythematosus.
- Anti-SSA/SSB Antibodies: An autoantibody test that appears in the Connective Tissue Disease known as Sjögren’s Syndrome.
- HLA-B27 Genetic Testing:
- Erythrocyte Sedimentation Rate (also known as Sedim or ESR): Helps to determine the level of inflammation in the body. It is usually high in inflammatory joint rheumatic diseases, but may not always be high.
- C-Reactive Protein test (CRP): Like the ESR, it detects the presence of a serious infection or inflammatory rheumatism somewhere in the body. High levels of CRP in the blood are usually elevated in patients with inflammatory joint rheumatism, but like ESR, it may not always be elevated despite the presence of rheumatism.
Is there a cure for inflammatory rheumatism?
In general, there is no treatment that completely cures inflammatory rheumatism, but there are many treatments that can put the disease into remission, reduce joint pain and improve quality of life. The priority of the rheumatism specialist is always to reduce and prevent inflammation in the body. Reducing inflammation helps prevent permanent damage to both joints and internal organs. Different medications and various methods are used to treat inflammatory rheumatism. Some of these include;
- Cortisone and non-cortisone anti-inflammatory drugs,
- Classical medicines for inflammatory rheumatism (DMARDs) that change the course of the disease: especially those containing Sulfasalazine, Hydroxychloroquine and Methotrexate,
- Biologic Agents (bDMARDs): This new generation of rheumatism drugs is often used in people who do not respond to conventional rheumatism drugs and is very effective in reducing inflammation,
- Complementary Medicine Methods (e.g. Ozone Therapy, Laser Treatments)
- Pilates, Hydrotherapy, Aqua/Pool Treatments and Exercise types performed under the supervision of a Physical Therapy and Rehabilitation and PTR specialist,
- Special Nutrition
What is needed for successful treatment of inflammatory rheumatism?
Early diagnosis is very important for successful treatment of rheumatism. Early diagnosis requires a long examination process and follow-up of the patient. Because the symptoms change during the period when the complaints decrease or increase. The type of treatment varies from person to person and each patient should be treated differently. Long-term treatment may be required as a result of chronic diseases. As a result of medication and physiotherapy under the supervision of a doctor, the disease cannot be completely eliminated, but its progression is stopped and the patient’s life is made easier by relieving pain.
In drug treatment, drugs are used to relieve the patient’s pain, to stop the disease or to relieve swelling and pain. These drugs affect the inflammation caused by rheumatism. In addition, muscle relaxants, vitamin supplements and blood pressure lowering drugs are used to eliminate other symptoms. These medicines should be taken with plenty of water. It should also be noted whether there are side effects (some drugs can prevent pregnancy). Rheumatism treatment methods include medication, intra-articular injections, physical therapy and surgery. The most important aspect of a rheumatologist’s role and service is to manage which treatment, when, how and for how long. Therefore, treatment options should be made under the direction of a rheumatologist.
What are the Types of Inflammatory Rheumatism?
The most common inflammatory rheumatisms;
- Rheumatoid Arthritis (RA),
- Spondyloarthropathies (SpA) (such as Ankylosing Spondylitis (AS), Psoriasis Rheumatism (PsA), Reactive Arthritis and arthritis due to Inflammatory Bowel Disease),
- Connective Tissue Diseases (Systemic Lupus Erythematosus and Sjögren’s Syndrome etc.).
- In addition, diseases such as Behçet’s Disease, Familial Mediterranean Fever (FMF) and Gout are also defined as “inflammatory” rheumatic diseases.
What is Rheumatoid Arthritis (RA)?
Seropositive Rheumatoid Arthritis: The most common type of inflammatory rheumatism. It can have more severe and serious symptoms than other types of rheumatism. General symptoms include swelling and pain in the small joints (fingers or wrists), stiffness in the joints for more than 30 minutes in the morning and a feeling of stiffness that decreases with movement, general weakness and fatigue. In uncontrolled patients, swelling, redness and sensations of warmth in the joints of the hands and/or wrists may also be present.
What are the diseases of the Spondyloarthropathy (SpA) group?
Spondyloarthritis or Spondyloarthropathy (SpA) is the name given to a group of rheumatic diseases. This group of diseases affects approximately one in a hundred patients in the population. The symptoms of SpA are very diverse, but they usually start in the joints we call sacroiliac joints (the joint between the coccyx and pelvis). In addition to the sacroiliac joints, the joints of the spine, peripheral joints (such as the knee, hip, shoulder and ankle), and the points where tendons and ligaments attach to the bones (especially heel and sole pain) are also involved. Patients with this group of SpA also suffer from psoriasis of the skin, inflammation of the eyes known as uveitis and inflammatory bowel disease. The main diseases in the SpA group are Ankylosing Spondylitis (AS), Psoriatic Arthritis (PsA), Reactive Arthritis and Enteropathic Arthritis (Enteropathic Arthritis) due to Inflammatory Bowel Disease.
What are Connective Tissue Diseases, especially Systemic Lupus Erythematosus (SLE) and Sjögren’s Syndrome?
What is Systemic Lupus Erythematosus?
Systemic lupus erythematosus (also referred to as SLE or just lupus) is a disease that causes different health problems. It can cause skin rashes, arthritis, anemia, epileptic seizures or psychiatric illness and often affects internal organs such as the kidneys, lungs and heart. Once a disease with a high mortality rate, it has now become a chronic (long-lasting) disease. In 1954, the survival rate after 4 years of illness was 50%; today it is over 97%.
Cause
SLE is a chronic (long-lasting) inflammatory disease caused by abnormal functioning of the immune system, which is normally responsible for protecting the body against infections and cancer. In SLE, the immune system overworks and produces large amounts of abnormal antibodies. These abnormal antibodies attack the patient’s candida tissues. The cause of lupus is not known exactly, but hereditary causes, environmental and hormonal changes are thought to play a role.
Impact on health
The prevalence of SLE is 40-50 per 100,000 people.
It is more common in some ethnic groups, for example black people.
More than 80% of people with lupus are women.
Diagnosis
- Because of the wide variety of symptoms, diagnosis is often difficult and requires the physician to be very careful. Typical features of SLE are:
- Butterfly-shaped skin blemish on the cheeks
- A skin blemish that appears on sun-exposed skin areas
- Sores in the mouth and nose
- Arthritis involving one or more joints
- Kidney inflammation
- Nervous system disorders such as epilepsy, mental illness and stroke
- Common symptoms include fever, weight loss, hair loss, poor circulation in the fingers and toes, chest pain when breathing deeply (pleurisy = inflammation of the lining of the lung) and abdominal pain.
Laboratory tests are very important in the diagnosis of SLE. In particular, the antinuclear antibody (ANA) test is always positive in SLE.
The disease can manifest itself slowly, so the final diagnosis is often delayed.
Treatment
The treatment of SLE depends on the clinical problems present and whether the disease is currently active. Earlier and more accurate diagnosis, a better understanding of the immune abnormalities in SLE and research into treatments will all contribute to improving the treatment of patients with SLE.
Regular medical evaluation is important in monitoring a patient with SLE. Medication should be adjusted for each patient according to their specific problems and the severity of the disease. If there is mild inflammation, non-steroidal anti-inflammatory drugs may help. Corticosteroids, the single most important drug in the treatment of SLE, should be used with caution. It is important to protect the bones when using steroids. Antimalarials (antimalarial drugs) such as hydroxychloroquine reduce the activity of the disease and help with skin and joint symptoms. More severe cases of SLE require immunosuppressive drugs such as azathioprine and cyclosporine. The disease often goes through periods of silence and little or no activity (remission), during which medications can be reduced and sometimes treatment can be stopped.
SJÖGREN’S SYNDROME
What is Sjögren’s syndrome?
Sjögren’s syndrome is a chronic, long-term disease characterized by symptoms of dry eyes and dry mouth.
It is named after Henrik Sjögren, the Swedish ophthalmologist who first described it.
It is often associated with rheumatic diseases such as rheumatoid arthritis, lupus erythematosus, scleroderma and polymyositis.
However, it occurs alone in about half of patients.
How does Sjögren’s syndrome develop?
The exact cause is unknown. There is evidence that genetic or viral infections can cause Sjögren’s syndrome through unknown mechanisms. It is thought that this disease is mainly caused by a disorder in the immune system. The immune system is the body’s defense mechanism against diseases. In Sjögren’s syndrome, there is a defect in the normal control mechanism of the immune system, resulting in an excessive production of white blood cells. These cells, called lymphocytes, travel to the lacrimal and salivary glands and destroy these tissues. This leads to a decrease in the secretion of both salivary glands and lacrimal glands, i.e. dryness. At the same time, these cells secrete protein substances called “autoantibodies”, which can be detected in the blood. These autoantibodies are an indication that the immune system is not working properly and have the potential to damage the salivary and lacrimal glands. Sjögren’s syndrome can also involve other organs such as joints, lungs, kidneys, nerves, thyroid, liver and brain.
Who has Sjögren’s syndrome?
Although Sjögren’s syndrome can occur at any age, it is most common in women over the age of 45. It is very rare under 20 years of age.
What are the symptoms of Sjögren’s syndrome?
It usually starts slowly. The patient feels severe dryness in the eyes and mouth. Many also have a dry cough and a tickling sensation in the throat. Swelling of the salivary glands, impaired sense of taste and smell may be observed. Eyes develop redness, burning, itching and hypersensitivity to light due to dryness. If not treated appropriately, ulcers on the outermost transparent membrane of the eye called “cornea” and rarely blindness may develop. Patients with Sjögren’s syndrome may also experience dryness in the nose, skin and female genital organs.
Dry mouth may cause difficulty in chewing, swallowing and speaking. Therefore, patients should drink plenty of fluids.
Dental caries is also common in patients. This is because saliva is a fluid that fights against bacteria and prevents cavities from forming. In Sjögren’s syndrome, saliva secretion is impaired, making it easier for cavities to form.
Sometimes patients develop a type of lymph node cancer called “lymphoma”. Although it is rare, it should be kept in mind during the examination and follow-up of patients.
How is Sjögren’s syndrome diagnosed?
This diagnosis should be suspected in patients who feel dryness in the mouth and eyes. During the examination, findings such as red and itchy eyes, swollen salivary glands, dry tongue and enlarged lymph nodes in the neck may be detected. The presence of autoantibodies in blood tests also supports the diagnosis.
Dryness in the eye is detected with the “Schirmer test”. Examination of the cornea by an ophthalmologist will also provide information about dryness.
A “sialogram” can be performed to check whether the salivary glands are working properly. This test is done by injecting dye into the salivary gland and then taking special films. For a definitive diagnosis of Sjögrens syndrome, a lip biopsy, i.e. a small piece of the small salivary glands in the lip, should be taken and evaluated under a microscope for the presence of lymphocytes.
Monitoring of lung and kidney function with both direct radiographs and laboratory tests may be helpful.
How is Sjögren’s syndrome treated?
Although there is no definitive diagnosis of this disease, patients’ complaints can be relieved and their quality of life can be improved with specific treatments for the symptoms. Since not all patients have the same symptoms, the treatment program should be planned individually by the physician according to the needs of the patient. Regular medical and dental check-ups are essential.
- Artificial tears and eye drops can be used for dry eyes.
- One of the most effective ways to relieve dryness in the mouth is to drink plenty of fluids. Special chewing gums (provided they are sugar-free to prevent decay), toothpastes and regular tooth brushing will also help patients.
- If the skin is dry, moisturizers recommended for sensitive skin can be used. It may be recommended to use steam machines that humidify the steam air at home and at work.
- Non-steroidal antirheumatic drugs may be used to prevent swelling, stiffness, muscle pain and joint inflammation. Cortisone may also be recommended in severe patients, but it is recommended to be taken under the supervision of a physician due to the severity of side effects. If patients have another rheumatic disease (such as rheumatoid arthritis, lupus, etc.), its treatment is also essential.
- Light exercises such as walking and swimming are beneficial for maintaining the elasticity of muscles and joints. Since exercises also have a preventive effect on joint damage, they should be included in the treatment program. Patients should also be given information about their disease and advice on how to reduce stress.
- A certain “antibody” in the blood of female patients with Sjögren’s syndrome is rarely associated with heart problems in newborn children. Therefore, women who are pregnant or who want to have a child should consult their doctor about this.
- Sjögren’s syndrome is generally not life-threatening. However, dryness in the mouth and eyes is long-lasting and may persist for the rest of life. The use of artificial moisturizers and attention to dental hygiene can often prevent serious problems.
BEHCET DISEASE
What is Behçe disease?
First described in 1937 by Dr. Hulusi Behçet, a Turkish professor of dermatology, Behçet’s disease is a chronic disease that causes sores (aphthae, ulcers) in the mouth and genital areas and inflammation in the eye.
In some patients, it also causes arthritis, inflammation and blockage of blood vessels, inflammation in the digestive tract, brain and spinal cord.
Behçet’s disease presents differently in each patient. In some patients, the disease is mild and there are only ulcers in the mouth and genital area.
In others it is more severe and can cause meningitis (inflammation of the membranes surrounding the brain). Severe symptoms usually appear months or even years after the first symptoms begin. Symptoms may persist for a long time or may go away in a few weeks. Typically, symptoms appear, disappear and reappear (flare-up periods).
Cause
The cause of Behçet’s disease is not known exactly. Most of the symptoms are caused by inflammation of the blood vessels. This inflammation of the blood vessels is thought to be caused by the immune system, but it is not known what initiates this reaction.
Behçet’s disease is not contagious. In addition to a defective immune system, hereditary causes are thought to play a role in its development. Environmental factors (such as viruses or bacteria) are also thought to initiate the disease in susceptible individuals.
Behçet’s disease is common in countries along the “silk road” (Mediterranean region, Turkey, Iran, Asian countries, Far East, Japan). Although it tends to start in the 20s and 30s, it can occur at any age. The “pathergy test”, which involves pricking the skin with a needle using a certain method, can be used in the diagnosis, but this test is positive in only 40% of patients.
Treatment
Although there is no cure for Behçet’s disease, it is often possible to control the symptoms with appropriate medication. The aim of treatment is to reduce symptoms and prevent complications such as disability or blindness. The choice of medication and the duration of treatment depends on the patient’s condition. Some symptoms may require a combination of several treatments to relieve them.
- Topical (local, regional) treatment: To relieve pain and discomfort, ulcers can be treated with corticosteroids to reduce inflammation or pain ointment to reduce pain. Mouthwash can be prescribed for mouth ulcers.
- Oral medications: Depending on the severity of the patient’s symptoms, corticosteroids such as prednisolone, immunosuppressive drugs such as azathioprine, chlorambucil, cyclosporine, colchicine may be prescribed. If these drugs are not effective on the symptoms, other drugs such as cyclophosphamide or methotrexate may be prescribed.
Flare-ups can occur even if treatment is effective.
What is Familial Mediterranean Fever – FMF?
Familial Mediterranean Fever (FMF) is a disease with a predominantly hereditary characteristic seen in Turkey, North African countries, Armenians, Arabs and Jews. It is known as Familial Mediterranean Fever (FMF) in the medical literature. The main characteristic of the disease is recurrent acute (sudden onset), short-term, painful attacks of peritonitis (inflammation of the peritoneum), pleuritis (inflammation of the pleura) or arthritis (inflammation of the joints), which may be accompanied by a skin rash. In some patients, the kidney may be affected and this is called amyloidosis. Rarely, kidney involvement and vascular inflammation can occur in addition to amyloidosis. Kidney involvement can lead to kidney failure.
Cause
Recently, a mutation (change) in a gene called “Pyrin” has been found in this disease, but the exact cause is not known.
Diagnosis
In patients with an attack, the diagnosis is based on clinical signs, family history, examination findings and laboratory tests. The benefit of genetic analysis in patients is limited, as mutations identified to date have only been found in 80% of patients with AAA. However, genetic analysis may be useful in atypical cases.
Treatment
Continuous treatment with colchicine 1-2 mg daily has been found to prevent attacks and the development of amyloidosis in a significant proportion of patients. However, amyloidosis is still a serious problem in patients who do not comply with treatment or who are late in starting colchicine. It is not known how colchicine prevents attacks or prevents the development of amyloidosis. In some patients treated with colchicine, the frequency of attacks does not change, while the development of amyloidosis stops. Therefore, colchicine treatment should be lifelong. Colchicine treatment is known to be a safe, appropriate and vital treatment for patients with AAA. It is recommended even if the patient becomes pregnant. Although colchicine has not been shown to have a harmful effect on the baby, amniocentesis (taking a sample from the water sac containing the baby) and genetic examination of the fetus are recommended for pregnant AAA patients.
What kind of disease is gout and is it a rheumatic disease?
Known as “the disease of kings and the king of diseases”, gout has been the subject of many studies since at least the time of Hippocrates and has affected countless people. Gout is a disease characterized by sudden, severe attacks of pain, tenderness, redness, swelling and increased temperature in some joints. It usually affects one joint at a time and this joint is usually the big toe joint. Other joints such as the knee, elbow and wrist can also be affected.
Attacks develop very quickly and the first attack usually occurs at night. It is the most painful of all types of rheumatism.
Attacks can develop for the following reasons:
- Too much alcohol intake
- Too strict diet and starvation
- Overeating of certain foods
- Having an operation (even a simple procedure such as tooth extraction can be the cause)
- Sudden, severe illness
- Excessive fatigue and worrying excessively for any reason
- Joint trauma, injury
- Administration of chemotherapy
- Taking diuretic drugs
(Diuretics are drugs used in high blood pressure, which provide fluid excretion from the body)
Remember!
If you have gout and after a minor injury or trauma your joint is very painful and takes longer than expected to heal, consider that it may be a gout attack.
Any event that disturbs your body system can trigger a gout attack. Be alert for early signs of an acute attack, because the earlier treatment is started, the better.
What causes gout?
Gout is caused by an excess of uric acid in the body. Uric acid is also present in the blood of healthy people as a breakdown product of various chemical processes.
However, an excess of uric acid is caused either by an excess of uric acid production, a low excretion rate by the kidneys or an excess intake of purines, which are converted into uric acid in the body, in certain foods. Red meat, seafood and legumes are rich in purines.
Alcoholic drinks also significantly increase uric acid levels. The view that gout is caused by eating and drinking too much is not correct. Eating too much of certain foods or gaining too much weight can make gout attacks more frequent.
Problems related to the chemical processes that uric acid undergoes in the body may be inherited in families or may occur as a complication of another disease. This problem is passed on from parents or grandparents. But environmental factors can also play a role. In addition, not every member of the family has gout attacks.
Over time, excess uric acid in the blood leads to deposits around the joints. As a result, uric acid forms crystals inside the joints that look like sewing needles, which causes gout attacks. These crystals do not only form inside the joint. Uric acid can also appear under the skin, as tofus in the earlobe and as kidney stones in the urinary tract. Tofus looks like a small, white pimple.
What are the long-term risks?
The first gout attacks do not cause permanent joint damage and your joints remain completely normal. However, if a joint is repeatedly affected by gout attacks – which is now very rare with treatment – then uric acid crystals damage the joint and chronic arthritis can develop. In mild cases, attacks are very rare and the intervals between attacks can be measured in years and no permanent damage develops.
Gout is closely associated with obesity, hypertension, hyperlipidemia and diabetes. If gout is left untreated, kidney stones can form.
How is gout diagnosed?
Since various rheumatic diseases can mimic a gout attack and treatment is specific to gout, accurate diagnosis is very important. Physical examination and medical history are very useful for diagnosis.
Your doctor may order the following investigations
Blood test. The amount of uric acid in the blood is measured. However, this result can be misleading. This is because people with gout may have normal or even low levels of uric acid. At the same time, high levels can be found in healthy people, especially obese people.
Examination of joint fluid. The synovial fluid in the joint can be extracted by your doctor with a syringe and examined under a microscope for the presence of urate crystals. If these crystals are detected, the diagnosis of gout is confirmed. This test is particularly useful if the gout starts in an atypical way. For example, gout can sometimes mimic another rheumatic disease such as rheumatoid arthritis.
Direct radiography (X-ray) of the joints. You can have a radiograph of your joints if your doctor wants, but usually the result is normal and does not help with the diagnosis.
Remember.
Repeated attacks of gout can damage your joint and cause permanent arthritis. Modern treatment methods can prevent the development of arthritis.
How is gout treated?
Acute gout attacks are treated with anti-inflammatory analgesic drugs. These medicines reduce pain and relieve inflammation. They are usually well tolerated and do not cause significant side effects, as they are only used for a short period of time in gout. However, indigestion, stomach pain, nausea, rash and headache may sometimes develop. Asthma patients should also be careful when using these medicines. People with a history of ulcers should warn their doctor about this so that he or she can consider less harmful treatment options. Aspirin and aspirin-containing medicines should be avoided during acute attacks.
Another drug used in the treatment of acute attacks is colchicine. Colchicine is very effective but can often cause nausea, vomiting and diarrhea. Intravenous administration of this medicine reduces the incidence of these side effects. If your doctor decides to give you colchicine, he or she will recommend that you take it every 2 hours until the pain goes away or you develop side effects such as diarrhea.
It will be more effective if you take your medication at the onset of an attack. It is therefore helpful to keep the medicines recommended by your doctor at home and take them until you see your doctor when an attack develops.
By following your doctor’s advice carefully and exactly, a gout attack can be controlled quickly and successfully. A painful joint such as the big toe needs to be protected. It is helpful to place a cage-like structure over the foot to protect the joint from weights such as blankets and quilts.
Medicines recommended for acute attacks have no effect on blood uric acid levels. In other words, they do not prevent new attacks or the accumulation of uric acid in the joints. Therefore, if your attacks become more frequent, if you develop tofus/kidney stones or if blood tests show high levels of uric acid, your doctor may recommend medicines to lower blood uric acid levels. Such a decision requires you to take medication every day, whether you have an attack or not. There are various medications that are used as preventive treatment for this purpose. Examples include allopurinol, which blocks the formation of uric acid in the body, and probenecid, which helps the kidneys to excrete uric acid. Depending on the amount of uric acid in your urine, you can choose between these two types of medication. With the right treatment, gout can be very well controlled in almost all cases.
Remember.
Preventive treatment lasts a lifetime.
You should drink plenty of fluids.
If an attack develops during preventive treatment, treat the attack separately.
Diet
Diet used to be believed to be more important, but since the discovery of effective treatments, many people with gout have been able to eat and drink what they want. Offal such as liver and kidneys should be avoided, as some foods have a high concentration of cells and uric acid is produced by cell destruction. Protein-containing foods (especially meat) should be eaten in moderation; a certain amount of these foods is beneficial for everyone, not just gout sufferers. If you are overweight, losing weight is not only good for lowering urate levels in the blood but also for your heart. However, too strict dieting and starvation can also trigger attacks.
Alcohol
Drinking excessive amounts of alcoholic beverages is not the cause of gout, but it can trigger an attack. There are various rumors about which drinks you should and should not drink; do not take them seriously. However, sometimes patients report that a certain type of alcoholic beverage triggers their attack. In this case, the patient is advised not to drink that type of drink.
SOME QUESTIONS AND ANSWERS ABOUT Gout
Can women get gout?
Mostly men over the age of 40 are at risk for gout, but it can affect women at any age. Very rarely, gout can develop in older women after menopause. In particular, it can occur in women taking diuretics, which may be recommended to treat high blood pressure or heart disease. These drugs cause uric acid to be stored in the body. The development of gout in young women is very rare and requires special investigations.
Does gout cause serious joint disease?
It can only happen in the absence of treatment. Initially, the attacks are acute, the joint returns to its normal state. However, the deposition of uric acid can cause deformity and disability. The good thing is that this can be prevented with appropriate treatment.
Is uric acid stored in places other than joints?
It can be stored under the skin in other areas, for example in the ears and hands. It can also be stored in our internal organs, especially in the kidneys. This is why kidney tests should be checked when evaluating a patient with gout. For this, a urine sample
Can long-term intake of medicines that lower uric acid levels be harmful?
These medicines are quite safe. Sometimes they may need to be stopped because of skin rashes or heartburn. But otherwise they can be taken continuously without any side effects.
Are there other types of crystals other than uric acid that can cause joint disease?
A special type of calcium crystal can also be deposited in the joints like uric acid. It can cause acute attacks similar to gout, but in this case the knee joint is affected rather than the big toe.
Gut sıklığı ülkeden ülkeye değişir mi?
Yüksek ürik asit düzeyine sahip bazı ırklar (örneğin Pasifik ülkeleri) bulunmaktadır; bu kişiler doğal olarak gut hastalığına daha fazla yatkındır. Gut hastalığına yakalanma oranları aynı ülkede bile değişik zamanlarda farklı olabilir. Örneğin İkinci Dünya Savaşı nedeniyle açlığın kol gezdiği ve yaşam koşullarının çok zor olduğu dönemlerde Avrupa ülkelerinde görülümü çok azalmıştır.
*Sayfa içeriği sadece bilgilendirme amaçlıdır. Tanı ve tedavi için mutlaka doktorunuza başvurunuz.
What is chronic fatigue syndrome?

Chronic Fatigue Syndrome is now also known as “Chronic Neuroendocrine Immune Dysfunction”. It is a chronic disease that generally does not go away with rest, lasts longer than 6 months, causes musculoskeletal system and headaches frequently and involves many systems. Chronic Fatigue Syndrome differs from other fatigue-causing diseases in that the exact cause of the disease is not known. Whether Chronic Fatigue Syndrome is caused by medical (organic) or psychiatric causes is still a matter of debate in the medical world. Therefore, the diagnosis of chronic fatigue syndrome requires a medical history, physical examination, assessment of mental state and laboratory findings.
What are the symptoms of chronic fatigue?
- Common symptoms of chronic fatigue syndrome are as follows:
- Constant fatigue and drowsiness, chronic fatigue of unknown cause for more than 6 months, fatigue that does not go away with rest.
- Muscle and joint pains that are not due to an obvious rheumatic disease and that are severe enough to limit one’s daily activities,
- Sore throat
- Abdominal pain
- Energy loss
- Nausea and vomiting
- Hypersensitivity to sound, noise, light, environmental factors,
- Forgetfulness and decline in cognitive performance. Or forgetfulness and accompanying concentration problems
- Disturbances in sleep patterns and quality, inability to “sleep” despite sleeping for 5-8 hours,
- Weakening of the immune system
- Disorders of bowel regularity
- Negative attitudes towards work and social life
- Constant restlessness
- Depression, or feeling dizzy
Therefore, in some medical communities, Chronic Fatigue Syndrome is referred to as “Chronic Neuroendocrine Immune Dysfunction” because it can be accompanied by immunological (similar to allergic), rheumatic (joint, back, back, muscle pain) and neuropsychiatric (sleep disturbance, difficulty concentrating) symptoms.
How is chronic fatigue syndrome diagnosed?
There is no specific test to diagnose chronic fatigue syndrome. The diagnosis is made after excluding other clinical conditions that may cause fatigue. In particular, depression should not be confused with chronic fatigue syndrome. However, patients may develop mental disorders and especially depression over time. However, this does not mean that everyone with depression has chronic fatigue syndrome.
Classically, the following two criteria are required for the diagnosis of chronic fatigue syndrome:
Clinically assessed, unrecognized persistent or recurrent fatigue that begins at a new or known time (e.g. not throughout life), is not the result of ongoing activity, is not relieved mainly by rest, and leads to a marked reduction in current work, educational, social and private life activities, suggests chronic fatigue syndrome.
At the same time, 4 or more of the following symptoms must be present and must persist for 6 consecutive months or more and must not precede the onset of fatigue.
- Significant impairment of short-term memory or concentration
- Sore throat
- Tenderness in the lymph nodes
- Muscle pain
- Pain in various joints without redness or swelling
- New, changing or severe headache
- Inability to wake up in the morning (continued sleepiness)
- Malaise that lasts for more than 24 hours after a job
In addition to these main symptoms, the presence of abdominal pain, alcohol intolerance, bloating, chest pain, chronic cough, diarrhea, dizziness, dry mouth and eyes, ear pain, palpitations, jaw pain, morning stiffness, nausea, night sweats, psychological problems (depression, irritability, anxiety, panic attacks), shortness of breath, skin sensitivity, tingling sensation and weight loss are also expressed.
How is chronic fatigue treated and which groups of doctors are known as Chronic Fatigue Syndrome specialists?
In chronic fatigue, the history (anamnesis) of fatigue complaints given by the patient to the doctor is extremely important. Symptoms accompanying fatigue and comorbidities are equally important for the specialist. In addition, all meaningful information about the patient’s social history, work and daily activities are noted by the physician. According to a study conducted in the USA, since many immunological (autoimmune), rheumatologic, inflammatory, inflammatory and metabolic diseases underlie chronic fatigue, and since a Rheumatologist is both an Internal Medicine specialist and a specialist in Rheumatology, the most qualified physician to treat Chronic Fatigue is a specialist Rheumatologist. Chronic Fatigue syndrome is often confused with Fibromyalgia and Myofascial Pain Syndrome and therefore the best physician to make this distinction was a Rheumatologist. The study suggested that before a patient is diagnosed with “chronic fatigue syndrome” or “chronic fatigue due to Fibromyalgia Syndrome”, the diagnosis should be reviewed and confirmed by a Rheumatologist. The rheumatologist has to consider many factors in order to make the correct diagnosis, and once the correct (definitive) diagnosis has been made, many causes of fatigue can be treated, and this treatment often starts with the elimination of the cause of the inflammation. It is also very important to reduce the foods that cause inflammation. An anti-inflammatory diet prescribed by a Rheumatologist as well as a Dietitian is also very important.
However, there are also cases where there are no underlying Internal Medicine and Rheumatologic causes of fatigue, or there are cases that are resistant to treatment. In these cases, the treatment of chronic fatigue begins with psychiatrists and psychologists. This situation, which adds other branches, emphasizes the importance of multidisciplinary work, not only by a physician, in the treatment of Chronic Fatigue Syndrome. Patients with chronic fatigue syndrome are encouraged to have an active social life. Stress reduction and relaxation techniques can help reduce chronic pain and fatigue. It is also extremely important not to neglect physical health and physical activity. It is also very important that the type of exercises and physical activities are individually designed by a Physical Therapy & Rehabilitation (PT) specialist and continued under the supervision of a doctor. In general, it is recommended to avoid very heavy exercises on days when fatigue is felt. The Physical Therapist adjusts the levels of physical activity and exercise according to the patient’s ability to do so, hence “personalized” programs. Therefore, it is of great benefit to have physical activity, rest and sleep patterns under the supervision of a physician together with a PTR specialist.
In addition, since another new name of Chronic Fatigue Syndrome is known as Chronic Neuroendocrine Immune Dysfunction, some Physical Therapy doctors (and other branches) also apply a complementary treatment method called Neural Therapy. Neuraltherapy is a method that activates the body’s self-healing systems. In Neural Therapy, certain “interference fields” are identified and injected into those areas, and as a result, chronic pain and fatigue can be suppressed.
Although no medication has yet been found to completely cure the disease, a number of drugs have shown a positive response in certain patients. However, medication and complementary treatments for Chronic Fatigue Syndrome are not simple. Morale is very important to cope with this disease. The aim of treatment is always to keep the patient more active and reduce fatigue. Physician supervision is very important and exercise/activity should never be abandoned.
What are the apparent causes of chronic fatigue and how does it differ from chronic fatigue syndrome?
In medicine, there are many medical and psychiatric causes of chronic fatigue. The list below is the most common causes of chronic fatigue (appearing under 15 headings).
Anemia is the most common cause of fatigue. The most common cause in women is anemia due to iron deficiency, but not all anemia is due to iron deficiency.
Vitamin or mineral deficiencies: especially chronic deficiencies of Vitamin D, Vitamin B12, Magnesium, Iron and Zinc can lead to fatigue.
Thyroid disorders: underactive thyroid (hypothyroidism) can cause people to be chronically tired due to thyroid disease. Also subclinical hypothyroidism, Autoimmune Thyroiditis diseases such as Hashimoto’s/Graves should not be forgotten.
Diabetes (uncontrolled Diabetes Mellitus) or insulin resistance
Heart diseases: especially chronic heart failure/cardiomyopathy is one of the most important causes of fatigue. Pericarditis (inflammation of the lining of the heart) can also cause chronic fatigue.
Cancer: patients diagnosed with cancer may experience fatigue for different reasons, and most importantly, it is important to remember that fatigue symptoms may be the earliest sign of some cancers.
Psychiatric Causes: Chronic Anxiety or Depression can be the main cause of chronic fatigue.
Infectious Diseases: Infectious diseases that occur in the body for various reasons are also common causes of fatigue: In particular, Chronic Viral Hepatitis (B and C) can cause fatigue without jaundice, in its chronic active form or in its carrier form. Chronic parasitic diseases, tuberculosis (TB), HIV (AIDS), Epstein Barr Virus (EBV) can also cause chronic fatigue.
Diseases due to Heavy Metal Exposure: Heavy Metal Poisoning can cause insidious diseases and chronic fatigue. Substances such as Lead, Cadmium, Arsenic, Mercury, Aluminum, Fluoride and Copper can accumulate in human tissues and cause DNA damage, leading to health problems such as Cancer, Kidney disease and chronic fatigue.
Metabolic / Other Endocrine diseases: e.g. chronic Renal failure and liver failure, or Hormonal causes / Adrenal dysfunction (related to the hypothalamic-pituitary-adrenal cycle) or Neurally induced hypotension can be the cause of chronic fatigue.
Sleep apnea: Sleep apnea is known to be one of the important causes of chronic fatigue, especially in people who have gained weight and snoring problems.
Immunological causes (related to the immune system): Chronic Rheumatologic diseases, Connective Tissue Diseases, Inflammatory Joint Rheumatism and other Auto-immune or Immunologic diseases are often accompanied by chronic fatigue during active periods of the disease. In addition, chronic intestinal inflammation/inflammatory diseases such as Chronic Intestinal Inflammation / Colitis / Gluten Sensitivity / Inflammatory Bowel Disease / Leaky Gut Syndrome are also among the causes of chronic fatigue.
Deconditioning and physical weakness: Fatigue is also very related to physical strength and fitness. A conditioned and strong person gets tired later.
Malnutrition: It is an important cause of chronic fatigue. Many people follow wrong diets and deprive themselves of important vitamins, minerals, electrolytes and protein.
Work Stress: In the modern age, many people cannot handle the stress of workload, leading to chronic fatigue.
However, the cause of the disease known as Chronic Fatigue Syndrome is not clearly known.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Inflammatory Low Back Pain

Low back pain is a common problem all over the world and can have dozens of causes.
The majority of low back pain is caused by “mechanical” causes such as structural disorders, slipped discs and herniated discs. Most of this type of mechanical pain is triggered by straining the lumbar region, such as lifting something heavy or excessive movement. In general, most mechanical pain is relieved by resting.
Inflammatory low back pain, on the other hand, occurs insidiously, without any strain or trauma. The most prominent feature of inflammatory low back pain is that it worsens with rest and decreases with movement. It is almost the opposite of mechanical low back pain. Inflammatory low back pain is also known as inflammatory low back pain in medical language, but inflammation is not due to infection. The majority of inflammatory low back pain is classified under the group of Spondyloarthropathies, colloquially known as “inflammatory low back rheumatism” diseases. The most severe of these spondyloarthropathies is Ankylosing Spondylitis (AS).
Inflammatory low back pain is definitely a condition to be considered. Especially in patients younger than 40 years of age, if they have morning stiffness (at least 45 minutes) and low back pain for more than 3 months, and if the low back pain worsens with rest and decreases with movement, these symptoms are most likely caused by inflammatory low back pain. Many patients say that simply opening their eyes in the morning is not enough to be ready for the morning. When the patient wakes up in the morning, they have difficulty with personal care and getting dressed. These patients have severe pain or stiffness in the lower back in the second half of the night, especially between 03:00 and 05:00 in the morning. Inflammatory low back pain is characterized by a decrease during the day and in many people disappears completely. It is relieved by movement or exercise and many patients give similar descriptions, such as “it is as if I am a different person during the day, the pain or stiffness disappears completely, but in the morning I wake up stiff again”.
If left unchecked, inflammatory low back pain can later become a progressive disease because it can progress in an insidious way. This is why we try to make an accurate and precise diagnosis as soon as possible. If inflammatory back pain is not treated in time, it can lead to fusion of the spine. Inflammatory low back pain can be accompanied by heel, back, neck, hip or rib pain for years. Patients who are thought to have low back pain for a long time should definitely be reviewed by a rheumatologist if they still have low back pain. A patient who has had “mechanical” pain for years may actually have a Spondyloarthropathy known for inflammatory low back pain. Unfortunately, most of the patients diagnosed with Ankylosing Spondylitis in our country are patients who have been traveling with the diagnosis of “mechanical” herniated disc for years and some of them have undergone back surgery but have not benefited. Therefore, we should pay attention and care about low back pain, especially in young people, and diagnose whether it is inflammatory or not as soon as possible.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is rheumatoid arthritis?

Rheumatoid arthritis (RA) is an inflammatory rheumatism and the most common non-microbial inflammatory joint disease. RA is a chronic, systemic, inflammatory disorder of unknown cause characterized by a symmetrical pattern of joint involvement. The main site of pathology is the synovium of the joints, the lining of the joints, but damage to cartilage, bone, tendons and ligaments/fibers can also occur. The synovial tissues can inflame and proliferate, forming a thick membrane (pannus) that invades the bone, cartilage and ligaments, causing damage and deformities/malformations of the joints. It usually forms a symmetrical pattern, meaning that joints are involved on both sides of the body.
How does rheumatoid arthritis start?
RA usually has an insidious onset with symptoms such as joint pain, swelling, and the number of joints involved over weeks or months. There is a symmetrical distribution within a few weeks or months.
What is meant by symmetrical involvement of joints in RA?
Symmetrical involvement means that both sides of the body are similarly involved, i.e. the right and left side of the body.
What are the typical laboratory findings in blood tests in RA patients?
Rheumatoid Factor (RF) and Anti-cyclic citrullinated peptide (anti-ccp) antibody positivity are important for the diagnosis. Especially anti-ccp is 98% specific for Rheumatoid Arthritis. Patients with active RA have elevated erythrocyte sedimentation rate (ESR) and C-Reactive protein (CRP) values.
Can there be extra-articular symptoms in Rheumatoid Arthritis and what are they?
Yes, there can be, we call these extra-articular symptoms. These include high or chronic fever, swollen lymph nodes, weight loss, weakness, skin lesions, eye inflammation, heart, lung and neurological involvement.
How is rheumatoid arthritis usually treated?
There is no chance of eradicating the disease. The treatments used are aimed at reducing inflammatory rheumatism and joint damage. Long-acting drugs are used to control and dry out the inflammation, such as Methotrexate, salazoprine, Plaquenil and Arava. In addition, injections and infusions (such as Enbrel, Humira or Infliximab/Mabthera), which have been used since 1998, have become important in the last 10 years. It is important to monitor all of these medicines at regular intervals and to carry out the necessary blood tests. Treatment is tailored to the individual patient, taking into account the severity of the disease, concomitant health problems and individual needs, and rest is the most important part of RA treatment. Rest of the affected joints is recommended, especially during acute flare-ups. Apart from the acute period, balanced exercises at times when the patient feels well are beneficial for the patient.
Some simple splints and devices called “splints” can be used to protect the function of the joints and prevent deformities. These splints and splints are very effective in preventing deformities. You can also help prevent deformities by following some rules:
Be careful to use your large joints rather than small joints when doing work. For example, when opening a door, push with your arm rather than your hand, or when opening a jar, open it with your hand rather than your fingers.
Try to distribute the load across more than one joint rather than just one. For example, when lifting a book, hold and lift it with two hands, not one.
Try to use your joints in their most “natural” position. Avoid excessive bending and strain.
Some patients may require surgery to correct deformities, reduce pain or make joints usable.
Close cooperation between the physician and the patient is needed at all stages of treatment decisions.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Fibromyalgia?
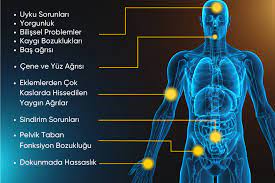
Fibromyalgia is a chronic musculoskeletal disease of unknown cause, characterized by widespread pain and tender points in certain parts of the body. It is a chronic disease that does not cause limitation of movement and deformity in the joints but impairs the quality of life of the person.
What are the conditions that cause fibromyalgia?
Although the cause of the disease is unknown, many conditions such as stress, anxiety, depression, perfectionist personality, neurohormonal disorders, immune system disorders, muscle problems, flu-like viral infections, noise, physical injuries, physical and psychological trauma (such as car accident, childhood sexual abuse, divorce, death of a loved one), heavy work pace, humid environment, sleep disorders, prolonged computer use are thought to cause fibromyalgia in those with genetic predisposition.
What is the prevalence of fibromyalgia and who suffers from it?
It affects approximately 2% of the population. Although it can be seen at any age and in both sexes, it is most common between the ages of 25-55 and more common in women than men. This disease is also seen in children and the elderly.
What are the symptoms of fibromyalgia?
The signs and symptoms that make up the clinical picture in fibromyalgia syndrome are very diverse. The main signs and symptoms are chronic widespread pain, stiffness, fatigue, sensitive and painful points and sleep disturbance.
Widespread Pain and Stiffness: Chronic, widespread and bilateral. It is often localized in the lower back, neck, shoulders and hips. It is burning, gnawing and radiating and rarely disappears completely. It varies throughout the day. Increases with cold, stress, fatigue, humid air, insomnia, anxiety, car travel, family problems, environmental and workplace conditions, and physical and emotional trauma; decreases with hot baths, warm and dry air, vacation, restful sleep and exercise.
Fatigue: The patient gets out of bed tired in the morning. Fatigue lasts all day, is severe and even light activity increases fatigue. Patients describe fatigue and weakness in performing daily tasks.
Sleep Disorders: Patients often complain of insomnia, light sleep and lack of rest during sleep.
Headache: Tension and migraine headaches are very common.
Subjective feeling of swelling: It cannot be seen on examination but the patient expresses that the joints are swollen.
Raynaud’s Phenomenon: Patients have bruising and blanching of the hands in the cold.
Irritable Bowel Syndrome: Patients may have constipation or diarrhea with abdominal pain, bloating and excess gas.
Irritable Bladder Syndrome: Although there is no urinary infection in patients, complaints such as frequent urination, burning during urination and pain in the lower abdomen are common.
Dry Mouth: It is not related to the use of any medication.
Anxiety and Depression: Anxiety has been reported in 50-70% and depression in 30%.
What are the physical examination findings?
- Painful points As defined by the American College of Rheumatology (ACR), applying a pressure of 4 kg with a finger causes pain in 11 of 18 specific points in various parts of the body.
- Other examination findings
- Dermographism: A form of urticaria (hives) that occurs when the skin is scratched or rubbed with a hard object, or where clothes and underwear squeeze the body.
- Cutis anserina: A skin condition characterized by the erection of feathers due to cold or fright; goose skin.
- Cutis marmaratus: Red-purple streaks on the skin caused by circulatory disturbances due to infection or sudden changes in temperature.
- Excessive sweating
- Hypersensitivity over the upper scapula
How is fibromyalgia diagnosed?
Laboratory tests and radiological examinations in fibromyalgia are not performed for diagnosis but to exclude other diseases that may be confused with fibromyalgia. Laboratory tests give normal results in fibromyalgia. If there are no signs of inflammatory rheumatic diseases or neck and lumbar herniated discs, there is no need for radiologic examination. Fibromyalgia is diagnosed by anamnesis and clinical examination. Fibromyalgia is diagnosed with widespread pain in the right and left half of the body, upper and lower back for more than 3 months, as well as pain in the spinal axis and the detection of 11 painful points on examination.
What are the conditions that can be confused with fibromyalgia?
Inflammatory rheumatic diseases, hypothyroidism, neuropathic pain, chronic fatigue syndrome, myofascial pain syndrome and some neurological diseases and cholesterol-lowering drugs (Statins)
What are the goals of fibromyalgia treatment?
Today, there is no treatment that provides a complete cure for fibromyalgia. Treatment aims to reduce complaints, maintain and improve quality of life and functioning.What are the treatment approaches in fibromyalgia? Treatment of this disease can be done with 4 main approaches. Drug therapy. physical therapy, psychosocial approach and complementary therapies
Psychosocial approach
As with any disease, informing and educating the patient about the disease is very important in treatment. The aim of education is to improve the patient’s self-management and self-efficacy, to gain the ability to cope with complaints, and to change negative perceptions such as feelings of frustration and helplessness in a positive direction. In addition, the patient’s compliance with the treatment should be increased through education. The patient should be told that his/her disease is “real” but not a disfiguring or disabling disease. Then, harmful habits such as alcohol and smoking should be reduced, as they both increase pain and weaken the muscles. Excessive caffeine intake disrupts sleep quality and increases the patient’s complaints. Some behavioral changes should be taught to the patient in the treatment. Patients should be told to avoid stress and excessive excitement and their tension should be reduced. The patient’s perfectionist personality and meticulousness in daily life activities should be shown to him and he should be told that he should take a break while doing physical activity, housework and hobbies. . However, the patient’s work should not involve prolonged sitting or standing and the patient’s workplace and working conditions should be organized.
Drug treatment
In the treatment of fibromyalgia, painkillers, antidepressants, anti-epileptics, muscle relaxants and sleep regulators are used according to the patient’s condition and the patient.
Physical therapy
Physical therapy sessions and exercise programs, which occupy the most important place in the treatment, are applied. In physical therapy, hot application, currents to reduce pain such as TENS or interference, ultrasound, laser, hiltherapy, cupping, massage, taping, dry needling, trigger point injections, mobilization and manipulation applications can be performed. With spa treatment, a decrease in pain threshold and the number of painful points and an increase in quality of life are provided.
Exercises
The main goals of exercise are to reduce stress, maintain and increase muscle strength and endurance, and ensure proper posture. It is known that patients with fibromyalgia have decreased muscle strength and muscle condition. Low muscle condition also increases the risk of muscles being affected by microtraumas and causes pain and fatigue. In general, cardiovascular (aerobic), strengthening, stretching, relaxation and aquatic exercises have been found to be beneficial in fibromyalgia. Studies have shown that cardiovascular (aerobic) and strengthening exercises improve physical functions, quality of life and pain. Since the pain and fatigue of these patients increase when they start exercising, light activities such as walking, swimming and cycling can be done first. Over time, the exercise program can be gradually increased as their fitness and muscle strength increase. The type and intensity of exercise should be adjusted according to the patient. These exercises should be performed 3-4 times a week for 20-30 minutes.Posture exercises for the evaluation of posture and correction of poor posture are important in these patients. Patients should be recommended to sleep on an orthopedic bed and use orthopedic pillows.
Complementary therapies
NutritionIn fibromyalgia, a special nutritional application is not recommended, except for healthy nutrition and nutritional recommendations that support achieving the target weight.Ozone therapy, Acupuncture, hypnosis, clinical pilates and meditation techniques (TAI chi, Yoga, Qi gong) can be applied as part of the treatment in fibromyalgia patients, in accordance with the clinical condition and conditions of the patient.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is a heel spur?

Heel spur is an important health problem that causes pain in the sole of the foot and negatively affects the quality of life. It usually manifests itself with a stinging sensation in the sole of the foot after prolonged immobility. The pain is most severe in the first few steps after getting out of bed in the morning. Pain can also be triggered by prolonged standing or standing up after sitting.
A heel spur is a bony protrusion caused by calcium deposits at the bottom of the heel bone. This protrusion can be easily diagnosed on X-rays. Sometimes there may be heel spurs that are too small to be seen on X-rays. This condition is called “heel spur syndrome”. Heel spurs are usually caused by inflammation of the thick band of tissue called the plantar fascia, which runs along the bottom of the foot and connects the heel bone to the toes. Under normal conditions, this band acts like a shock-absorbing arch and supports the foot. If the tension and stress on this band increases, inflammation develops over time. A heel spur that develops on the back of the heel is often associated with inflammation of the Achilles tendon. Heel spurs do not always cause pain. Also, not all heel pain is caused by heel spurs.
What causes heel spurs?
Heel spurs are caused by calcium buildup in the lower part of the heel bone over months. The inflammatory process caused by chronic stretching and tearing of the sole band called plantar fascia is the most important cause of calcium deposition.
Some factors increase the risk of heel spurs:
Certain types of exercise, long-distance running and jumping sports, activities that put a lot of stress on the heel and connective tissue, such as ballet and aerobic dance, and occupations that require constant standing
- Being overweight
- Wearing unhealthy shoes that are not suitable for foot structure
- Gait disorders that put stress on the bones and ligaments of the foot
- Foot deformities such as flat feet, foot arch height, outward or inward tread, and dropping of the metatarsal bones
- Inflammatory diseases such as reactive arthritis and ankylosing spondylitis
- Achilles tendonitis
What are the symptoms of heel spurs?
The most obvious symptom of a heel spur is pain in the sole of the foot during the first step in the morning. The pain decreases with a little walking and may even go away. However, the pain starts again later in the day with standing. Waking up in the morning with unrested feet and waking up with pain in the heel are among the symptoms of heel spurs. A heel spur is suspected if pain accumulates in the heel after a long period of sitting and resting, and if pain is felt when stepping on it. Heel spur is a condition that leads to a decrease in quality of life. It reduces the person’s mobility. The patient cannot walk comfortably due to heel pain.
Heel spurs should not be confused with daily foot pain. It is quite normal to have pain in the heel if the foot is overtired. However, even in cases where the foot is not overloaded, if there is pain in the heel for no reason, the heel spur problem can be suspected. In heel spurs, the pain starts directly from the heel and does not spread from another area to the foot. Heel spur pains are completely localized and occur with a stinging sensation. Heel spurs also cause gait disturbances over time. These bring along problems such as wobbling and walking inward.
How to recognize a heel spur?
The diagnosis can usually be made by clinical examination in a patient who describes severe and nail-piercing pain in the first steps of the day. The presence of a heel spur is confirmed by seeing the protrusion on the heel bone on an X-ray. In some cases, severe pain may be present even though the bone spur is not yet visible. This is called heel spur syndrome. In addition, heel spurs can be found in X-rays taken for another reason without any symptoms.
How is heel spur treated?
In the treatment of heel spurs, pain and complaints can be reduced by making some changes in daily life.
The aim is to reduce the pressure on the foot, control pain and inflammation, stimulate tissue healing and increase the flexibility of soft tissues. Measures such as rest, wearing soft-soled shoes or slippers, losing weight and using a heel cushion are the first methods to be used.
If the patient has compression defects such as flat feet, appropriate insoles and shoe adjustments should be made. Stretching exercises and ice application for the soles of the feet, as well as simple edema and pain relieving medications may also be useful in treatment.
In cases where these measures are not sufficient, physical therapy methods are used.
ESWT, or shock wave therapy, is a reliable treatment method based on the application of high-pressure sound waves to the desired area of the body with an application head. It is applied in a total of 3 to 5 sessions. The application time is between 10-20 minutes. After the application, the patient can continue his/her daily life. Within 4-6 weeks after the treatment, pain and complaints are largely eliminated and the patient’s quality of life is improved.
Hilterapy (high intensity laser therapy) is another treatment method used in the treatment of heel spurs. It is applied between 3 to 5 sessions. It is a completely painless and painless treatment method.
Local cortisone and platelet-rich plasma injections are other methods that can be used in treatment. Surgery is the last option in the treatment of heel spurs and is rarely used. The vast majority of patients regain their health with non-surgical treatments.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Contact
- Karanfil avenue . Alkaranfil street No: 4 Ofis No: 1 Beşiktaş / İstanbul
- +90 850 220 17 21
- info@checkupway.com

