1) Eye Diseases

Lazer
Eye Checkup
Detect your vision problems early and take the necessary precautions with checkup programs prepared by specialist doctors to detect your visual defects.
It is recommended that healthy people undergo eye checkup programs once a year.
Retina Checkup
The retina is a network of visual cells that covers the back wall of the eyeball like wallpaper. At the same time, the retina consists of 10 layers, the retina is the most complex and sensitive part of the eye. The retina allows light to be transmitted to our brain as an image and this is how we see. Problems occurring in the retina are not an eye disorder, but an eye disease. Early diagnosis is very important at this point.
Refractive Checkup
It is recommended to have a refractive checkup once a year to detect vision problems such as myopia, hyperopia, astigmatism, presbyopia and keratoconus and to obtain the basic data necessary for the application of treatments to improve your vision quality. In order for the refractive checkup results to be healthy, you should stop wearing contact lenses at least 5 days before your checkup appointment,
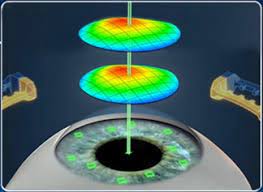
Laser
General information
In which diseases is laser eye reshaping applied?
It is applied in the treatment of refractive errors such as myopia, astigmatism and hyperopia.
How Long Does Laser Eye Lining Surgery Take?
The laser treatment takes about 4-5 minutes for each eye and no pain is felt. It is very important that the patient is comfortable throughout the treatment and follows the doctor’s instructions. After the treatment is over, the patient is taken out of the laser room without bandaging the eyes.
Types of Laser Eye Reshaping Surgery Types of Laser Eye Reshaping Surgery
There are 13 different methods and state-of-the-art technology in laser treatment, popularly known as eye reshading. The eye examination for laser treatment takes about 1 and a half hours and requires an examination including detailed examinations.
Does the eye disorder go away after laser surgery?
The degree of eye impairment after laser surgery is to bring it to + / – 0.50. In laser, it is aimed to see as much as you can see with glasses without glasses. Numbers of 0.5 and below are glasses-free values and are perceived as successful. If the laser is performed while the numbers are still progressing, you may have to wear glasses again. Therefore, the numbers should not increase for at least 1 year. After the laser, 95% of myopes and 70% of hypermetropes remain glasses-free.
Up to How Many Numbers Is Eye Lining Performed?
People with myopia up to -10 diopters People with astigmatism up to 6 diopters People with astigmatism up to 6 diopters People who feel the need for glasses and do not want to wear glasses, laser can be applied to any number if the eye structure is suitable.
What is the age for laser eye correction?
Laser operation can be performed after the age of 18.
Who Can Receive Laser Treatment?
People over 18 years of age
People with suitable corneal thickness
People with myopia up to -10 diopters
People with astigmatism up to 6 diopters
People with hyperopia up to +4 diopters
Those who do not have systematic diseases such as diabetes and rheumatism
Those who do not have any other diseases in their eyes (corneal sharpening, eye pressure, etc.)
Not pregnant or breastfeeding
The conditions for eye scratching are as stated above. Contrary to popular belief, the laser method is not new, but a form of treatment that has been successfully applied since 1990. Laser treatment, which is popularly known as laser eye correction, is applied for the treatment of refractive errors such as myopia, hyperopia and astigmatism.
Caution: If the patients who will undergo laser examination use contact lenses, they should stop using contact lenses at least 5 days before and should not use them until the examination.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Laser Treatment Processes
How is a Laser Examination Performed?
A detailed eye examination should be performed to determine the laser eye surgery to be applied in laser treatment. In the examination, visual acuity and spectacle numbers should be determined, corneal topography should be taken, biomicroscopic examination should be performed and finally eye pressure should be measured.
Systemic conditions such as age, diabetes, goiter and high blood pressure should be questioned in detail and Wavefront or Topolaser further examinations should be performed according to the need.
Which examinations are necessary for laser treatment?
For laser treatment, a detailed topographic analysis of the cornea layer of the eye is performed with the topography device and the thickness of the cornea is calculated. Corneal thickness is as important a parameter as eye number.
How is a Drop Eye Examination Performed?
After a drop that dilates the pupils is instilled and left for about 30 minutes, the eye numbers are determined again and a detailed fundus examination (retinal vascular and nerve layers) is performed. If there are objects and areas such as thinning, tears, holes in the retina, these enlargements are primarily treated with the argon laser method. Argon laser application may require postponing the laser eye surgery for 3 weeks. However, this procedure is absolutely necessary before laser eye surgery is performed. After the pre-treatment, laser eye surgery will be safer and the process will be more comfortable.
What Should Be Considered Before Laser Treatment?
There is no harm for people who will have laser treatment to eat on the day of laser eye surgery.
The patient only before laser eye surgery;
She should not wear eye makeup,
She should not wear perfume,
Blood thinners should not be taken.
What Procedures Are Performed During Laser Treatment?
For laser eye surgery, a sterile cover is first placed over the patient’s eye, then the eyelids are opened with a specially produced apparatus to prevent the eyes from closing during the treatment. Laser eye surgery takes about 4-5 minutes for each eye, and thanks to the anesthetic creams applied, the patient does not feel any pain during laser eye surgery. It is very important that the patient is comfortable and follows the instructions during laser eye surgery. The eyes are not bandaged after laser eye surgery, but special glasses may be given to prevent eye sensitivity after laser eye surgery.
What Should Be Considered After Laser Treatment?
After the laser treatment is completed, the patient is kept waiting for about half an hour and taken for a control examination. The patient is discharged after this control. On the first day, it is normal to have blurred vision or stinging, burning and watering in the eyes for 3 to 4 hours. It is very important to apply the medication as recommended by the ophthalmologist. If you feel a headache after laser eye surgery, you can take a painkiller without blood thinners. On the day of laser eye surgery, it is not recommended to drive or return to work on the same day after laser treatment. Dusty environments should be avoided after laser eye surgery, and it is not recommended to rub, itch, touch or wash the treated eyes for the first 24 hours. Contact with the eyes should be avoided when using soap and shampoo on the first day after laser eye surgery.
It is necessary to use an artificial tear drop recommended by the ophthalmologist for about 3 – 6 months after laser eye surgery.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
SMILE LASER / RELEX

Which Patients Can Receive Smile Laser Treatment?
Smile laser treatment is one of the personalized superficial laser treatments that we usually apply in eyes with thin corneas and not very high myopia and astigmatism. After a detailed examination, Smile Laser treatment can be applied to people whose eye structure is deemed suitable for surgery by the doctor.
It is a suitable treatment method for athletes and professional groups who are at risk of being exposed to impact and pressure.
Who is Relex Smile Laser Not Applicable?
As a result of detailed examinations and examinations, people whose eye structure is found suitable for surgery by the doctor can be treated with laser. In the treatment of myopia and astigmatism, it is a laser technology method that provides the opportunity to treat up to -10 in myopia and up to -5 in astigmatism with the personalized bladeless SMILE laser method.
How is Relex Smile Laser Treatment Application?
With Zeiss Visumax Femtosecond technology, a thin lenticule (disc-shaped tissue) is created in the anterior layer of the eye (cornea) in a single step. The surgeon removes the created lenticule from the cornea through a 2.0 mm opening in the cornea. There is no need to cut any flap. The refractive error in the eye is corrected by changing the shape of the cornea as a result of the removal of the lenticule. Since no flap is created, corneal biomechanics are less affected.
What is the Difference of Smile Laser?
SMILE (Small Incision Lenticule Extraction) and No-Touch Laser technologies have attracted attention as treatment methods for myopia and astigmatism in recent years. With these technologies, successful results are obtained in myopia and astigmatism problems and less dry eye problems occur after laser.
Why Smile Laser?
Treatment up to -10 in myopia and -5 in astigmatism
Preservation of corneal biomechanics
Compatibility with thin cornea structure
Incisionless operation with closed surgery technique
One-stage surgery
Safe recovery
ATHLETES HAVE AN ADVANTAGE WITH SMILE LASER
The SMILE method provides a significant advantage over other methods in maintaining the mechanical strength of the patient’s cornea. This method is especially advantageous for athletes and people with busy work and education lives. An important advantage for people who do sports is that the person can return to his/her sport in a very short time after the treatment.
This treatment is a personalized non-contact laser using iris identification technology. With iris recognition, the rotations of the eye on its axis can be calculated and this method allows us to treat astigmatism in the most accurate axis.
WHAT WILL CHANGE IN YOUR LIFE WITH SMILE LASER?
You can easily see your watch and your face in the mirror.
You can get a natural look and vision without glasses and lenses.
You can achieve comfort and higher success in your sports activities.
You will be less affected by climatic events such as wind and rain.
You can improve your quality of life by getting rid of the restrictions you experience in your daily activities because you cannot see clearly.
Frequently Asked Questions
What is the Corneal Thickness for Smile Laser?
The cornea should be at least 500 microns thick. In some special cases, Smile method can also be considered in 490 micron thickness.
What is the Smile Laser Healing Process?
It takes approximately 10-15 minutes. Recovery after Smile laser takes place quickly. The next day after the operation, the patient can return to work life and start sports such as walking and jogging. Water sports can be started in 1 week, impact sports such as karate and kick boxing can be started in 1-2 weeks.
Is Smile Laser Applied to Hyperopia?
This method can be applied in the treatment of myopia and astigmatism refractive errors. Other alternative methods recommended by the doctor for the treatment of hyperopia are recommended as a result of the tests performed.
How Long Does Blurred Vision Last After Smile Laser?
Blurred vision after the operation may last for about 2-3 hours. It is very important to use the drops recommended by the doctor regularly after the treatment in order to have a healthy healing process.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
iLASIK (iDesign Wavefront)
What is i-Lasik Laser?
On average, 80% of people worldwide have refractive error.
Refractive surgery has been practiced since 1980 and the method that gives the most reliable results in the treatment of refractive errors is the laser method. With the developing technology, refractive errors such as myopia (difficulty in distance vision), hyperopia (difficulty in near vision), astigmatism (blurring of the image) can be treated with laser.
The aim of laser treatment is to increase the quality of life of people and to ensure that they have a more comfortable life. Today, I-LASIK (Laser Assisted insitu Keratomilluesis) is the most widely used treatment method for the treatment of refractive errors all over the world. This method is personalized and is performed in accordance with the patient’s eye structure after detailed examination and diagnosis.
Who Can Receive i-Lasik Laser?
People over 18 years of age
Myopia up to 10, hyperopia up to 6 and astigmatism up to 4 degrees
Those with a sufficiently thick cornea
Those who do not have systematic diseases such as diabetes and rheumatism
As a result of the preliminary examination and examinations, i-Lasik laser treatment can be applied to people whose eye structure is deemed suitable for surgery by the physician.
How is i-Lasik Surgery Performed?
In i-Lasik application, the entire procedure is planned specifically for the patient with wavefront and idesign technology and even the smallest defects can be corrected with the combination of the eye recognition system. With the use of femtosecond laser, bladeless incisions are possible and this increases the success of the treatment.
Wavefront
The program is determined by evaluating the image obtained in the retina layer by sending a beam of light to the eye. It is a preferred method especially for patients with night vision problems or large pupils to avoid scattering, scattering and shadowing around the light after laser. The operation decision is made after evaluation with special Wavefront analyzers.
iDesign Wavefront
In the first stage, a personal vision profile is prepared with Wavescan technology.
Then a femtosecond corneal incision is made without the use of a blade. Vision can now be corrected within the framework of iLASIK.
The information reflected from the light sent to the eye is detected by a special camera. This information is sent to the laser and the planned treatment is applied. One of the reasons why Advanced CustomVue™ is preferred is the ability to map three-dimensional vision with Wavefront aberometry.
In laser treatment, it is very important that the device shoots at the planned point of the eye.
Therefore, there must be a digital locking system (eye tracker) between the device and the eye. In Wavefront treatment, measurements are made while sitting and the operation is performed in a lying position. In this position, a small rotational movement may occur in the eye. The iris layer of the person is detected by the laser device and can follow the movements of the eye around its axis.
Differences between i-Lasik and Lasik
The difference of i-Lasik operations from other operations is that personalized laser treatment can be performed. In i-Lasik surgery, the entire procedure is planned specifically for the patient’s eye structure with wavefront and iDesing, and even the smallest defects can be corrected with the combination of the eye recognition system. In LASIK operation, the corneal flap is opened with a knife called microkeratome.
Does Blurred Vision Occur After i-Lasik Laser Surgery?
In all laser operations, blurred vision may occur on the first day. This condition is temporary. The patient may experience blurred vision for the first few days after the operation.
What is the i-Lasik Laser Recovery Period?
After the i-Lasik operation, the patient is called for control the next day and then can continue his/her daily life. Full recovery takes place within 10-15 days.
How Long Does i-Lasik Laser Surgery Take?
The i-Lasik operation takes approximately 10 minutes. In the first stage, a flap is created using femtosecond technology. In the second stage, number correction is performed with excimer laser. With these stages, the operation takes approximately 10 minutes.
Is i-Lasik Laser Treatment Permanent?
In all laser treatments, it is possible, although very unlikely, for the numbers to come back.
How Should We Protect Our Eyes After i-Lasil Laser?
It is recommended to wear protective glasses or sunglasses to protect and rest the eyes after the operation. The eyes should not come into contact with water on the first day and should not be rubbed in any way. The patient should regularly use the drops given after the operation and should not neglect the control the next day.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Femtosecond Laser (Intralase)

What is Femtosecond Laser?
Femtosecond Laser is a laser technology used in the treatment of refractive surgery and cataract surgery. Femtosecond affects the success of computer-controlled laser surgery and plays an important role in the operation.
With Blade Laser;
Unplanned surgical outcomes, flap tears
High risk in people with thin cornea
Inability to apply the treatment to people with high eye number
Higher risk of dry eye formation
With bladeless Femtosecond Laser;
Possibility to create flaps in the planned thickness for those with thin cornea structure
Possibility of laser in people with high eye number
Lower risk of post-operative dry eye
Who Can Receive Femtosecond Laser?
It can be performed if the eye structure is suitable for the treatment of refractive errors. The method can be determined after a detailed eye examination.
Is Femtosecond Laser Applied for Myopia?
Femtosecond Laser; It is a method applied in the treatment of refractive errors such as myopia, hyperopia and astigmatism.
Which Eye Diseases is Femtosecond Laser for?
The method is used in all refractive errors, i.e. refractive surgery and cataract surgery.
How is Femtosecond Laser Surgery Performed?
During the laser operation, it is necessary to open a flap with a thin incision in the cornea; Femtosecond Laser opens this process at the desired level without using a knife (flap) and allows it to be created with laser beams.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
PRK / LASEK

What is PRK?
PRK (Photorefractive Keratectomy) is a laser method used in the treatment of patients with refractive errors such as myopia, hyperopia and astigmatism.
Who Can Receive PRK / LASEK Laser?
People who are over 18 years of age and whose eye structure is determined to be suitable as a result of a detailed examination can be applied PRK LASEK method. The procedure can be performed after the examination or on the day recommended by the doctor.
Who is PRK / LASEK Laser Applied to?
People over 18 years of age
People whose corneal thickness is suitable for Lasek method
People without systematic disease
People without diseases such as corneal sharpening, eye pressure, etc.
People who are not pregnant or breastfeeding
What is LASEK?
Lasek is based on the principle of removing the epithelial tissue in the eye with the help of alcohol. After the laser is applied, the epithelium spreads back to its place. Although safe results are obtained with these two surface methods, patients may experience burning, stinging and watering for 2-3 days. Vision becomes clear in an average of 1 week-10 days.
How long does it take to recover after PRK / LASEK laser?
After the laser surgery is completed, the patient is kept for approximately half an hour and then a control examination is performed. It is very important to use post-operative medication as recommended by the doctor to accelerate the healing process.
In case of a headache after the operation, painkillers without blood thinners may be preferred. Again, be sure to consult your doctor about this situation.
We recommend not driving after the operation and resting that day. Also, avoid being in a dusty environment, do not rub, itch, touch, wash your face or take a bath for the first 24 hours. The day after the operation, there are no side effects that will restrict social and work life.
If a wrinkle is detected in the transparent area on the surface of the eye or if there is a reaction under the flap, it may be necessary to wash under the flap.
After the surgery, an artificial tear drop recommended by the doctor should be used for about 3 – 6 months.
What should be considered before PRK Laser Treatment?
There is no harm in the patient eating before the treatment.
The patient should only
Should not wear eye makeup,
She should not wear perfume,
They should not drink blood thinners.
Patients who wear contact lenses are advised to stop using their lenses 1 week if they wear soft lenses and 2 weeks if they wear hard lenses before PRK examination and surgery.
Advantages of PRK laser surgery;
No scarring occurs because a corneal flap (membrane) is not removed.
Patients who do not want to be scarred often prefer it.
Since the corneal flap (membrane) is not removed, there is no deterioration in the natural structure of the cornea.
Patients who undergo PRK laser surgery do not feel pain or ache and eye pressure does not increase since vacuum is not used during the operation.
How long does blurred vision last after PRK / LASEK surgery?
On the first day; blurred vision and stinging, burning and watering in the eyes for 3 to 4 hours is normal.
Is PRK / LASEK Laser Safe?
The PRK Lasek method, which is widely used for the treatment of refractive errors such as myopia, hyperopia and astigmatism, has been successfully applied all over the world since 1987.
Up to How Many Numbers Is PRK / LASEK Laser Performed?
While the general rule is accepted as 6 – 8, the suitability of the patient’s eye structure should be evaluated for the operation.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Phakic Lens Treatment

What is a Phakic Lens?
Phakic intraocular lens is one of the strongest alternatives in the treatment of refraction and is a treatment method applied in all refractions “hyperopia, hyperopia astigmatism, myopia and myopic astigmatism” eye refraction defects.
Advantages of Phakic Intraocular Lens Surgery
The biggest advantage of phakic intraocular lens surgery is that the application is reversible and can be applied to people with high myopia and hyperopia. Phakic lens surgery at Dünyagöz Hospital is performed by the relevant branch physicians based on the principle of placing an artificial and numbered lens inside the eye.
For Which Eye Diseases is Phakic Intraocular Lens Suitable?
- Myopes from 0.5 diopters to 20 diopters,
- Myopic astigmats from 0.5 diopters to 6 diopters,
- Hyperopia from 5 diopters to 10 diopters,
- Hypermetropic astigmatism from 5 diopters to 6 diopters can be treated.
To whom is phakic lens surgery performed?
Phakic lens surgery can be performed on people over the age of 18 who have not had a major change in their refractive error in the last two years and who do not have glaucoma (eye pressure), retinal diseases and cataracts. The final decision on whether this treatment is suitable for the person’s eye structure can be determined after a detailed eye examination and examination of the corneal tissue with special tests.
How is phakic lens treatment performed?
Phakic lens surgery takes about 5 minutes for one eye and the patient does not feel anything because it is under general anesthesia. No bandage is required.
Is Phakic Intraocular Lens Treatment Permanent?
The lens placed inside the eye is transparent and compatible with the eye tissue. When all processes are performed ideally, the lens is produced from a medical material that will remain in the eye for a lifetime without causing any problems.
These lenses placed in the eye cannot be seen from the outside after surgery and the presence of the lens in the eye is not felt by the patient. With phakic lens treatment, this lens placed in the eye can be removed at the patient’s request and provides the opportunity to benefit from different treatment methods suitable for the patient.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Intraocular Lens (IOL) Treatment
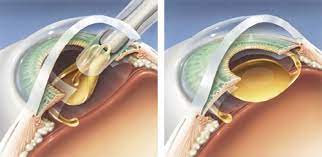
What is Intraocular Lens Therapy?
Intraocular lens treatment is a method used for the treatment of cataracts and refractive errors in the eye.
This method is applied by replacing the natural lens in the eye with lenses produced with special technology.
Advantages of Intraocular Lens Surgery
Intraocular lens surgery can be applied for the treatment of refractive errors such as myopia, hyperopia and astigmatism. In the method applied, the lens inside the eye is removed and replaced with a lens with more than one focal ability, while the treatment of refractive errors is provided, if there is a cataract problem in the eye, cataract treatment can be provided.
How is Intraocular Lens Treatment Performed?
This method is called Clear (transparent) lens replacement. Intraocular lens treatment is performed by opening a 3mm incision and placing the lens into the eye. The implanted lens takes its normal shape with body heat.
Steps of Lens Placement Inside the Eye
For intraocular lens application, the patient must first undergo a comprehensive examination and a series of examinations. After the patient’s eye structure is evaluated by the doctor, the type of lenses to be implanted is determined. Since the treatment is also a cataract method, both the cataract of the patient is treated in a single session and the distance and near vision problems are eliminated in suitable candidates with the lens to be placed in the eye.
There are various rings in the lenses. Some of these rings provide distance vision and some provide near vision. The doctor determines the type of lens according to the patient’s eye problem.
Who Can Receive Intraocular Lens Treatment?
Patient selection is very important for this treatment. Attention should be paid to whether it is more important for the patient to see far or near. Another important issue in patient selection is the pupil size of the patient. The patient must first undergo a detailed eye examination. Not every patient’s eyes may be suitable for this type of surgery.
The occupation, age, social activity, reading habits and intellectual level of the patient with cataract are also important in patient selection. Successful treatment is possible with appropriate patient selection, appropriate technique, the experience of the institution where the surgery is performed and the physician and of course the right lens.
What Should Be Considered After Intraocular Lens Treatment?
Postoperative vision will reach its normal level within 1-2 days. Antibiotic, cortisone eye drops and tear drops recommended by your ophthalmologist should be used for the recommended period.
After intraocular lens treatment, the patient is discharged on the same day.
Routine controls are on the 1st day, 1st week, 1st month and 6th month after surgery, but the frequency and duration of controls may vary by the ophthalmologist.
What is Trifocal Lens?
In the Trifocal Lens method, the lens inside the eye is removed and replaced with a lens with more than one focus capability. These lenses have various rings. Some of these rings provide distance vision and some provide near vision. Thus, both distant and near images fall on the yellow spot in the eye that provides vision. Patients who are suitable for treatment can adapt to this and their dependence on distance and near glasses may decrease.
Trifocal Lens Advantages
Trifocal lens treatment provides clarification of vision at the level seen with glasses at far, near and middle distances. At the same time, thanks to the fact that the treatment to be performed with lens replacement based on the principle of cataract operation, cataract treatment will be provided for people with cataract problems before treatment, and cataract formation will not be seen in people without cataract problems in the future.
Patient selection is very important for this treatment. It should be noted whether it is more important for the patient to see far or near. Another important issue in patient selection is the pupil size of the patient. Since the treatment is a cataract surgery, patients can find a solution to both cataract problems and distance and near vision problems in the same session.
The patient must first undergo a detailed eye examination. Not every patient’s eye may be suitable for this type of surgery. The professional position, age, social activity, reading habits and intellectual level of patients with cataracts are also important in patient selection.
Frequently Asked Questions
Is Intraocular Contact Lens Application Permanent?
Lenses placed in the eye can be used for a lifetime.
Can Intraocular Lens Be Removed?
Intraocular lens operations are performed by removing the lenses that exist in the eye and have lost their refraction and transparency and replacing them with new lenses compatible with the patient’s eye.
It should not be confused with contact lenses used daily and monthly.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
About Cataract

What is Cataract in the Eye?
Cataract in the eye is an eye disease that causes the lens of the eye behind the pupil to lose its transparency over time, causing blurred vision, often seen in middle age and older.
Cataract Onset:
Just behind the pupil is our natural lens, which gives our eyes a refractive power of 10 at a distance and 13 at near. With advancing age, our natural lens loses its transparency and becomes opaque. Initially, cataracts do not completely affect vision. This is because it does not initially cover the entire lens of the eye. The onset of cataracts is in the form of dulling of colors and decreases in the quality of vision.
How does the eye with cataracts see?
An eye with cataracts begins to see as if looking through a fogged glass. As the cataract progresses, it significantly reduces vision and negatively affects the patient’s life. Cataract is a disease that can be diagnosed with a simple eye examination. However, a detailed eye examination should be performed to determine whether the patient has other eye diseases accompanying cataracts. In the examination to be performed; the transparency of the cornea, the structure of the cataract, the position of the lens, the width of the pupil, the condition of the retina are examined in detail before the operation plan and the patient’s cataract treatment is evaluated in terms of operation.
What are the Symptoms of Cataract?
- The most prominent symptoms of cataract are,
- Decreased visual acuity,
- Impaired night vision,
- Blurred vision in sunny weather,
- Sensitivity to light,
- Frequent changes in spectacle numbers,
- We can list complaints such as blurred colors.
Is it possible to prevent cataract?
It is not possible to completely prevent cataract disease. However, measures can be taken against the risk of cataract formation:
- Protection from sunlight, wearing sunglasses,
- Proper and balanced nutrition,
- Avoid smoking and alcohol consumption,
- People with diabetes (diabetes) to keep their disease under control.
At what age is cataract seen?
Cataract manifests itself with a slight dulling and hardening of the lens of the eye in people aged 50-60 years on average. However, it can be observed at earlier ages, even in infancy. Cataracts can also be seen in diabetics, patients who are exposed to eye impact or patients who use cortisone for a long time.
How does a cataract go away?
It is not possible to remove cataracts with medication or glasses. The only treatment for cataract is surgery. As the cataract progresses, it begins to disturb the patient’s life by significantly reducing vision. The technology used for cataract surgery and the quality of the lens placed in the eye determine the success of the surgery and most importantly the quality of the patient’s vision.
How Long Does Cataract Surgery Take?
Cataract surgery takes approximately 15-20 minutes. After the operation, the patient can be discharged on the same day. If the person has cataracts in both eyes, the operation is performed at intervals determined by the doctor; both eyes are intervened at certain intervals.
What is the Treatment of Cataract?
The only treatment for cataract is surgery. The clouded lens is removed by surgery. When the natural lens is removed, the eye is deprived of a refractive power of 10 at a distance and 13 at near. For this reason, during cataract surgery, a new lens is implanted into the eye with the strength the eye needs. Today, the most common cataract surgery method is phacoemulsification, or phaco for short. These operations can be performed under drip, local or general anesthesia depending on the surgeon’s preference. It is often mistakenly thought to be laser cataract surgery as there are usually no stitches. In fact, there is also laser cataract surgery. In femtosecond laser phaco surgery, some surgical interventions are performed with a laser first. Phaco surgery is completed with some stages ready. Femtosecond laser technology, which works with the help of a computer, is the most advanced technology in the world in cataract operations, thus increasing the safety of surgery and ensuring perfect positioning of the newly inserted lens. Another factor as important as the technologies used in cataract treatment is the artificial lenses that will be implanted into the eye. During cataract surgery, astigmatism can be corrected and the need for near and far glasses can be eliminated with the lenses implanted into the eye. If a single-focal lens is implanted without taking astigmatism into consideration, the patient will wear both near and far glasses. If a single-focal lens that corrects astigmatism is worn, the patient sees far without glasses and wears near glasses while reading. Patients who want to see far and near without glasses can be fitted with special lenses such as trifocal, EDOF, new technology monofocal or adaptive lenses. It is also possible to provide a glasses-free life by performing an early cataract surgery and fitting special lenses in suitable patients of near spectacle age without cataracts.
What should be considered for cataract surgery?
Cataract treatment is performed painlessly with the development of modern techniques. In the success of cataract treatment, the technologies, consumables and the quality of the lens are as important as the experience of the physician.
When the right lens is selected, the person can see clearly after surgery and the quality of vision adds comfort to his/her life. Many important factors such as age, lifestyle, hobbies, profession and the structure of the eye should be taken into consideration when choosing a lens. The lenses used must have undergone adequate tests and their success must be proven with a quality certificate.
Is Cataract Surgery Risky?
As with all surgeries, there are some risks in cataract surgery. However, thanks to the developing technology and methods, the success of cataract surgeries is quite high. In addition, with timely intervention without delay, the risks of complications that may occur in cataract surgery will be minimized. Lens selection and correct application is the most important stage of this surgery. The type of lens to be implanted in the patient’s eye, its degree, the angle at which it will be placed in the eye, and the lens number (which can correct both astigmatism, distance and near) must be determined exactly after the measurements made. It is not possible for these lenses to cause allergies or not to be accepted by the tissue. The intraocular lenses inserted during surgery remain in the patient’s eye for life.
Frequently Asked Questions
- Will I regain my vision after cataract surgery?
If there is no reason other than cataract in the eye that reduces vision, an eye that has undergone cataract surgery regains its former vision.
- Will I wear glasses after cataract surgery?
During cataract surgery, the number of the lens placed in the eye can be adjusted to see far or near clearly. Thus, if the eye of the operated person is zeroed for distance, he/she can see far without glasses, but needs to wear glasses for near. If the lens implanted during the surgery makes the eye myopic, the person will be able to see near without glasses, but will need glasses for distance. If a multifocal lens is preferred, myopia, hyperopia and astigmatism problems can be solved with a single lens.
- Do I need to have cataract surgery for my vision to deteriorate?
No, surgery can be performed at any stage of the cataract, starting from the onset of cataract formation and decrease in vision.
- Does having cataract surgery at a very late stage (advanced cataract) affect the success of the surgery?
Yes, surgery for very advanced cataracts is more likely to have problems. Also, the duration of surgery is longer in advanced cataracts.
- Do I need to be anesthetized for cataract surgery?
Narcosis (general anesthesia) is not required for cataract surgery except for pediatric and infant patients. In cataract surgery, different types of local anesthesia are used for adult patients. The eye is numbed by injection around the eye and at the same time eye movements are eliminated.
- If I need laser surgery after cataract surgery, can I have it?
Laser surgery can be performed if your eye is found suitable after the examination.
- Will my lazy eye improve?
Cataract surgery does not cure lazy eye. There are different treatment methods for lazy eye.
- What is Femtosecond Laser?
Cataract surgery performed with laser is called Femtosecond laser cataract surgery. Femtosecond laser technology has been successfully used in the last 15 years to create flaps in refractive surgery.
This technology, popularly known as bladeless laser surgery, has also been used in cataract surgery in recent years. In this way, some of the maneuvers that the surgeon needs to perform during the operation can be performed before the operation with the femtosecond laser, without touching the eye and in a controlled manner. The use of a femtosecond laser makes the surgery easier and safer as it performs some stages of the surgery in advance. In addition, a femtosecond laser also marks the implantation axis of astigmatic lenses and helps to implant the astigmatic lens in the most accurate position.
- How is Cataract Surgery Performed with Femtosecond Laser?
During the surgery, the eye is anesthetized with the help of drops, so that the surgery is performed without narcosis, needles, knives and pain. The most important feature of the laser technology called “Femtosecond Laser”, which is also popularly referred to as knife-free cataract surgery, is that the most important stages of the surgery are performed without the use of a knife. In cataract surgeries, although rare, some complications that cannot be prevented by human hands can be seen. The experience of the doctor is very important to prevent these complications. With femtosecond laser cataract surgery, the risk of complications will be significantly lower.
“Femtosecond laser” technology also ensures the most accurate placement of the lens implanted into the eye. This helps us to get the most accurate result, especially with multifocal or astigmatic lenses.
Cataract operations with femtosecond laser is the most ideal method for cataract patients today as it provides faster recovery and fewer complications.
Cataract Treatment with Phaco Method
What is Phaco Surgery?
Phaco is the most widely used cataract surgery method today. Its most important feature is that it is performed through small incisions. Since it is usually performed under drip anesthesia and no stitches are placed, it is commonly thought of as ‘laser cataract surgery’. Cataract treatment is a very important surgery that requires microsurgery. The success of the surgery is directly affected by the experience of the physician, preoperative examinations, sterilization of the operating room where the surgery is performed, the quality and sterilization of the materials used.
How is Phaco Surgery Performed?
For phaco surgery, the front shell of the natural lens is first peeled off. Then, the lens is broken into particles and removed from the eye with the phaco device working with ultrasonic wave power, which is inserted into the eye through a 2.2 mm tunnel. After the inside of the lens is completely cleaned, a new lens of the strength required by the eye is inserted into the posterior capsule sac left in place. The incision sites are inflated and antibiotics are administered into the eye and the surgery is terminated.
What are the Features of the Phaco Device?
In the Phaco (Phaco Emulsification) method, patients usually think that they will be treated with a laser device. However, contrary to popular belief, the Phaco device removes the cataractous lens with sound waves, not laser. In laser cataract surgery, the stage of peeling the front shell of the lens and breaking the lens is performed using a femtosecond laser before the surgery begins. Then phaco is applied.
Intraocular Lenses Used in Cataract and Clear Lens Surgery
Our natural lens inside our eye has a refractive power of +10 degrees. Until the forties, our natural lens adapts when looking close and gains 3 numbers close. In our forties, we start to lose our adaptive reflex when looking close and we start to wear close glasses. Frosting of our natural lens is called cataract. When the cataract is surgically removed, our eye is deprived of refractive power of 10 at a distance and 13 at near. Therefore, in cataract surgery, intraocular lenses of the strength required by the eye are inserted into the eye.
Today, cataract surgery can be performed through very small incisions, so astigmatism control is possible. In addition, the technology and formulas used to calculate the lens required by the eye have also improved considerably. When the right intraocular lens is selected, cataract surgery can be considered as a return to life without glasses.
Especially in hypermetropes who have reached the age of near glasses, even if cataracts have not yet started, we can provide a glasses-free life by performing an early cataract surgery and placing appropriate intraocular lenses. When we take the natural lens, which is the reason why the number of the eye is constantly changing, and place a fixed lens inside the eye, there will be no change in the numbers anymore.
How many types of intraocular lenses are there?
Lenses with only one focus are called monofocal, single focus lenses. Since these lenses do not provide a solution to astigmatism, they aim to show distance without glasses in people with low astigmatism. Patients with monofocal lenses need +2.25 near glasses to be able to read.
Monofocal lenses that also correct astigmatism are called toric monofocal lenses. These patients also need +2.25 near glasses.
The newest type of monofocal (+) monofocal lenses provide some support at intermediate distances, but not very close. They especially aim to show the step distance and the table top.
Depth-of-focus-enhanced (EDOF) lenses also give good support, not so close but at medium distances. They are especially good for showing cell phones and computers.
Lenses with a focus at near and far are called bifocal lenses. These lenses show far and near together. Near is clear only at a certain distance.
Today, the most common trifocal lenses, Trifocal lenses are preferred. Because in these lenses, near is seen not only at a distance but also at a distance of 40-80 cm in depth.
Things to Consider After Intraocular Lens Surgery
After intraocular lens surgery, postoperative controls are performed and the patient is discharged on the same day. It is very important for the application of drops given at intervals determined by the doctor and for the healing process. Usually, a control examination is performed the next day after the operation.
Is There Blurriness After Intraocular Lens Surgery?
Blurred vision may occur on the first day after intraocular lens surgery. This is normal and temporary. Generally, the reason for blurred vision after intraocular lens surgery is due to the drops used during the operation and edema in the cornea. However, you will notice that your vision becomes clearer within a few days after the operation.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
About Presbyopia
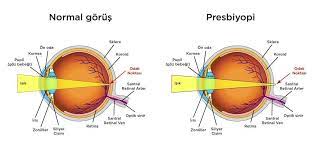
What is Presbyopia (Near Vision Disorder)?
Presbyopia is a condition in which the eyes lose the ability to see nearby objects clearly over time. Many patients wonder what presbyopia means. In colloquial terms, Presbyopia is a near vision problem. If we explain it with its full definition; When a distant object comes closer, the stimulus reaching the brain is evaluated and transmitted to the eye. Here, in the region of the eye called the “ciliary body”, the fibers connected to it are stretched or relaxed by the contraction and relaxation of the muscles. This movement of the fibers causes the lens to sharpen or thicken, increasing its refractive power. The eye loses its near vision due to age. Although it has not been conclusively proven, the closest theory for the age-related loss of this ability is the cell aging theory. This theory states that our eye cells lose this ability as our hair turns gray with age. Therefore, the problem can be considered as a physiological aging rather than a pathological problem.
How Does Presbyopia (Near Vision Impairment) Develop?
The development of presbyopia starts as follows; our natural lens, which has a refractive refraction of 10 degrees at a distance, allows us to see up close by gaining 3 more numbers thanks to our adaptive reflex. The lens inside our eyes has a structure that can change shape. Thanks to our adaptive reflex, it allows us to focus on the near by sharpening our lens when objects come closer.
At what age does nearsightedness (presbyopia) occur?
Nearsightedness begins in the forties when the elasticity of our natural lens deteriorates and gradually loses its power to focus near. In this situation, people with good distance vision need a pair of near-sighted glasses around size 1 in their 40s, size 2 in their 50s and size 3 in their 60s. Low myopic eyes are already refractive enough, so they do not need to focus on the near, they can see the near without glasses.
What are the Symptoms of Presbyopia (Near Vision Impairment)?
Presbyopia is a slowly developing eye problem. Some symptoms of presbyopia include;
Difficulty reading small print,
Having to keep reading materials (books, magazines, menus, digital devices, labels, etc.) at arm’s length,
This includes difficulty seeing nearby objects.
Presbyopia can also cause visual fatigue, such as headaches and eye strain, which makes other near vision tasks less comfortable and more tiring.
How is presbyopia (near vision impairment) treated?
Intraocular trifocal lens operations are one of the most widely used near vision surgery methods for the treatment of presbyopia all over the world. Patient selection is very important for this treatment. The patient must first undergo a detailed eye examination and the suitability of the operation must be checked as a result of the examinations. Not every patient may be suitable for near vision impairment treatment.
Near Vision Impairment (Presbyopia) Surgery
Presbyopia surgery is usually performed with trifocal lens treatment. With this surgery, the patient’s near vision impairment can be corrected. In the treatment to be applied, attention should be paid to whether near or far vision is more important for the patient. Another important issue in patient selection is the patient’s pupil size. Since the treatment is a cataract surgery, patients can find a solution to both cataract problems and distance and near vision problems in the same session. Another option for the treatment of near vision problems is laser treatment.
When Does Near Vision Impairment (Presbyopia) Start?
Presbyopia, which usually begins to make itself noticeable shortly after the age of 40, is considered a normal part of aging.
What can be done to prevent the progression of presbyopia and for early diagnosis?
There is no way to stop or prevent presbyopia from progressing. What is desired to be done in the treatment of presbyopia is to ensure that the image similar to the image when the eye focuses is seen again. Glasses or contact lenses can be given to provide this image. For a complete treatment, refractive surgery or intraocular lens operations can be performed depending on the suitability of the patient’s eye condition.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
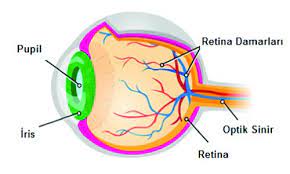
What is Retina?
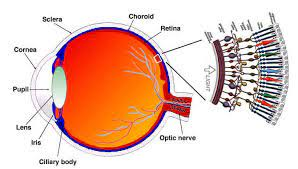
What is Retina?
The retina is a network of visual cells that covers the back wall of the eyeball like wallpaper. At the same time, the retina consists of 10 layers, the retina is the most complex and sensitive part of the eye. The retina allows light to be transmitted to our brain as an image and this is how we see. Problems occurring in the retina are not an eye disorder, but an eye disease. Early diagnosis is very important at this point. If you have one or more of the following symptoms, you should definitely be examined by a retina doctor.
- Symptoms of Retinal Diseases
- Sudden or slow loss of vision
- Broken-curved vision
- Light flashes
- Dark objects flying in front of the eyes (hoverflies)
- Screening of vision
- Temporary and short-term vision loss
- Dark areas in the field of vision
What are Retinal Diseases?
- Bleeding due to diabetes and hypertension
- Retinal vascular occlusions
- Retinal detachments / tears
- Yellow spot disease
- Congenital retinal diseases
- Fluid accumulation under the retina, retinal edema
- Macular holes
- Vitreoretinal surface disorders
- Retinal tumors
Negative Effects of Sugar and Hypertension on the Retina
Diabetes and hypertension have a negative impact on all systems of the body, with the eyes being the first to suffer the greatest negative impact. Diabetes and hypertension diseases can cause vasodilation and permeability disorders in the retina. For this reason, especially diabetics and hypertensive patients should be monitored by an ophthalmologist to protect eye health.
What Causes Retinal Tears?
Retinal tears are divided into three as retinal hole, horseshoe tear and disinsertion. The most common type of tear that causes retinal detachment is the so-called horseshoe tear, which is mostly in the form of center-facing tears. These tears cause photopsia (light vision) complaints in the patient. If these tears are accompanied by tears in the vessels, the patient may also complain of foggy vision. The retinal hole is seen in oval shapes, but retinal holes do not cause symptoms but are considered as a natural freeze of aging. Retinal tears are considered as a natural consequence of aging. However, in some cases, retinal holes may occur as a result of a blow to the eye or an operation. It is very important for eye health to treat these holes in the retina without delay.
- Retinal Tear Symptoms
- Light flashes
- Narrowing of vision
- Curtain in the eye
- Blurred vision
Retinal Tear Laser Treatment Prices
The process of treating retinal tears with photocoagulation is called argon laser therapy. It treats the damaged tissues of the retina and prevents further deterioration of the tissues. This procedure is performed painlessly with drip anesthesia. Retinal tear laser treatment prices can be determined after the examination.
About Retina Surgery
Retinal surgery is performed after a doctor determines the damage to the retina. Major diseases such as retinal detachment are treated with surgical interventions, while small holes in the retina can be treated with laser.
However, early diagnosis, preventive medical treatment and correct surgical intervention before it is too late are of vital importance.
Frequently Asked Questions
What Should Be Done After Laser Treatment of Retinal Tear?
Anesthesia applied after retinal tear treatment may cause blurred vision due to drops and procedure. Therefore, driving is not recommended for the first few hours after treatment. The patient does not need to stay in the hospital after treatment. It will be sufficient to come to the control at the intervals determined by the doctor after the treatment.
Does Blurred Vision Occur After Retina Surgery?
The drops to be applied to the eye and the procedures performed may cause blurred vision in the patient. For this reason, the patient is informed before the treatment to come with people who can accompany the patient after the treatment to be applied.
Does Retinal Detachment Make You Blind?
If retinal detachment is not treated immediately, it may cause partial or complete loss of vision.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Retinal Detachment?
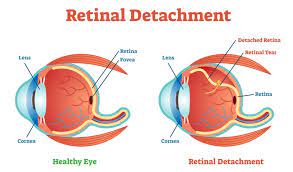
What is Retinal Detachment?
Retinal detachment is caused by tears or holes in the retina. It is often seen in patients with high myopia. It can occur at any age, more often in middle age and older.
The retinal layer stretches as the anteroposterior diameter of the eye increases and the tensile area on it begins to thin and deteriorate. Some familial or degenerative diseases and infections may also cause thinning and deterioration around the retina. In the meantime, for the same reasons, the vitreous gel begins to lose its homogeneity and deteriorate, the gel consistency changes and gradually separates from the retina. This separation is called vitreous detachment. In the meantime, the vitreous tissue, which shrinks and becomes opaque in places, is perceived by the person as flies flying in front of the eye or a smoke screen as it passes through the visual axis. If retinal detachment is not treated immediately, it may cause partial or complete loss of vision.
What are the Causes and Symptoms of Retinal Detachment?
- Retinal diseases can result in permanent blindness if left untreated.
- Main symptoms of retinal detachment;
- Flashes of light,
- fly swatting
- symptoms such as sudden loss of vision
- These symptoms may be a harbinger of retinal detachment.
How is Retinal Detachment Treatment Process Realized?
For the treatment of retinal detachment, early diagnosis, detailed examination, timely and most importantly correct treatment can prevent consequences that may lead to vision loss. Retinal surgeries are sensitive surgeries that require the use of high technology with great sterilization measures, otherwise they can lead to vision loss.
When the macula (the visual center of the eye) detaches from the underlying tissue, central vision is lost. In long-term detachments, the intraocular balance is disrupted and the eyeball begins to shrink. Sudden, severe or penetrating blows to the eye can cause detachment. In diabetes and some degenerative diseases, bands may form in the vitreous that pull the retina and traction-induced detachments may develop. Rarely, detachment can also develop without any tear in the eye in some infections, tumors or blood pressure crises that occur especially during pregnancy.
What is the Recovery Process After Retinal Detachment Surgery?
The patient can return to his/her daily life within 7 – 10 days after the operation. Full recovery of vision after retinal detachment surgery is observed within 1 – 2 months. After the operation, control examinations should be performed at intervals determined by the ophthalmologist.
Frequently Asked Questions
Does Eye Bleeding Occur After Retinal Detachment Surgery?
Blurred vision and bloodshot eyes are possible conditions after retinal treatments. This condition will completely resolve during the healing process. Therefore, there is no need to worry if there is blood in the eyes after the operation.
How Long Does Retinal Detachment Surgery Take?
Detachment surgery takes approximately 20 – 30 minutes for each eye.
Can Retinal Detachment Recur?
Retinal detachment is the separation of the inner surface of the eyeball. Many factors can cause this to happen. It is possible for a detachment that has been treated to occur again.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Bionic Eye Treatment

What is Retinitis Pigmentosa Disease (Chicken Black)?
Retinitis pigmentosa, popularly known as chicken black or night blindness, is a genetically inherited retinal disease. Retinitis pigmentosa (chicken black) disease usually starts in the 10s and continues over time with effects such as narrowing of vision, reduction of colors and light. Recognizing this disease, which varies from person to person, at an early age is very important for the course of treatment. For this reason, it is recommended that parents observe their children and check whether their vision is healthy under dim light at intervals.
What is a Bionic Eye?
Bionic eye is a treatment method for people with vision loss due to retinitis pigmentosa (chicken black) disease, in which the light receptors in the eye are absent or severely damaged, but the optic nerves remain intact. Retinitis pigmentosa, popularly called chicken black or night blindness, is a very serious eye disease that shows very different genetic transition characteristics, is more common in consanguineous marriages and leads to total blindness. The aim of bionic eye treatment is to increase the visual acuity of people with visual impairment due to retinitis pigmentosa by increasing their perception of shadow or light.
Who Can Receive Bionic Eye Treatment?
- People who have no or damaged light receptors in the eye,
- People with intact optic nerves,
- Persons over 25 years of age,
- People who can feel light in at least one eye,
- It can be applied to people with vision loss due to retinitis pigmentosa disease.
How Does Bionic Eye Treatment Work?
Bionic eye treatment is the process of implanting a chip in the visual center of the person and transmitting images to the visual center with special glasses.
How Does Bionic Eye Treatment Work?
The retinal implant (Bionic Eye / Argus II Retinal Prosthesis System), which is placed inside the person’s eye, consists of two parts. The device works by means of an electronic eye that detects objects in the field of view. The special glasses have a camera on them and are connected to a power device to activate the implant.
What is the post-treatment process?
After the treatment, it is aimed for the person to interpret objects by perceiving light. The person starts to see in black and white, shadow and light perception increases. After the treatment, a three-month rehabilitation process begins and the person’s vision improves. In this process, the person is supported in perceiving people and objects and how to interpret what they see with the bionic eye.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
About Pediatric Eye Health

Child Eye Health
Children are most often unable to express their disease. Many important eye diseases occur at a young age. However, successful results can be achieved with early diagnosis and correct treatment.
What should be done to protect the eye health of children in the 0-16 age group?
The first eye examination should be done at 2 – 3 months of age. With the examination, congenital eye diseases are screened.
For the next process, it should continue as the first 1 year of age and annual follow-ups. This will facilitate the diagnosis and treatment of existing or potential eye problems.
What are the Symptoms of Eye Disorders in Children?
- Eye slippage (strabismus)
- Do not track
- Redness or watering of the eye
- Tremor in the eye
- Squinting or closing one eye
- White or hazy color in the pupil that should appear black
- Constantly holding objects close to your eyes
- Don’t look with your head tilted to one side
- Do not rub your eyes often
- Premature birth
- Family history of lazy eye
- Family history of eye disorder
In case of the above symptoms, you should immediately consult an ophthalmologist (pediatric ophthalmologist) specialized in pediatric eye diseases.
PEDIATRIC EYE DISEASES
Eye diseases in children can occur from birth or in later years. Pediatric eye diseases seen from birth are usually hereditary. Pediatric eye diseases can cause functional problems in the eye, depending on the structurally affected area. For this reason, it is recommended that children have routine eye examinations every year.
What are the Most Common Eye Diseases in Children?
Bursting and Blood in the Eye
Babies may develop burrs and blood in the first 15 days after birth. However, in long-term burrs, if the color of the burr is present, the nature of the discharge in the eye is important. In this case, treatment should be started by an ophthalmologist. Again, redness and burrs that occur after birth may not require special treatments. However, if redness and accompanying burrs persist for more than 1-2 days, it requires an eye examination and drops may be recommended after the examination.
Redness in the eye can sometimes be a condition involving the cornea. If the baby squints or has watery eyes, an ophthalmologist should be consulted.
Watery Eyes
Unilateral or bilateral watery eyes that start immediately or within 2 weeks after birth may usually be related to blockage or stenosis of the tear ducts. If the obstruction is complete, watering in the eye may occur frequently and with burring. In this case, there is typically not much redness in the eye. If the eye is burring, treatment may require an eye examination and an appropriate drop and appropriate massage to open the canal together. In general, this condition may disappear with massage within the first 6 months. If watering continues until the age of 1 year and burrs are seen frequently, canal opening treatment can be applied with probing.
Strabismus
Strabismus is a condition in which both eyes lose their parallelism with each other. There are 6 extraocular muscles in each eye. A lack or excess of strength in one or more of them can cause strabismus. While one eye looks straight, the other can shift inward, outward, upward or downward. In some cases, the shift is present in both eyes. The shift in the eyes may be permanent or temporary depending on the cause of strabismus. There is no single cause for strabismus. Strabismus can occur for different reasons.
Early diagnosis is very important in the treatment of strabismus. When it is too late for the first eye examination, children may have aesthetic problems in their eyes as well as lifelong problems with low vision. Immediately after birth and during childhood, children should be regularly checked by a specialist ophthalmologist, even if they have no eye complaints.
AMBLYOPIA
Amblyopia is lazy vision. It can occur in one or both eyes. Visual acuity is not complete, amblyopia may develop in both eyes in bilateral high refractive errors. In patients with a high refractive error difference between the two eyes, laziness may occur on the side with the high refractive error. In addition, unilateral strabismus, droopy lid covering the visual axis, congenital cataracts are also among the causes of amblyopia. It should be detected and treated early. The best response to treatment is obtained until the age of 5-6.
What are other eye diseases seen in children?
- Refractive errors
- Eyelid diseases
- Cataract
- Corneal diseases
- Glaucoma
- Trauma
- Retina and optic nerve diseases
- Retinopathy of Prematurity (ROP)
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Retinopathy of Prematurity?
What is Retinopathy of Prematurity?
Retinopathy of Prematurity is defined as one of the most important health problems seen in the eyes of premature babies. The vessels in the eyes of babies develop until they are born. In premature babies, this development is not completed and continues after birth.
Oxygen given in high concentrations to keep premature babies alive causes abnormal development of the vessels in the eye. As a result, Retinopathy of Prematurity, also known as ROP, occurs in the retinas of babies with incomplete vascularization. If not treated early, it can cause blindness in both eyes. For this reason, premature babies should definitely be examined by an ophthalmologist.
In Which Babies Is Retinopathy of Prematurity Most Common?
A normal pregnancy lasts 40 weeks or 280 days. If the baby is born before the completion of 37 weeks, the baby is considered premature. Babies born weighing less than 2,500 grams are called low birth weight babies. Two thirds of these babies are premature.
What are the Risk Factors for Retinopathy of Prematurity?
The most common group with Retinopathy of Prematurity is those born under 1,000 grams. The risk factors for retinopathy of prematurity apply to all babies born under 1500 grams and before the 32nd week. Therefore, premature babies must be examined for ROP.
Early diagnosis and treatment of ROP in newborn babies is possible with the collaboration of specialized pediatricians and ophthalmologists. In addition, lung and cardiovascular diseases, severe infections and problems in the brain also increase the risk of retinopathy. It can be treated with early diagnosis and can lead to blindness in both eyes when it is late.
When should babies have an eye examination?
An eye examination should be performed between 4-6 weeks after birth. Success in the treatment of ROP, which has five stages from mild to severe, is related to the stage of the disease. Follow-up is sufficient in the first two stages, and laser and cryo treatment should be started from the third stage. Because the disease gives the best results in the third stage.
Eye examination of all newborn babies within the first month is very important not only for ROP, but also for many eye diseases, such as eye pressure, lazy eye, tear duct obstruction and strabismus, in terms of timely diagnosis and successful treatment.
Pediatric Anesthesia
If anesthesia is required in the treatment of pediatric eye diseases, it is applied by anesthesiologists specialized in pediatric anesthesia. Treatment is performed in sterile operating rooms with tables designed for pediatric patients and disposable medical consumables.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Strabismus?

What is strabismus?
Strabismus is when the two eyes look in different directions. One eye looks straight ahead while the other looks inward, outward, upward or downward. Patients with strabismus can sometimes look straight with both eyes in different head positions, such as tilting their head to the right and left. Sometimes strabismus can manifest itself with such abnormalities in head position.
Who Has Strabismus?
Although it is usually seen in children, it can also occur at older ages. Strabismus is found in 5% of all children and 1% of adults. It occurs equally in both sexes. Except for some rare types, it usually does not show a genetic inheritance.
Do Our Two Eyes Work Together?
Vision is an event that takes place in the brain. The eye is the organ of emotional perception. The image formed as a result of the stimuli received by the retina is transmitted to the visual cortex in the brain via the optic nerve and visual pathways. In addition to this emotional system, there is a motor system (extraocular muscles) that is used to turn both eyes to the object of interest and create the same image on both retinas. Normally, our eyes look at the same point and the two images transmitted from both eyes to our brain are fused (fusion) by our brain, allowing us to see in three dimensions (stereopsis). In short, it is provided by the movement centers in our eyes and brain and 6 muscles located outside the eye.
When one eye looks in a different direction, two very different images will come to our brain. In this case, the image coming to the brain from the eye looking in the opposite direction will either be ignored (amblyopia development) or suppressed (suppression development). The brain will only accept the image transmitted by the opposite eye. If this happens in childhood, the child develops adaptation mechanisms that lead to serious problems such as lack of depth perception and poor vision in the sliding eye (laziness = amblyopia). In strabismus that occurs in adulthood, the brain does not make adaptation mechanisms as it does in children and double vision occurs by accepting both images.
What Causes Strabismus?
The cause is not known exactly. Genetic transmission can be seen in some families. Strabismus may occur only due to spectacle disorder or congenital brain damage, mongolism, brain tumors, cataracts that reduce vision, eye injuries or tumors may cause strabismus.
If strabismus has not been present in an adult before and has just occurred, diabetes, multiple sclerosis, thyroid disease, myasthenia gravis, other diseases involving the central nervous system should be investigated.
What are the Symptoms of Strabismus?
- Eyes looking in the same direction
- Loss of three-dimensional image
- Blurred vision
- Head or face turned to one side
- Eye watering
- Pain
- Headache
- Double vision
There may also be symptoms such as tilting the head to one side or turning the face to one side to use one or both eyes in a sunny environment.
It is very important for the visual development of all children to be checked by an ophthalmologist within the first 3 years of life. If there is someone else in the family with strabismus or lazy eye, this examination should be done before the age of 3.
In adults, strabismus since childhood, apart from cosmetic discomfort, if the patient is not treated well, the vision problem may be lazy eye. However, if strabismus occurs at an advanced age, the most common symptom is double vision. Some adults may have symptoms such as pain in the eye, headache, constant head tilt.
What are the Types of Strabismus?
Although there are many classifications, none of them is perfect. Strabismus can be classified as paralytic (the angle of misalignment is different in each direction) and non-paralytic (the angle of misalignment is the same in each direction); monocular (only one eye is used) or alternating (both eyes can be used alternately) according to the fixation status of the eyes; those that are corrected with glasses or surgery. It can be classified according to the direction of slippage.
Can Congenital Eye Shifts Occur?
Congenital misalignments can usually occur in the period ranging from 3-6 months to 1 year of age. The angle of misalignment is very high and can be noticed by almost everyone. These types of shifts generally do not develop due to a refractive error (hypermetropia, etc.). Babies may have low or moderate hypermetropia, but even if they wear glasses, it does not correct the shift. These types of shifts may be accompanied by upward shifts. It is important not to wait and to act early in their treatment. The ideal is surgical correction of the shift at the age of 1.5 years. Thus, the baby can continue his/her life with a perspective where he/she can use both eyes, not just one eye.
What is Pseudo Strabismus?
Babies’ eyes seem to turn inward. This may be because the root of the nose is wider or there is a skin fold (epican) on the inside of the eyelid. Especially when looking sideways, it gives the impression that the child’s eye is shifting inward. This condition, which disappears with age, is called false strabismus. The difference between false and true strabismus can only be diagnosed by the doctor. However, examination with the light test shows that the corneal light reflections are symmetrical. There is no movement of the eyes with closure tests. In addition, unilateral exophthalmus, high myopia and facial asymmetry are other causes of false strabismus.
Why does double vision occur?
In an adult with strabismus, the image in one eye falls on the fovea, while in the other eye it falls on a point outside the fovea. Unlike children, adults cannot ignore or suppress the image coming from the eye facing in a different direction. This causes double vision. This is treated by closing one eye, giving special prismatic glasses or surgically repositioning the eyes to the correct position.
What is lazy eye (amblyopia)?
The development of vision is a process that continues incrementally after the child is born and this process develops rapidly in the first 2 years of life. This development continues gradually until the age of 7. If a child cannot use one eye sufficiently, the vision of that eye will not develop. Since the visual system completes its development at the age of 9 at the latest, vision no longer develops after this time. Since the visual system completes its development at the age of 9 at the latest, vision can no longer be changed after this time. Healthy vision in children occurs when both eyes are in a normal position and both eyes receive equal stimuli. Lazy vision is the loss of vision due to the failure to develop normal vision in one eye in early childhood. It is seen in 2-3% of the population. The most common causes are strabismus, eye disorders (myopia, hyperopia, astigmatism) and cataracts, which are rarely seen in children.
Lazy eye is treated by closing the good-sighted eye for a certain period of time. Amblyopia can be successfully treated in patients with early diagnosis. The later treatment is started, the lower the chance of success.
Remember that the success of amblyopia treatment depends on the severity of amblyopia and the age at which treatment begins. Treatment continues until the age of 9. After this age, treatment is no longer successful. For this reason, it is important to have an eye examination at the age of 3 and before starting primary school.
Eye Shifts Due to Refractive Error
Eye shifts due to refractive error are mostly seen between the ages of 1-1.5 years and 3 years. In these children with moderate to high hyperopia, the misalignment can be either completely or partially corrected with glasses. Their history is typical. The shift may start suddenly or may occur after a fever or a fall. They often have a higher number in one eye and are at risk of lazy eye. Most of these types of misalignments can be treated with glasses and closure therapy. If the misalignment does not resolve completely and vision is impaired when both eyes are viewed at the same time, then strabismus surgery may be required for the misalignment.
Eye shifts due to muscle paralysis
Muscle paralysis can occur in infancy and childhood after trauma, especially head trauma, difficult births and high fever. Rarely, it may occur due to tumors, cysts or structural disorders in the head. In adults, it can also occur after trauma or in diseases involving the central nervous system such as diabetes, thyroid diseases and MS.
In this type of misalignment, there is typically double vision and while it disappears quickly in younger ages, it is permanent in older age groups. Typically, the head is tilted to the side and one eye is squinted. In children, if the angle of misalignment is too high, the brain immediately deactivates the misaligned eye to eliminate double vision in a short period of time and laziness starts in that eye. In adults, double vision is present as long as there is a shift and causes head position. Double vision is a condition that makes life very difficult. Most of the shifts due to strokes may disappear within a year. Therefore, it is necessary to wait. In this period, no surgical intervention is usually applied, but botox application is frequently performed to recover the slippage in the earlier period and to improve double vision. If the eye shift angle is low, double vision can be prevented with prismatic special glasses.
Eye Shifts Seen in Older Age Groups
Although they are rarely seen in infancy, they usually start in childhood and adolescence. They are usually seen as an outward shift. They start intermittently, there is not always a shift, it occurs when the eye is distracted or looking away. It can be caused by overwork of the external muscles or weakness of the internal muscles. Surgical intervention is required for fixed shifts that affect vision in both eyes. In some cases, orthoptic treatments may be beneficial in intermittent strabismus.
Special Strabismus
Sometimes there are congenital structural and functional defects in the eye muscles or in the nerves that move these muscles, which can lead to misalignments. If they lead to lazy eye and cause a pronounced head position, they should be treated to help the child regain vision in both eyes. Glasses, closure and orthoptic treatments, surgical treatment when necessary are applied in these slips.
How is strabismus diagnosed?
What is Inspection?
The relationship of both eyes with each other is examined while the patient looks straight ahead. It is also examined whether the eye movements are compatible when looking to the right, left, up right and left, down right and left.
What is the Light Test?
The physician shines a small flashlight into the patient’s eye from a distance of about 30-35 cm and from across the patient. While the patient looks at this light, he/she watches the light reflection on his/her cornea. Normally, these reflections should be symmetrical and in the center of the pupil in both eyes. If the light reflection in one eye is not in the center of the pupil, strabismus is detected. This method called “Hirschberg test” is a rough examination and does not make a definitive diagnosis. The patient should also be evaluated while looking at a picture or object approximately 5 cm away.
What is the Closure Test?
The physician closes one eye while the patient looks at a point and watches the movement of the other eye. When the healthy eye is closed, the exposed eye will fixate and a movement is seen according to the type of shift (the eye that shifts inward will move outward to come to the center). This test can be performed alternately between the two eyes, so bilateral (alternating) strabismus can also be recognized.
How is strabismus treated?
The aim of treatment is to preserve vision, bring the eyes back to a parallel position and restore binocular vision. The age of onset of strabismus, whether it is in both eyes or in one eye, and concomitant refractive errors are important in determining the type of treatment. Treatment includes glasses, eye exercises, prismatic lenses, Botox injections into the extraocular muscles or surgery.
It is very important to first correct the refractive error with spectacle treatment in a child with slippage and eye disorder. Many types of slippage fall into the group called accommodative strabismus (corrected with glasses). When the child’s eye defect is corrected, that is, when the child wears glasses, the strabismus disappears (the eyes come to the midline when the child wears glasses), but when the glasses are removed, the eyes shift again. The treatment for this type of strabismus is wearing glasses. Surgery is not performed in this group of patients.
In a group of strabismus, wearing glasses due to eye disorder does not change the strabismus angle. The treatment approach for these is surgery. It should be known that if the child wears glasses before surgery, he/she will continue to wear them after surgery. Strabismus surgery is usually performed under general anesthesia. Like all surgeries, this surgery has complications such as bleeding and infection. However, strabismus surgery is a reliable and accepted method for treatment and has been practiced for more than a century.
The diagnosis and treatment of strabismus should be performed by a specialist physician and the treatment should be completed before the age of 7. Every child should be examined at least once before primary school age, even if there are no complaints or symptoms. Ideally, this examination should be performed at the age of 3-4 years.
How is Orthoptic Treatment Performed in Strabismus?
Orthoptic treatments are physical therapy of the eye muscles. It is applied to strengthen some muscles and the ability to see with both eyes. Strengthening the ability to see with both eyes stabilizes or gains the sense of depth. This function of our eyes is very important in our daily life as well as keeping the eyes parallel. It allows us to be more comfortable and successful while driving a car, playing sports that require distance and time adjustments such as basketball and tennis.
How is surgical treatment applied in strabismus?
Congenital strabismus usually does not require glasses and requires surgery in the early period (6 months – 1 year of age). The majority of strabismus occurs around the age of 2-3 years and can usually be fully corrected with glasses. Surgical treatment is required for those that do not improve despite wearing glasses. Strabismus surgeries are usually performed under general anesthesia. Anesthesia is administered by physicians specialized in pediatric anesthesia. With early diagnosis and treatment of strabismus, lazy eye can be prevented and 3D vision can be achieved. For this reason, every child with suspected strabismus should be taken to a strabismus specialist ophthalmologist before reaching a certain age.
Can Botox be used in strabismus treatment?
Botulinum Toxin (BOTOX) can also be applied in some strabismus treatments. Botox is effective and can be used therapeutically in strabismus caused by paralysis, in patients who have undergone surgery but have not achieved complete recovery, and in patients with strabismus due to goiter disease. Sudden shifts due to strokes usually involve double vision and are very difficult for the patient. The general tendency in this type of strabismus is to wait 6-8 months, but Botox can be applied to reduce double vision during the waiting period. Complete recovery is possible by starting treatment immediately after the strabismus occurs.
Eye Tremor (Nystagmus)
What is Nystagmus?
Nystagmus is the involuntary movement of the eye. It can occur congenitally or during and after infancy. Nystagmus is not a condition that occurs due to a single cause. It can have many different causes. It can also occur without affecting vision. It can be seen with head shaking in infancy. In this group that does not affect vision, nystagmus generally decreases towards primary school and sometimes may disappear completely. However, nystagmus may also occur due to low vision or neurological causes.
How to Treat Eye Tremor (Nystagmus)?
It is important to make a very good diagnostic differentiation of nystagmus patients, as it is due to many causes and treatment options vary. Glasses, telescopic aids, drops, medication and surgery when necessary are the treatments applied to these patients.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Cornea?
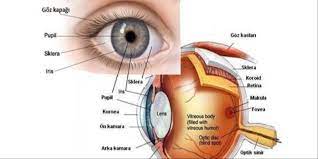
What is Cornea?
The cornea is the curved transparent layer of the eye, which is located at the very front of the eye, has the task of focusing light and protecting the eye from external factors, and plays a major role in visual function.
What are the Cornea Examination Methods?
A person who is not an ophthalmologist can evaluate the transparency of the cornea with local light, the brightness of its surface, corneal injuries, corneal sensitivity with the help of a cotton swab. Ophthalmologists use some devices to assess corneal morphology and function;
Biomicroscopy: It is used for binocular examination of the cornea and other structures of the anterior segment. Light beams of different thicknesses are sent from different angles to magnify the biomicroscope and the cornea can be examined. It is the most commonly used routine examination method.
Keratometry: It is the measurement of the refractive power of the cornea. It is used before contact lens and intraocular lens implantation.
Topography: Used for topographic analysis of the anterior surface of the cornea.
Pachymetry: Measurement of corneal thickness.
Specular microscopy: Shows endothelial cell number and structure.
Esthesiometry: Used to evaluate corneal sensitivity.
Examination of the cornea by staining: Defects on the corneal surface can be visualized with “fluorescein and rose bengal” solution.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Keratoconus?
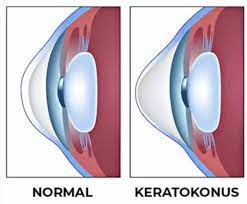
What is Keratoconus?
Keratoconus is a disease caused by the thinning and sharpening of the transparent layer of the eye, the cornea, with progressive myopia and astigmatism. Patients are usually aware of the disease, which usually starts in adolescence, only in their 20s. The disease progresses between the ages of 20-40 and enters a stationary period after the 40s. The cornea is a very important part of the eye. Light enters the eye through the cornea. The cornea refracts or focuses the rays, allowing you to see clearly. In keratoconus, vision is impaired because the cornea deteriorates. Keratoconus can make some activities such as driving, typing on a computer, watching television or reading difficult.
What are the Causes of Keratoconus?
- Ultraviolet rays
- Eye rub
- Environmental factors
- Rigid contact lens wear
- Genetic predisposition
- Chronic eye irritation
Although the cause of Keratoconus is not known exactly, genetics and mechanical traumas play the most important role in its development.
What are the Symptoms of the Disease?
- Persistent allergy or itching in the eye
- Continuously progressive myopia and astigmatism
- Not being able to see clearly despite glasses
- Increased sensitivity to light
- Eye glare
- Straight lines appear bent or wavy
The contact lens worn because the cornea protrudes does not fit the eye or causes discomfort
These symptoms indicate a high risk of keratoconus disease. In such cases, it is useful to be examined by a specialist physician. Because early diagnosis and treatment of keratoconus disease is of great importance in preventing serious vision problems that may occur in the future.
What are Keratoconus Treatments?
Special hard contact lenses are used in the early stages of the disease. However, contact lenses cannot stop the progression of the disease. Stopping the progression of the disease:
Corneal Cross Linking (CCL) -Cross Linking treatment is applied in cases where the steepening of the cornea progresses and the thinning of the cornea gradually increases.
It is more preferred in young people and women before pregnancy, where progression is more common.
Corneal Cross Linking (CCL) is a treatment method that strengthens the collagen and fibrils in the cornea by cross-linking with the help of riboflavin (vitamin B2) and Ultraviolet A rays. It is applied under sterile conditions in the operating room. With this treatment, the forward progression and thinning of the cornea due to the disease is stopped. In almost all patients who undergo cross-linking treatment, vision loss is prevented and at the same time, visual acuity is increased in some patients.
Keratoconus treatment methods
What is Topolaser?
With topolaser, the topographic map of the cornea is created in 3D like a fingerprint and laser treatment is programmed specifically for each patient.
Unlike full Wavefront treatment, this treatment is based on the principle of evaluating only the upper surface irregularity of the cornea.
Who Can Use Topolaser?
Patients who cannot wear contact lenses,
After 6 months, patients who had cross-linking treatment for improved vision,
Patients whose corneal thickness will remain at least 400 microns after laser application,
It can be applied in keratoconus patients who have previously undergone corneal transplantation and have low vision due to high astigmatism.
CCL (CORNEAL CROSS-LINKING)
What is CCL?
Keratoconus is a disease caused by deformity of the transparent layer (cornea), which forms the front part of the eye, as a result of increased curvature and thinning. CCL is one of the treatment methods for keratoconus. The aim of Corneal Cross Linking (CCL) treatment is to strengthen the corneal structure and stop the disease.
What is the CCL (CORNEAL CROSS-LINKING) Treatment Process?
Instillation of Riboflavin (B2 vit)
The eye is numbed with a topical anesthetic drop before the procedure. After topical anesthetic drops, the corneal epithelium is mechanically lifted with a blunt spatula. Riboflavin solution is instilled on the cornea for 30 minutes, 2 drops at 5 minute intervals for 30 minutes.
How is UV light applied?
After 30 minutes, the patient is seated on the biomicroscope. After riboflavin fluorescence is seen in the anterior chamber, the patient is taken back to the operating room. 370 nm UV is applied at a distance of 4-5 cm from the corneal surface in an area of approximately 7 mm for 5-10 minutes. During UV application, 2 drops of Riboflavin are instilled every 1 minute. After the procedure, a bandage contact lens is placed on the eye and the eye is not closed.
UV Cross-Linking (cross-linking at molecular level) Treatment
UV-Cross Linking surgery can stop the progression of keratoconus disease by using UVA light and Riboflavin to act on the collagen molecules of the cornea and increase corneal mechanics.
Results of Applied CCL Operations
Dünyagöz Hospitals’ first scientific study on this subject was presented at the European Cataract and Refractive Surgery Congress (ESCRS, September 8-12, 2007) in Stockholm and was accepted for presentation at the American Academy of Ophthalmology (AAO) Congress.
Which examinations and tests are performed before surgery?
- Visual acuity with and without glasses
- Refractive error with and without drops
- Corneal topography (Orbscan II, Oculus Topography)
- Corneal thickness (Sonogage 50Hz)
- Endothelial count (Specular Microscope, Conan)
- Fundus examination
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Ring Treatment?
What is Ring Treatment?
If keratoconus is not in the advanced stage in patients who cannot wear contact lenses or whose eyes do not fit contact lenses, intra-corneal ring application may be a good alternative. It can be treated by placing intra-corneal rings (INTACS, Keraring, Ferrara) into the channels opened in seconds with Femtosecond Laser under local anesthesia into the cornea.
What are the Corneal Ring Features?
Transparent
Micro size,
Varying in thickness according to the amount of diopters to be corrected,
Placed in the cornea of the eye,
They are special apparatus in the shape of a half-moon and consisting of 2 parts.
These rings are not noticeable from the outside and most importantly, they do not feel like contact lenses. The rings, which can be removed when deemed appropriate by the physician, do not leave any permanent scar that will affect vision as they are not placed in the visual center. The rings, which have different thickness types, are placed according to the degree of keratoconus disease.
When Intacs are placed into the corneal tissue, they eliminate the sharpness and curvature of the cornea caused by keratoconus disease by stretching it like a pulley. In the meantime, the person’s myopia also improves.
The ring placed inside the eye is transparent and compatible with your eye tissue and will remain for a lifetime without causing any problems, and it is also a material that can be removed when desired. After the surgery, it is invisible from the outside and its presence in the eye is not felt.
What are the Ring Types?
There are two types of rings currently in use in the world:
INTACS (Addition Technology): 7 mm diameter hexagonal rings.
KERARING / FERRARA RING (Mediphacos/AJO Company): 5 mm diameter rings with a triangular prism structure.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Dry Eye?
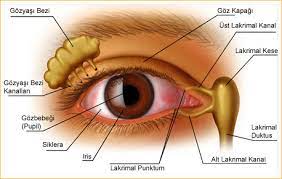
What is Dry Eye?
Dry eye is a condition in which the tear layer that protects the front of the eye and keeps it wet is missing or irregular. This layer protects our eyes from external factors such as dust, wind and some microorganisms. Our cornea, a glassy layer in front of our eyes, is a very sensitive tissue. We need this layer to be regular and healthy in order for it to be healthy and to provide a regular image.
What are the Symptoms of Dry Eye?
The most common complaints of patients with dry eye are;
Burning and stinging sensation
- Redness
- Excessive tearing, feeling of fatigue
- Discomfort when wearing contact lenses
In addition, there may be complaints such as eye pain, itching and redness of the eyes. If patients have dry eyes, they may have difficulty with activities they used to do before. For example, they state that they are not as comfortable at the computer as before or that their eyes get tired quickly.
What are the Causes of Dry Eye?
The cause of dry eye can be patient-related factors as well as environmental factors. Spending long hours on screens such as computers or not using contact lenses correctly are common causes of dry eyes.
In addition, some rheumatic diseases may predispose to dry eye. Medications used for the diseases the patient has can also cause dry eye.
Hormone medications used for hormonal disorders, especially post-menopausal periods in women, anti-systemic drugs used, depression medications that have been widely used especially in recent years are among the common causes of dry eye today.
The reasons that can be counted among environmental factors are that the working environments are not humid enough, working under very high illumination and bright light.
What are the Treatment Methods for Dry Eye?
The most common treatments for dry eye are artificial tear drops and gels. As a result of the evaluation of the patient by the physician, the most suitable artificial tear preparation will be selected. Apart from this, precautions should be taken according to the patient’s life practices.
A patient who is frequently in a humid environment can reduce dry eye complaints by making the environment more humid. A patient who does not pay much attention to the use of contact lenses, a patient who sleeps with lenses at night or a patient who exceeds the duration of use can reduce dry eye complaints by paying attention to these. In addition, some vitamins known to increase tear production may be recommended.
As Our Hospitals Group, we have incorporated LipiFlow treatment, which has been approved by the American Health Organization (FDA). This new LipiFlow treatment is a very small apparatus that is attached to the eyelids without harming the eye and the lids are periodically squeezed and heated to 41.5 degrees and is extremely safe.
In this treatment, which has no side effects on the body or the eye, the lids are regularly squeezed and heated at the same time and the gland is activated by removing the blockage in the ducts of the gland. LipiFlow, which is a treatment to reactivate inactive glands that have lost their activation, has absolutely no side effects on patients. Two purposes are essential when performing this treatment.
First; to replace the missing tears from outside, which is the simplest treatment, artificial tears.
Secondly, to ensure that the patient’s own tears work by activating the inactive glands that have lost their activation.
The layer that covers the tear, which we call the fat layer, ensures that the tear stays in the eye longer and protects the cornea and keeps it healthy. In order to activate this layer, we aim to make the glands work better with LipiFlow treatment.
It has been observed that LipiFlow treatment provides sufficient activation in patients for approximately one year and 18 months. After providing this activation, it is a successful and reliable treatment method that allows those glands to work in some way and get back in order with the treatment protocols.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Conjunctivitis?

What is conjunctivitis?
The conjunctiva is a thin and transparent membrane that covers the inside of the eyelids and the white part of the eyes (sclera). Inflammation of this thin and transparent membrane is called “conjunctivitis”. Conjunctivitis makes the blood vessels larger and more prominent, making the eyes look red. It can occur in one or both eyes.
What are the Symptoms of Conjunctivitis?
- Increase in irrigation
- Pain in the eye
- Itching in the eye
- Excessive burring
- Crusting of eyelashes in the morning
What are the Factors Causing Conjunctivitis?
- Infections (viral and bacterial)
- Allergies
- Environmental factors
What is the treatment for conjunctivitis?
Ophthalmologist prescription eye drops may be recommended to help minimize drainage or discomfort. Timely and correct antibiotic treatment is important for treatment to take place. Bacterial or viral infectious conjunctivitis becomes highly contagious during drainage in the eyes.
Conjunctival Tumors and Types
The incidence is 1 in every 2,500 people. Benign tumors are 3 times more common than malignant ones. The reason why corneal and conjunctival tumors are considered together is that such tumors frequently affect both tissues together. Many tumors can also infect the eyelid due to the lid margin neighborhood.
Tumors:
- Cysts: These are clear cysts originating from the conjunctival tissue.
- Papilloma: Multi-segmented tumors that develop due to the human papilloma (wart) virus with or without a stalk.
- Intracellular cell neoplasia of the conjunctiva: Cauliflower, white plaque or gelatin-like intracellular cancer.
- Corneal carcinoma: White plaque-like raised tumors in the limbus where the cornea meets the conjunctiva.
- Nevus (mole) of melanocyte origin, melanocytosis and melanomas: May be dark or light brown in different locations. Increasing darkening of color with age is important.
- Lymphoid hyperplasia and lymphomas
- Epibulbar dermoid or dermolipoma: They are white, raised and dome-shaped in the limbus where the cornea meets the conjunctiva. They are usually in the lower half.
Treatment is usually surgical. To prevent recurrences after surgery, it may be necessary to apply different medications to the area where the tumor was removed during surgery and to use special drops after surgery.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Cornea Transplant?

What is Cornea Transplant?
The cornea is the curved transparent layer of the eye, which is located at the front of the eye, has the task of focusing light and protecting the eye from external factors, plays a major role in visual function, and is the most important refractive lens of the eye. The transparency of the cornea can be impaired by many diseases. These diseases can be congenital, genetic or microbial. In the last stage of keratoconus, if vision is very low and the patient cannot benefit from contact lenses or corneal rings, corneal transplantation is the treatment option.
Some diseases such as keratoconus may require corneal transplantation by changing the shape of the cornea.
About Cornea Transplant
Corneal transplantation is the replacement of diseased tissue with healthy donor tissue in diseases where the shape or transparency of the cornea is impaired. It is medically known as keratoplasty. The most common diseases are keratoconus, corneal edema, microbial ulcers of the cornea or spots (opacities) that develop as a result of accidents and injuries and hereditary corneal spots. In the past, all corneal transplants, regardless of the cause of the disease, involved full-thickness corneal tissue replacement (penetrating keratoplasty). This procedure had complications such as severe infection, rejection of the transplant tissue and inability to see due to irregular astigmatism.
Today, corneal transplants are performed for whichever layer of the cornea is affected by the disease. Transplantation techniques vary according to the condition of the endothelial cell, which is located in the innermost layer of the corneal tissue and keeps the cornea transparent. Corneal transplants in which the anterior layer of the cornea is replaced are called anterior lamellar keratoplasty (DALK) and corneal transplants in which the endothelium is replaced (DSAEK, DMEK). In developed countries such as the USA, more than 50% of corneal transplants are performed with these new methods.
At Dünyagöz, advanced corneal transplants such as DALK, DSAEK or DMEK are routinely performed depending on the patient’s corneal disease. In this way, patients from our country and different countries of the world regain light and vision thanks to these new corneal transplantation techniques. Classical full-thickness corneal transplants are now performed in very few patients and only in mandatory cases.
In keratoconus and corneal stains where the endothelium is intact, the front 85-90% of the cornea is replaced in anterior lamellar keratoplasties called DALK. In such corneal transplants, the possibility of rejection of the donor tissue is greatly reduced or almost eliminated. The life chance (lifespan) of the tissue becomes equal to the patient’s healthy eye.
In eyes with corneal edema or endothelial insufficiency where a previous corneal transplant has been rejected, sutureless endothelial cell transplantation is performed through a small incision called DSAEK or DMEK. In such corneal transplants, patients can return to their normal lives in a few weeks. Patients do not wait for a year for wound healing and suture removal as in conventional transplants. In these eyes, the eye number does not change and astigmatism does not occur after corneal transplantation.
Patient and donor corneas can be cut in planned shapes with Femtosecond laser instead of the blades called trepan. In femtosecond laser cut cornea transplants, less astigmatism occurs and patients can see better.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
About Glaucoma

About Glaucoma
Glaucoma, popularly known as “Eye Pressure” or “Blackwater Disease”, is the damage to the optic nerve due to the frequent increase in intraocular pressure. As a result, the visual field of the person gradually narrows. Glaucoma, an insidious disease that makes itself noticeable in the last stages of the disease, can cause serious damage to the optic nerve that cannot be repaired if diagnosed late.
How Does Glaucoma (Eye Pressure) Occur?
People with higher than normal intraocular pressure have a higher risk of developing glaucoma; however, this does not mean that everyone with high intraocular pressure can have glaucoma. Glaucoma can develop due to many causes. A fluid called aqueous humor is produced inside the vascular layer of the eye. There is a balanced pressure that occurs during the outflow of this fluid out of the eye. This pressure is actually a necessary condition to protect the integrity of the eye. When this fluid does not come out sufficiently, it accumulates in the eye, causing the pressure to increase and damaging the visual nerves.
Who Can Get Glaucoma?
Glaucoma may be related to genetics. People with a family history of glaucoma have a higher risk of developing it. In other words, one or more genes may be defective and these individuals may become more susceptible to the disease.
People over 40 have an increased risk of glaucoma.
Causes of Glaucoma
Patients with diabetes and hypothyroidism (goiter) are at increased risk of developing glaucoma.
Serious eye injuries can cause elevated intraocular pressure. Other risk factors include retinal detachment, eye tumors and eye inflammations such as chronic uveitis or iritis. Some eye surgeries can also trigger the development of secondary glaucoma.
The incidence of glaucoma is about twice as high in myopia, commonly known as nearsightedness.
Long-term use of cortisone (as drops, oral or skin pomade, etc.) can cause secondary glaucoma.
It is important for people with these characteristics to have regular eye examinations for early detection of damage to the optic nerve.
Symptoms of Glaucoma
- Headaches that are more pronounced in the morning
- Occasional blurred vision
- Seeing luminous rings around lights at night
- Pain around the eyes when watching television
What Factors Increase the Risk of Glaucoma?
- Family history of glaucoma (genetic predisposition)
- Being over 40 years of age
- Diabetes
- Severe anemia or shocks
- High-low systemic blood pressure (body pressure)
- High myopia
- High hyperopia
- Migraine
- Long-term cortisone treatment
- Eye injuries
- Racial factors
Since the risk of glaucoma is higher than normal in people with these characteristics, they should have regular eye examinations for early detection of damage to the optic nerve.
Glaucoma Treatment
There are titles in the treatment of glaucoma;
- Medication
- Laser treatment
- Surgical treatment
If eye pressure does not decrease despite medication or laser treatment and the disease continues to progress, the treatment method to be applied will mostly be surgical.
What is the importance of early diagnosis in glaucoma?
Glaucoma is a disease that can be easily treated when diagnosed early. It is especially important for the success of the treatment that individuals with this disease in the family do not neglect their regular check-ups.
What are the rules that the patient must follow in glaucoma treatment?
Eye drops are often used in the treatment process. Since the drops used have the effect of lowering intraocular pressure, they will help keep the disease under control. It is usually started with a drop type. The most important thing here is that the patient uses the given drops at the specified intervals. In order to understand the effect of the drops, after 2 – 3 weeks of use, the patient is called for a follow-up visit for eye pressure measurement. At this stage, the effect of the drug is checked and the treatment is continued with the same drug or different recommended drops. The patient should definitely inform his/her doctor about any other medications he/she is taking.
Glaucoma Auxiliary Diagnosis and Examination Methods
Eye pressure measurement can be done easily and quickly as part of a general examination. During comprehensive eye examinations, eye measurement and eye pressure measurement should be performed. Thanks to these measurements, it can be determined whether a patient is suspected of having glaucoma even if there is no complaint. The basis of glaucoma is the loss of the fiber layer that forms the optic nerve. For this reason, it is necessary for people with signs of the disease to have a Retinal Nerve Fiber examination to detect the damage. In this section, special light and photographic film techniques and computerized support imaging are used. Tests such as corneal thickness measurement and visual field can also be performed to detect eye pressure.
Is Eye Pressure Completely Healed?
Glaucoma is an eye disease that can be kept under control and the progression of the disease can be stopped. However, the person diagnosed with glaucoma should continue lifelong follow-up and treatment.
Frequently Asked Questions
What should eye pressure normally be?
Eye pressure measurement is an essential part of an ophthalmologic examination. The measurement can be used to determine whether you are suspected of having glaucoma. However, glaucoma is a disease that can hide itself. There may be fluctuating pressures during the day or measurements due to corneal thinness may clearly cause the disease to hide itself. Although eye pressure measurements below 20 mmHg are generally considered normal, it is important to remember that there are many types of glaucoma. There are many types of glaucoma such as pigment glaucoma, neovascular, exfoliative and congenital. Therefore, in addition to measuring eye pressure, corneal thickness measurement, optic nerve and retinal examination should be performed.
How Does Eye Pressure Pass?
Glaucoma is a disease that can progress to blindness if left untreated. Its treatment cannot correct the nerve damage in the eye, but it can stop its progression and worsening. The main goal of treatment is to ensure that the patient can see for life.
What happens when eye pressure rises?
Increased intraocular pressure is one of the most risky conditions. As eye pressure rises, the visual field narrows and can cause permanent damage. For this reason, it is very important to analyze the symptoms well and have regular follow-up to protect eye health.
What Should People with Eye Pressure Not Eat?
As in every important disease, excessive consumption of sugary and fatty foods negatively affects eye health. Especially for glaucoma patients, consuming too much fluid at close intervals can increase intraocular pressure.
Does Eye Pressure Occur in One Eye?
Glaucoma is a disease that can be seen in both eyes or one eye at the same time.
How Dangerous Is Eye Pressure?
Glaucoma occurs as a result of the accumulation of intraocular fluid in the eye, which triggers an increase in intraocular pressure. While 9 mmHg is the lower limit for eye pressure, 22 mmHg is considered the upper limit.
Does Eye Pressure Affect Normal Blood Pressure?
Eye pressure and body blood pressure are two different diseases independent of each other. Although this issue is often associated among the public, a person with eye pressure may not have eye pressure, and a person with body blood pressure may not have eye pressure. However, since normal blood pressure is a disease that can affect every organ in general, high or low blood pressure can adversely affect the eyes. Therefore, glaucoma patients are expected to pay extra attention to their body blood pressure.
Does Eye Pressure Cause Headache?
Severe headaches are among the most prominent complaints in high eye pressure. However, it is not correct to associate every headache with glaucoma. For this reason, the underlying cause should be investigated in long-term headache complaints.
Does Glaucoma Cause Pain in the Eye?
In glaucoma, complaints and symptoms usually begin to appear in advanced stages. Symptoms may vary according to the type of glaucoma. However, eye pain may occur due to glaucoma. It is recommended to be examined by an ophthalmologist in case of persistent eye pain. Eye pressure measurements and fundus examinations should be performed during regular eye examinations.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Glaucoma Types
What is Open Angle Glaucoma?
It is the most common type of glaucoma. It occurs at an advanced age (50-60 years). As the function of the drainage angle decreases over the years and the intraocular fluid cannot drain sufficiently, the intraocular pressure (eye pressure) rises and causes damage to the optic nerve. Eye pressure is usually between 12 and 20 mm Hg in normal individuals. In glaucoma patients, this value is usually above 20 mm Hg. However, some people with sensitive optic nerve structure may experience damage to the optic nerve even at normal eye pressure values.
People with high eye pressure who have not yet developed glaucoma damage are considered ocular hypertensive. Patients with optic nerve damage due to glaucoma must be treated. Unfortunately, glaucoma is asymptomatic. Since central vision is not affected in the early stages, patients may not notice vision loss. For this reason, it is important to undergo an eye screening at the age of 40 and to have an eye examination once a year after the fifties.
Depending on the level of damage to the optic nerve, localized visual field loss initially develops. As the disease progresses, these areas merge to form large visual field losses. When the optic nerve is completely damaged, blindness develops.
What is Narrow Angle Glaucoma?
It is a less common type of glaucoma. It usually occurs in hyperopic eyes with a smaller structure, when the iris tissue (the colored part of the eye) is located very close to the drainage angle and closes this angle.
Since the outflow of intraocular fluid is blocked by the closure of the drainage angle, eye pressure suddenly rises to 40 – 50 mmHg. This condition is quite painful. It may be accompanied by nausea and vomiting and blurred vision. This condition, which needs to be treated urgently, can cause permanent blindness. In some patients with narrow-angle glaucoma, angle closure may develop gradually over years.
Glaucoma Diagnosis
Anyone can get glaucoma and early diagnosis is the only way to prevent vision loss due to the disease. Unless there is significant damage to the visual field due to glaucoma, the patient does not realize these losses. For this reason, it is important to have regular eye examinations and tests performed annually. Approximately 2.5 out of 100 people over the age of 40 are at risk of glaucoma, and the risk of glaucoma in the population increases with increasing age. Glaucoma can be diagnosed early with a careful eye examination. For this reason, annual eye examinations are very important.
How is Glaucoma Diagnosed?
- Intraocular pressure (IOP) measurement: IOP can be measured using different methods. These are air measurement, measurement by applanation method and measurements with devices such as Tonopen and Icare. In the normal population, IOP is 98% 22mmHg and below. The pressure difference between the two eyes is mostly below 4mmHg. IOP measurement alone does not indicate whether a person has glaucoma or not.
- Corneal thickness (pachymetry) measurement: It helps the physician to decide whether or not to start medication in some patients. The average corneal thickness in the normal population is around 530 microns. In patients with a high corneal thickness, the eye pressure measurement may be above the normal value as a false elevation or in patients with a corneal thickness of less than 500 microns, the eye pressure may be underestimated.
- Gonioscopy: Examining the anterior chamber angle, which is the area where the eye water drains into the capillaries and where the reticular structure that is the “sink of the eye” is located, is an important part of the glaucoma examination. Changes such as accumulations, adhesions, narrowing, tears, new vessel formations will guide our diagnosis and treatment.
- Computerized visual field measurement: It is important in the diagnosis and follow-up of glaucoma. Here, losses that occur in the visual field due to nerve cells affected by glaucoma, which the person is not aware of, are detected. Depending on the stage of the disease, certain parts of the visual field can be examined in more detail. In addition, tests performed at certain intervals can be analyzed to determine whether there has been progress in successive visual field tests over the years. In recent years, visual field test results can be combined with tests such as optical coherence tomography (OCT) to perform structure-function analysis. This enables a more accurate and precise diagnosis and follow-up of the disease.
- Optic nerve head, nerve fiber layer and macular region analysis: We can detect glaucoma-related changes in the optic nerve head, retinal nerve fiber layer and macular region very precisely with OCT. Using the different features of this method, we can diagnose glaucoma at a very early stage even before any loss of visual field occurs and there is no complaint in the patient, and we can also determine whether there is progression in the disease in diagnosed cases very precisely and re-plan our treatment accordingly. Using the angiography feature of the same method, we can examine the capillary density in areas that may be affected by glaucoma.
- Anterior segment imaging methods: Detection of changes in the formations in the anterior part of the eye, which we call the anterior segment, is of great importance in the diagnosis and follow-up of glaucoma cases. We can obtain important parameters such as anterior chamber angle, iris slope, anterior chamber depth with anterior segment OCT test. Ultrasound biomicroscopy (UBM) can also be used to examine the formations further back that we cannot evaluate with OCT.
- Other tests:In addition to the above routine methods, tests such as orbital B Mod ultrasonography, angiography, electrophysiological tests, microperimetry and examination under general anesthesia (especially infant patients) can be performed when needed in the diagnosis and follow-up of glaucoma patients.
How is Glaucoma Treated?
There are mainly three ways to treat glaucoma.
Medication Therapy
First, the patient’s eye pressure is lowered either by reducing the production of fluid in the eye or by increasing its outflow. There are medications used for these two methods. These medications are drops that are taken at regular intervals every day and are used for life. Since each patient responds differently to these drops and they may have side effects, your doctor will choose the appropriate medication for you and observe the results. It is also very important that patients who are taking medication are followed up at intervals that their doctor deems appropriate, because over time, the response to the medication may decrease. In this case, it may be necessary to change the medication, add other medication or resort to additional methods such as laser treatment and surgical treatment.
Laser Treatment
In the treatment of glaucoma, the laser beam is first used to treat an acute glaucoma attack and to prevent the other eye from going into a glaucoma attack. Secondly, in chronic glaucoma cases, the laser is applied to the outflow channels like a strainer to facilitate the outflow of the fluid made in the eye. These two laser treatment methods are outpatient treatments without the need for an operating room. Another use of laser in the treatment of eye pressure is the application of laser to the white area around the colored part of the outer part of the eye. The aim is to reduce the production of eye water by destroying the area on the inner side of this part that secretes eye water. This treatment method is performed in the operating room, usually under local anesthesia, and the patient can go home the same day.
Surgical Treatment
If the patient’s eye pressure does not decrease despite medication or laser treatment and the disease continues to progress, surgery is often the treatment of choice. Depending on the stage of glaucoma and the condition of the eye, the doctor will apply one of many different surgical techniques to the patient.
What is Trabeculectomy?
Surgeries that aim to drain the eye water into the vessels outside the eye are the most common surgeries. The first of these, also called trabeculectomy surgery, is an operation in which new thin channels are created in the eye wall in order to filter the fluid that cannot drain sufficiently from the eye to the vessels outside the eyeball. This surgical method, which is usually performed under local anesthesia and sometimes under general anesthesia, has been the most commonly used surgical method for many years and its results and complications are well known. Its effectiveness is also quite high. Although it is perceived as a single type of surgery, the surgeon can make modifications in this surgical method according to the condition of the eye in question. It is also possible to perform this surgery together with cataract surgery. There are also some current implants that aim to drain the eye water in this way. The above-mentioned canals are replaced by very thin tubes made of different materials, the end of which is inserted into the eye.
What is Minimally Invasive Glaucoma Surgery?
In some new methods, also called minimally invasive surgical methods, there are various methods, with or without implants, in which the water in the eye is directed to the eye’s own drainage canals system. With these methods, the recovery of the eye can be shorter, but their effectiveness is not always as good as with trabeculectomy surgery. In appropriate cases, very satisfactory results are obtained. Here too, your doctor will inform you about the advantages and disadvantages of the method to be applied at the preoperative decision stage. Another common application of these methods is in combination with cataract surgery.
What is Tube Implantation?
In the method called seton or tube surgery, eye pressure is controlled with implants that have a thin silicone tube part placed inside the eye and a reservoir part placed between the layers outside the eyeball, allowing the eye water to drain into the capillaries outside the eye. These implants are made of material compatible with the eye and have a compatible design, meaning they are permanent in the eye.
What are Cyclodestructive Procedures?
Another way of glaucoma surgery is to reduce the production of eye water. This used to be done by cryodestruction, also known as freezing. Recently, it is performed using a diode laser. Here, the laser is applied to the white area around the colored part of the outer part of the eye. The aim is to reduce the production of eye water by destroying the area on the inside of this part that secretes eye water. This treatment method is performed in the operating room, usually under local anesthesia, and the patient can go home on the same day.
Do Babies Get Glaucoma?
Rarely, glaucoma can also be seen in infants and the treatment is surgery without delay. Some surgeries different from adult glaucoma are applied here. In cases where there is no response, one or more of the methods mentioned above can be applied.
What are Other Methods?
In rare types of glaucoma where the anatomy of the eye is different, the above-mentioned surgeries may be combined with additional interventions. Sometimes surgeries such as vitrectomy and keratoplasty can also be combined with glaucoma surgery.
Glaucoma laser treatments and surgeries performed at Dünyagöz Hospitals are listed below:
- Laser trabeculoplasty
- Laser iridotomy
- Laser iridoplasty
- Infant glaucoma examination/follow-up under general anesthesia
- Ab-interno surgery for infant glaucoma
- Ab-exsterno surgery for infant glaucoma
- Trabectome surgery
- Gonioscopy-assisted transluminal trabeculotomy
- Canaloplasty
- Xen implant surgery
- Deep sclerectomy
- Viscocanalostomy
- Trabeculectomy
- Kahook Double-blade surgery
- Tube implantation (Ahmed Valve surgery)
- Cyclocryodestruction
- Diode laser cyclodestruction
- Bleb revision
- Concomitant surgeries of cataract and glaucoma
- Various combined operations in complicated cases
People who have undergone glaucoma surgery should continue regular glaucoma follow-up.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Ocular Oncology?

What is Ocular Oncology?
The sub-discipline dealing with all kinds of diagnosis and treatment of eye tumors is called ‘Ocular Oncology’. Ocular oncology, i.e. eye tumor science, is a department that requires two years of additional training after ophthalmology residency. Ocular Oncology, which has developed as a subspecialty of Ophthalmology all over the world, is a special subspecialty that requires close cooperation and multidisciplinary teamwork with various medical sciences such as radiation oncology, pathology, radiology, medical oncology and genetics, as well as with all other areas of the eye. Ocular oncologic evaluation is, therefore, an area in which ophthalmology is most intertwined with systemic medicine.
The most advanced gold standard technologies are used in the treatment of intraocular tumors and orbital diseases. The center is managed under the leadership of a specialist physician, and the treatments are performed comfortably for both the patient and the physician with the advanced technological machine park and experienced medical team.
Radioactive Plaque Treatment
If the size of the tumor in the eye is appropriate, if it is located in a certain place, if it is less than 1 cm thick and its base is less than a certain size, radioactive gold plate treatment is recommended directly to the eye wall.
The isotopes that can be used in the radioactive plate to be placed in the eye are cobalt 60, Iodine 125 and Ruthenium 106. The most ideal for the eye is Iodine-125. For this reason, Iodine-125 isotope plates are used during surgery. The radiotherapy dose to be applied according to the tumor dimensions transferred to the computer environment before the operation is calculated by the brachytherapy physicist and the plate is ordered accordingly.
During the surgery, the location of the tumor is determined and the radioactive plaque is sutured to the sclera over the tumor site. In addition to the plaque treatment, thermotherapy or cryotherapy may be required during or after surgery. The radioactive plaque is adjusted according to the dose to be administered and removed from the eye with surgery again after an average of 4-7 days.Postoperatively, patients are checked at regular intervals (usually postoperative day 1, week 1, month 1; 3 months, 6 months…).Immediately after surgery, a temporary increase in tumor size and an increase in retinal detachment may be seen.Mostly, tumor shrinkage is seen 3-6 months after the plaque is placed.
Other complications that may occur due to treatment are anesthesia-related problems during surgery, infection, cataract formation, radiation-induced retinal and optic nerve damage, central retinal artery occlusion, bleeding into the eye, elevated eye pressure (glaucoma), melting of the eye wall (sclera), double vision, strabismus, corneal inflammation (keratitis, dry eye and intraocular reaction (uveitis), decreased vision and vision loss.
WHAT IS UVEAL MELANOMA?
Uveal melanoma is the most common primary malignant (intraocular) tumor of the eye in adults.
WHAT ARE THE SYMPTOMS OF UVEAL MELANOMA?
Choroidal melanoma gives symptoms such as flashes of light, flies, broken and crooked vision, decreased vision, loss of visual field (scotoma) in the early stage, inflammation, pain, redness, glaucoma in the late stage. In tumors involving the iris, the colored layer of the eye, there are findings such as changes in eye color, changes in the shape of the pupil, and spontaneous bleeding in the eye.
HOW IS UVEAL MELANOMA DIAGNOSED?
Uveal melanoma is diagnosed by clinical eye examination and radiological examinations such as ultrasonography, fundus angiography, computed tomography and magnetic resonance imaging. In addition to these, chest X-rays, liver function tests and abdominal ultrasonography are performed to examine metastases.
WHAT ARE THE TREATMENTS FOR UVEAL MELANOMA?
Laser treatment, freezing treatment (cryotherapy), heat treatment (thermotherapy) or surgical removal can be applied in small-sized tumors. Radioactive plaque and Helium or Proton radiation therapy, which is not available in our country, can be applied in medium-sized tumors and eyes that have a chance of seeing. There are not yet sufficient number and long-term results on Cyberknife treatment.
WHAT IS RADIOACTIVE PLAQUE THERAPY IN UVEAL MELANOMA?
Uveal melanoma is diagnosed by clinical eye examination and radiological examinations such as ultrasonography, fundus angiography, computed tomography and magnetic resonance imaging. In addition to these, chest X-rays, liver function tests and abdominal ultrasonography are performed to examine metastases. There are various options for the treatment of uveal melanoma. For tumors less than 12 mm in height and less than 18 mm in base diameter, radioactive plaque is the gold standard treatment worldwide.
In larger tumors, proton beam therapy may be used, which is not available in our country. Adequate and long-term results on Cyberknife treatment are not yet available.
WHAT IS RETINOBLASTOMA?
Retinoblastoma is the most common malignant intraocular tumor of childhood. Retinoblastoma occurs in approximately one in 20,000 live births. It is most common between the ages of 1-3 years and spreads outside the eye when left untreated. It causes death especially by metastasizing to the brain and bone marrow. Retinoblastoma is the only malignant tumor that has been shown to be inherited (genetically inherited). Retinoblastoma is unilateral (in one eye) or bilateral (in both eyes). In most cases (two thirds) it is unilateral. When unilateral, there is usually one tumor. When it is bilateral, there may be tumors in more than one focus, increasing the risk of other tumors developing in the brain or throughout the body.
WHAT ARE THE SYMPTOMS OF RETINOBLASTOMA?
Retinoblastoma initially causes no symptoms. It is rarely diagnosed during a routine eye examination. In 75% of children under 3 years of age, leukocoria (white flash in the pupil) and strabismus are typical for retinoblastoma.
When retinoblastoma is suspected, a fundus examination should be performed. Children should be examined under general anesthesia to avoid missing tumors.
RETINOBLASTOMA TREATMENT
Appropriate staging of the tumors, determination of the initial treatment choice, and realistic evaluation of treatment outcomes are necessary.
The main treatment modality for retinoblastoma is chemotherapy.
The aim is to shrink the tumor or tumors with chemotherapy (chemoreduction) and, in the meantime, to completely destroy the tumors with local treatments [cryotherapy (tumor freezing treatment), thermotherapy (laser treatment that kills the tumor by heating it) and radioactive plaque (local radiation treatment with plaque)]. In addition to these treatments, external beam radiotherapy, enucleation and exenteration can be performed. The ideal method in the treatment of retinoblastoma should destroy the tumor quickly, protect the eye and vision, not be life-threatening, leave no damage to the eye and provide aesthetics.
According to these ideals, a combination of chemotherapy and local therapies has been used to avoid enucleation (removal of the eye) and radiotherapy. For this purpose, in some patients with retinoblastoma, a radioactive plate can be used to prevent enucleation in eyes with unifocal retinoblastoma that has recurred despite all kinds of chemotherapy and local treatments.
RADIOACTIVE PLAQUE TREATMENT IN RETINOBLASTOMA
The guidelines for the insertion and removal of the radioactive plaque and the complications that may occur during treatment are as described in the discussion of uveal melanoma. Unlike uveal melanoma, if an eye perforation occurs during surgery while passing the sutures, the risk of the tumor spreading outside the eye and posing a risk to life is very rare in eyes with retinoblastoma. The radiation dose for retinoblastoma is lower than for uveal melanoma. The aim here is to save the patient’s life and eye, and to preserve vision as much as possible. Although it varies according to the literature, in more than half of the cases, the eye can be preserved by destroying the tumor. In about half of the cases, the eye may need to be removed despite all efforts.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Oculoplasty?

What is Oculoplasty?
Oculoplasty and orbital surgery is a specialty that deals with diseases of the eyelids, tear ducts and orbit.
From the removal of eye bags to prosthetic eye construction, from intraocular tumor surgeries to Botox, the treatment of all eye contour diseases such as almond eye, chalazion, plexr and thyroid eye disease and aesthetic surgery applications are performed with oculoplasty and orbital surgery.
The eyelid is a much more sensitive area than other tissues in the body. Eyelid skin is the thinnest skin area of the body. In all surgical interventions in oculoplasty and orbital surgery, it is very important not to damage intact tissues and to intervene only where necessary. It is important that the surgery is performed by ophthalmologists who are trained in oculoplasty surgery and who know the anatomy of the eyelid and the principles of aesthetic surgery.
Eyelid Surgery
Eyelid surgery (blepharoplasty) is the process of removing excess fat, muscle and skin tissue in the upper and lower eyelids and tightening the parts around the eyes that support these tissues. With this surgical procedure, sagging, inverted or everted upper and lower eyelids, bagging due to excess fat accumulation and wrinkles around the eyes are corrected.
WHAT IS DROOPY EYELID?
A droopy eyelid, a droopy upper eyelid is called “ptosis”. It is an eye problem that is congenital due to various reasons or develops later, and is seen as a low eyelid that covers the colored part of the eye for more than one millimeter in length. Patients with droopy eyelids must be treated not only aesthetically but also because it can cause problems such as narrowing of the visual field. In children, droopy eyelids can cause lazy eye. If lazy eye occurs, it must be operated until the age of 6.
Although the disease can be seen in people of all ages, it can be congenital (congenital ptosis) or acquired.
Congenital disorders of the upper eyelid
The most common congenital defect of the upper eyelid is droopy eyelid (ptosis). There may also be eyelid disorders such as eyelid adhesion (ankyloblepharon), inward (entropion) or outward turning (ectropion) of the lid margin, incomplete formation of the eyelid (coloboma), extra row of eyelashes (dystichiasis).
WHAT ARE THE SYMPTOMS OF DROOPY EYELID?
A droopy eyelid can often be caused by hereditary problems or muscle disorders.
Symptoms of patients with droopy eyelids can be as follows
- Trying to pull the eyelids up by raising the eyebrows
- A tired and dull expression on the face
- Dryness or excessive tearing in the eye
- Narrowing of the visual field
WHAT ARE THE TREATMENTS FOR DROOPY EYELID?
Treatment of ptosis is surgically possible. Since this problem is seen at all ages, treatment methods may vary according to age groups. Generally, in pediatric patients, surgery is performed in order not to affect vision and prevent lazy eye, and then the use of special glasses with closure treatment may be recommended and intervened with eye drops. If the patient is an adult, the excess tissue in the eyelid, which is visible from the outside and may even reduce the level of vision, can be removed or the muscle holding the eyelid can be intervened to strengthen the muscle.
When surgical intervention is required for droopy eyelids, treatment is performed by our oculoplasty physicians who are experts in their field. The treatment takes about 20 minutes and is usually performed under local anesthesia.
What are Congenital Disorders of the Upper Eyelid?
The most common congenital defect of the upper eyelid is droopy eyelid (ptosis). Apart from this, there may be eyelid disorders such as eyelid adhesion (ankyloblepharon), inward (entropion) or outward rotation (ectropion) of the lid margin, incomplete formation of the eyelid (coloboma), extra row of eyelashes (dystichiasis).
What are Age-Related Eyelid Changes?
With aging, eyebrows and eyelids fall, the lower eyelid turns inward or outward, bags or depressions around the eyes and wrinkles occur. These complaints can also be seen familial in younger people. Changes around the lids give the person an unhappy, tired and sleepy appearance. The type of treatment is determined according to the type of problem.
What is Ingrown Eyelashes (Trichiasis, Dystidiasis)?
Ingrown eyelashes occur congenitally (dystichiasis) or after some eyelid diseases, as a result of the lid edge (entropion) or only the eyelashes (trichiasis) turning inward. They touch and damage the transparent layer of the eye called the cornea and the treatment is surgical.
What is the Treatment of Congenital Eyelid Disorders?
The most common congenital defect of the eyelid is droopy eyelid (ptosis). Apart from this, there may be eyelid disorders such as eyelid adhesion (ankyloblepharon), inward (entropion) or outward rotation (ectropion) of the eyelid margin, incomplete formation of the eyelid (coloboma), extra row of eyelashes (dystichiasis). Treatment of these diseases is surgical.
What is inverted eyelid (entropion)?
Entropion, which usually occurs in the lower eyelid, occurs when the eyelid turns inward. Inverted eyelid margin may be congenital or may develop later. Surgical treatment is applied.
What is Eyelid Outward Rotation? (Ectropion)
Outward rotation of the eyelid margin usually occurs as a result of aging. It can also develop after congenital paralysis of the nerve that closes the eyelid (facial paralysis) and injuries. Surgical treatment is applied.
Is it possible to treat facial paralysis (facial paralysis)?
Facial paralysis occurs when the nerve that provides the movement of the eyebrows, eyelids and face stops working for any reason. In case of temporary paralysis, medical treatment is applied to protect the eye. In permanent paralysis, different surgical treatments are applied.
How Are Under Eye Bags Treated?
The most important reason for the formation of under-eye bags is genetics, that is, heredity. The second reason is thyroid disease. Under-eye bags give the person an older and tired appearance. It is treated by removing excess fat tissues or changing their location.
Operations can be performed under local anesthesia and the effects last for a long time. Interventions on the lower eyelid can usually be performed through the lid without the need to cut the skin. Thus, the problem of scarring or deformity of the lid after the operation is avoided.
What is Brow Lift Operation?
Patients may have low eyebrows as well as excessive eyelid. Generally, due to age or genetics, the outer sides of the eyebrows may fall downward due to gravity. This fall creates excess skin on the lid by placing a load on the lid and disrupts the aesthetic appearance.
In direct browpexy, an incision is made just above the eyebrows parallel to the eyebrow hairs and the eyebrow is lifted upwards. This incision can be made with a scalpel or carbon dioxide laser. The incision scar can be seen for 3-6 months, even if it is hidden. It is rarely applied.
In internal browpexy, an incision is made from the lid line as in the technique we call blepharoplasty. It is especially effective in the lower 1/3 of the outer part of the eyebrow. It is a method that does not leave a scar on the eyebrow.
WHAT IS BLEPHARITIS?
There is a gland mouth at the base of each eyelash. These glands make secretions and nourish and irrigate the transparent layer (cornea), the front layer of our eye. This helps us to see clearly.
These gland openings are narrow in some people. These glands, which we call meibomian glands, get infected due to stenosis. It causes dandruff at the base of the eyelashes, loss of eyelashes and frequent inflammation and even cysts on the eyelid and forms CHALAZION.
Blepharitis is a chronic disease. The patient goes from doctor to doctor and looks for a cure. Each doctor gives a different antibiotic drop or cream, the patient thinks that he will be cured. However, the real treatment is WARM DRESSING and CLEANING THE EYELASH BOTTOM EVERY MORNING. Some patients do eyelash cleaning at night due to lack of time in the morning. The important thing is to clean the base of the eyelashes every day.
Blepharitis is very common in seborrheic patients and patients with rosacea.
TREATMENT
Eye Relax device. The patient buys this device and applies it at home. Every morning or evening, the eyelids are heated and massaged for 5-10 minutes and the meibomian glands are drained. Thus, blepharitis is relieved.
IPL (intense pulsed light) treatment. The patient is treated with this device in the hospital. The patient enters this device at intervals to be determined by the physician (1 time a week for 1 month or 3 months). With this device, the disease is treated by applying certain doses of energy to the meibomian gland and eyelids. It is a technique also used in dry eye.
Hot dressing every day. Wash your eyelids frequently every day with hot water from your tap. Hot treatments such as showers, saunas and spas relieve blepharitis very well. The more often you wash during the day, the more comfortable you will be. This application can even be 20-30 times. You can also do this with hot water soaked in cotton or cloth.
Massage. After the hot application, empty the cloth by pressing on the bottom of the lower lid eyelashes. Since the narrow gland mouths are opened with hot water, the gland ends will be emptied immediately with massage.
Shampoo Apply the given shampoo to the base of the eyelashes at night and go to bed without rinsing. Before this procedure, you must wash your eyelids with warm (as much as you can stand) water that softens the eyelash base glands.
Cleaning with medicated wipes. Since there is dandruff and flaking at the base of the eyelashes, it is necessary to clean the base of the eyelashes every morning after dressing and massage with hot water. Since S.aureus germs and demodex parasites settle at the base of the eyelashes, cleaning with medicated wipes will quickly cure blepharitis. Medicated wipes are much more effective than eye shampoos and are even more effective when used together.
Antibiotic drops. If your doctor deems it necessary, he or she will prescribe drops to eliminate germs and parasites. Use these drops as prescribed by the doctor. This is usually for 7 days. Then stop taking the medicine. Continue with warm dressing, massage and cleaning with medicated wipes.
Remember that blepharitis is a chronic disease. So it can continue. Therefore, apply the above-mentioned procedures for 3 months. When it recurs, follow the same procedures again. This is the remedy.
Use of glasses. If you need glasses and do not wear glasses, blepharitis recurs very often and cannot be treated. In this case, it is good to wear glasses or, if your eyes are suitable, to remove the numbers with excimer laser.
Stress. Blepharitis and chalazion are more common in stressed people.
How should women use pencils and mascara? Blepharitis and chalazion are common in female patients who use pencils because the base of the eyelashes are covered by the pencil. If you have blepharitis or chalazion, we recommend that you completely remove the pencil from your life. As for mascara, it should be applied only on the tip of the eyelashes, not on the base of the eyelashes.
In short: Apply shampoo before going to bed at night and clean with a medicated wipe in the morning
SHALAZYON
Poorly treated blepharitis and stye (hordeolum) can develop into chalazion. If a chalazion has formed, there is NO OTHER REMEDY but SURGERY. Since the surgery is performed through the lid, no stitches are used and there is no scar. If chalazion surgery is delayed, it may infect other valves and require surgery on all valves. If chalazion has developed, undergo surgery before the end of 1 month. If you do the things described in the treatment section above after chalazion surgery, you will prevent the chalazion from recurring.
What is Almond Eye Aesthetics?
In almond eye aesthetic operations, it is aimed to lift the eyes slightly. These operations, which have started to be performed quite frequently recently and make many women happy, provide a more aesthetic appearance of the face and eye area. Thanks to the almond eye surgery, a completely new and aesthetic appearance is achieved thanks to the almond eye surgery of the eye edges, where women deal with make-up the most and deformations occur over time.
How is Almond Eye Aesthetic Surgery Performed?
Almond eye aesthetic operations are performed by applying local and general anesthesia. Thanks to the anesthesia applied before the operation, there is no feeling of pain during the procedure. The operation is completed in approximately 1 or 1 and a half hours. It can also be performed in combination with operations such as upper and lower eyelid aesthetics and brow lift aesthetics. There is usually no pain after the operation, but bruising or swelling may occur. The average duration of these swellings is 5 to 7 days.
Tear Duct Surgery
The lacrimal ducts begin with two small holes on the inside of the upper and lower eyelids, form the lacrimal sac and end in a thin duct that opens into the nasal cavity. The purpose of tears is to protect the eye from foreign bodies, to provide the lubrication and clarity necessary for eye health and to nourish the eye. The front of the eye is constantly washed with tears. With this washing, harmful substances in the front of the eye are transferred through the tear duct to the nose and then to the throat. Blockages in this pathway cause watering and burring. At first, the patient experiences watery eyes in cold weather, but later the watering becomes permanent. Tear duct surgery is a surgical unit that deals with diseases that occur in this region.
What is Dry Eye?
Dry eye gives symptoms that vary according to the severity of tear deficiency. These can range from minor complaints such as mild burning, watering and redness that occur from time to time to severe enough to seriously impair vision and quality of life. In mild cases, artificial tear drops are used according to the principle of replacing the deficiency. Severe dry eye requires different and serious treatments.
What are the Types of Tear Duct Blockage?
Subsequent Tear Duct Obstructions
The cause of a blocked tear duct is usually an infection of the narrow tear duct. The location of the blockage is the holes in the eyelids or the junction of the tear sac and the duct. It is more common in women. Surgical treatment is applied.
Congenital Tear Duct Obstructions
The tear ducts continue to develop after birth. In some babies, when the development of the duct is not completed after birth, it may be seen with symptoms such as watery eyes and burrs. Different treatments may be required depending on the patient’s condition.
What are Tear Duct Obstruction Treatments?
Probing Treatment (Probing)
Tear duct blockages cause watering and inflammation. If the tear duct is blocked, the tear sac area is massaged as directed by the physician until the age of 1. Until the age of 1, if it is not opened with massage, probing is performed under operating room conditions. In some children, burring and watering are very excessive. In these children, probing is performed around 6 months without waiting for 1 year of age. The procedure is performed under general anesthesia and takes about 5-10 minutes. The upper end of the tear duct is entered with the help of a probe and the obstruction at the lower end of the duct is opened. The chance of success is around 90-95%. Over 2 years of age, the chance of success decreases.
Surgical Intervention (Silicone tube intubation)
It is applied seamlessly in children or adults if the tear duct is narrow, if the punctum is narrow or absent, if there is obstruction in the small channels in the soft tissue we call canaliculi. After 6 months in the eye, the silicone tube is removed.
Surgical Intervention (DSR)
In adults, opening the blocked duct can be done by creating a new pathway between the lacrimal sac and the nose. The surgery can be performed through the skin or through the nose. In the surgery performed through the skin, there is usually no disturbing scar on the skin. Sometimes, if the canal is narrow in DSR surgery, a silicone tube can be applied additionally.
Multidiode Laser (Treatment of Tear Duct Obstruction with Laser)
It is one of the newest and most comfortable techniques for opening tear duct obstructions. With the new generation “Multidiode Laser”, which has been used in the USA and various European countries for the last 10 years, tear duct surgeries can be treated without incisions on the skin, without leaving scars and with regional anesthesia. In order to perform tear duct surgery with laser, there must be no obstruction in the canaliculi, which we call soft tissue, and the tissue must be intact.
Tear System Tumors
Tumors of the lacrimal gland are more common than tumors of the excretory system. They are more common in adults. Treatment varies according to the type of tumor.
Tear Pathway Injuries
It is usually associated with eyelid injuries. If not treated within 1 week, it may cause permanent blockage of the tear ducts, constant watering and burring. It should be seen by an ophthalmologist and the disorder caused by the trauma in the tear ducts should be corrected.
Prosthetic Eye
The prosthetic eye applied to people who have had their eyes removed can be produced individually in different colors and sizes.
Prosthetic eye is an aesthetic solution preferred in cases of irreversible loss of vision and serious aesthetic losses caused by serious traumatic injuries such as traffic accidents and foreign objects in the eye. Prosthetic eye can be applied at any age. It can be applied with the physician’s decision 3 – 4 weeks after the patient’s eye is removed.
The prostheses are completely customized and are applied without burning, stinging or redness in the eye.
The eye prosthesis is made of acrylic, a light material. This material is compatible with the human body and is unbreakable. Placing a ball (implant) after enucleation or evisceration surgery is a procedure that increases the movement of the prosthesis.
With the prosthetic eye;
- Sports
- Bath
- Sleepable
- Swimmable
Pterygium (Flesh Growth in the Eye)
Pterygium, popularly known as “angel wing”, is a common eye problem. It is quite common in the climate zone in which our country is located. It is a wedge-shaped, pink-colored, non-cancerous lesion that extends over the cornea tissue covering the colored part of the eye, mostly in the conjunctiva on the nasal side. Also called “surfer’s eye” abroad, it is a problem that we encounter more frequently in people who spend a lot of time outdoors, who are exposed to the sun’s rays and hot and dry air flow, especially those who work or play sports outdoors for a long time without protection, that is, without sunglasses or hats. Symptoms include burning, itching, discomfort, foreign body sensation and blurred vision.
Eye and Eyelid Tumors
Ocular oncology is the branch of science that deals with tumors in the eye and tissues around the eye.
Eyelid Tumors
Approximately ¾ of the tumors seen in and around the eyelid are benign tumors. When there is a wound on the eyelid that does not heal, it is absolutely necessary to be examined by an ophthalmologist to determine whether it is a malignant tumor. Surgical treatment should be applied.
Tear System Tumors
Tumors of the lacrimal gland are more common than tumors of the excretory system. They are more common in adults. Although the treatment depends on the type of tumor, surgical intervention, chemotherapy and radiotherapy are the methods used in treatment.
Intraocular Tumors (Melanoma)
Uveal melanoma is the most common intraocular tumor in adults. It is not life-threatening as long as it remains inside the eye. Large tumors require surgical treatment and removal of the eye (enucleation). For smaller tumors, radiotherapy, plate radiotherapy (brachytherapy), transpupillary thermotherapy (TTT) can be applied.
Intraocular Tumors (Retinoblastoma)
Retinoblastoma is the most common childhood intraocular tumor. Surgery, radiotherapy and laser applications are the techniques used today.
Capillary Hemangioma
They are benign lesions consisting of a ball of capillaries that are congenital or appear in the first months after birth, especially on the eyelids, but also around and behind the eyes. Treatment is necessary for lesions that affect vision.
Cavernous Hemangioma
It is the most common benign orbital tumor in adults. They need to be surgically removed.
Lymphangioma
Although it is a benign vascular lesion, it is difficult to treat completely because it spreads between the tissues in the orbit and gradually grows. Treatment depends on the case.
Lymphoma
It is one of the most common tumors of the orbit and its incidence is increasing. Radiation therapy (radiotherapy) and chemotherapy are applied depending on the condition.
Meningioma
It is a benign neurogenic tumor of the orbit. Treatment depends on the case.
Optic Glioma
It is a tumor of the optic nerve and visual pathways. Treatment can be done with radiotherapy or surgery depending on the condition of the eye.
Rhabdomyosarcoma
It is the most common malignant orbital tumor in children. Surgical treatment, radiotherapy and drug treatment (chemotherapy) are applied together.
Orbital Surgery
Thyroid Related Eye Diseases (Graves’ Disease)
In some diseases of the thyroid gland, which plays an important role in the regulation of metabolism, there are some disorders and deformities in the eye. This condition is more common in cases where the thyroid gland is overactive (hyperthyroidism). Findings such as protrusion of the eyes forward (exophthalmos, proptosis), excessive opening of the lids, strabismus, double vision, decreased vision are observed. This disease, also known as “thyroid orbitopathy” or “Graves’ orbitopathy”, may be mild or severe enough to lead to vision loss. Treatment is determined according to the period, severity and whether the disease is active or not.
Orbital Inflammation
There are infections caused by microbial agents and non-microbial, immune-related inflammation of the orbit. Microbial infections often develop in children and following sinus infections, but can occur at any age due to many factors, especially after trauma. If not treated early and appropriately, it can become vision and life-threatening. Depending on the condition, medication or surgical treatment is performed. Radiotherapy may be necessary if there is no response to cortisone.
Orbital Tumors
Approximately 20% of all orbital diseases are benign or malignant tumors. The tumor may threaten life by spreading to the tissues around the eye and other organs, especially the brain. Therefore, early diagnosis and treatment of diseases is important.
Orbital Injury
Due to its proximity to vital organs, orbital injuries can be life-threatening. Therefore, the patient is first evaluated in terms of brain function and respiratory tract. The rate of eye involvement is also high in orbital injuries. In this respect, the condition of the eye should be evaluated first. Surgical treatment is applied.
Congenital small or absent eye
Since the size and presence of the eye ensures the development of the tissues around the eye, when the eye is underdeveloped, the eyelids, soft tissues around the eye and the bony framework do not reach sufficient size. In mild and moderate cases, increasingly larger molds (conformers) are used, while in more severe cases, surgical intervention is required.
What is an Oriental Fracture?
All of the bone, muscle, fat, nerve and vascular structures surrounding the eye are called orbit. Bone fractures around the eye are called orbital fractures. The orbital region is the most sensitive and delicate part of our face. For this reason, traumas in the orbital region should be detected and treated early. It is possible to encounter orbital fractures frequently in case of impact or contact with a hard object. It is very important to treat orbital fractures, especially in children, with emergency intervention. Orbital fractures may be asymptomatic and require careful examination. The risks of causing double vision problems or changes in the position of the eyeball should be examined in detail.
What are the Types of Orbital Fractures?
Orbital rim fracture;
Since the bony outer edges of the eye socket are very thick, an injury in this area must have experienced too much pressure for a fracture to occur. The orbital bones in the orbital region, i.e. the bones of the roof and side walls, are intact. There are two types of orbital rim fractures. A zygomatic fracture, which is a fracture involving the lower edge of the rim of the eye, which is part of the jawbone. There is also a frontal bone fracture. It is a fracture involving the upper edge of the corner of the eye, which is part of the frontal bone. Fractures in this area are usually caused by car accidents. It is possible to encounter orbital edge fractures as a result of severe trauma in car accidents. Therefore, an ophthalmologist should be consulted immediately after the accident.
Burst fracture
A burst fracture is a break in the base or inner wall of the orbit or eye socket. A crack in the very thin bone that forms these walls can compress the muscles and other structures around the eye, preventing the eyeball from moving properly. Sudden and hard blows, such as a blow from a fist, can often cause a burst fracture. A burst fracture may not be felt in the immediate situation. For this reason, an ophthalmologist should be consulted in case of sudden blows to the eye area.
Orbital base fracture;
This is when a blow or trauma to the orbital rim pushes the bones back and causes the bones of the base of the eye socket to bend downwards. An orbital base fracture can also affect the muscles and nerves around the eye, preventing it from moving properly and feeling normal.
What are the Symptoms of an Orbital Fracture?
- Blurred, reduced or double vision
- Black and blue bruising around the eyes
- Swelling of the forehead or cheek
- Swollen skin under the eyes
- Numbness on the injured side of the face
- Blood in the white part of the eye
- Difficulty moving the eye to look left, right, up or down
- Intense cheek pain when opening the mouth
- Swollen or sunken eyeballs
Diagnosis of Orbital Fractures
In the eye examination to be performed as a result of trauma, a detailed examination is performed according to the history of the impact. During the examination, visual functions, eye muscles, eyelids, cheek, upper lip and upper teeth are checked by the doctor and the eye is examined with an ophthalmoscope to check for internal damage. If the suspicion of an orbital fracture persists, a CT scan ‘computer tomography of the scanned area’ can be performed for a more comprehensive examination. A CT scan can diagnose an orbital fracture with an X-ray.
How are Orbital Fractures Treated?
In most cases, orbital fractures do not need to be treated with surgery. If the orbital fracture is small, the ophthalmologist may recommend placing ice packs on the area to reduce swelling and allow the eye socket to heal on its own over time. Sometimes antibiotics and decongestants may also be prescribed. An orbital fracture is more severe when it prevents the eye from moving properly, can cause double vision or repositions the eyeball in its socket. In this case, the ophthalmologist may refer the patient to an oculoplastic surgeon (a specially trained ophthalmologist) for surgery. In many cases, the oculoplastic surgeon may choose to wait a while to see how the healing process goes before operating. Waiting until the swelling goes down before surgery usually gives better results. If the symptoms of an orbital fracture disappear, it may be possible to avoid surgery and the possible complications associated with it.
Orbital fractures are important for your eye health. You should always undergo an eye examination after injuries that affect your eye area.
WHAT IS A STYE?
A stye is an infection of the eyelid glands. The disease can usually occur within 1 or 2 days.
WHAT ARE THE SYMPTOMS OF STYE?
The disease usually develops within 1 or 2 days.
The stye starts with pain in the eye, swelling of the eyelid, redness, burning and stinging.
WHAT IS THE TREATMENT OF STYE?
In the first week, it should be treated with hot water dressing and antibiotic drops. Otherwise, it may turn into a chalazion, i.e. a valve cyst.
WHAT IS CHALAZION?
Chalazion is a lid cyst.
If the stye turns into a chalazion, surgery should be performed within 1 month without waiting. Otherwise it may spread to other eyelids.
WHAT ARE THE SYMPTOMS OF CHALAZION?
The person with chalazion experiences pain, swelling and redness. As a result of the spread, it starts to recur frequently and may disrupt the structure of the eyelid and lower the eyelid slightly.
WHAT IS THE TREATMENT OF CHALAZION?
The chalazion should be operated on. The surgery should be performed by a specialized oculoplasty specialist and further spread of the disease to the eyelid should be prevented.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
STEM CELL APPLICATION IN EYE DISEASES

STEM CELL APPLICATION IN EYE DISEASES
What is a Stem Cell? How Does It Function?
A stem cell is an undifferentiated precursor cell that has not completed the maturation process. In simple terms, it is the purest, most basic form of cell. When stem cells are placed in a suitable growth environment, they can proliferate, renew themselves or maintain the continuity of their own cell community. They also have the potential to repair and functionalize the tissue following an injury to a part of the body. Because of this potential, they help repair damaged cells in the retina. These properties have led to the research and use of stem cells as a treatment option in many diseases. What Are Stem Cell Types and How Are They Obtained?
- Embryonic Stem Cells (ESCs): Obtained from embryonic tissues obtained through IVF, it is the stem cell with the highest potential. Embryonic stem cells are not used in our country for ethical reasons.
- Adult Stem Cells-Mesenchymal Stem Cells (MSCs): Their use is legal in our country. They are found in many tissues such as blood, blood vessels, fetal blood, umbilical cord, skeletal muscle, skin, teeth, bone marrow, fat, cartilage and are obtained from these tissues under laboratory conditions. The most commonly used MSCs are derived from adipose tissue, bone marrow and umbilical cord tissue.
Mechanisms of Stem Cell Action
Cell Replacement: Healthy stem cells can replace degenerating unhealthy stem cells.
- Nutritional Support: Healthy stem cells secrete growth factors and increase the life support of surrounding cells. MSCs mostly act through this mechanism.
Immune Modulation: With the help of the factors they secrete, MDCs help regulate the immune system and prevent autoimmune damage to the retina and optic nerve.
What is the Legal Dimension of Stem Cell Applications in Turkey?
In our country, stem cell applications are carried out at both clinical and research levels. The Stem Cell Advisory Board was established within the Ministry of Health in 2006 to provide the necessary support in this regard. Permission from this board is required for clinical trials and experimental treatments on humans.
Where are stem cells obtained and how are they produced?
Stem cells can be obtained from one’s own cells (autologous) or from another person (allogeneic). The most commonly used tissue as a source of stem cells is the umbilical cord tissue stored in stem cell banks. Apart from this, the person’s own adipose tissue or bone marrow can be used as a source of stem cells. Stem cells provided by ONKİM Stem Cell Technologies (ONKİM) will be used in the application to be performed on you, ONKİM Stem Cell Technologies (ONKİM) is a health company established in our country in accordance with the current organ and tissue transplantation law, blood and blood products law and regulations published by the Ministry of Health.
In Which Eye Diseases Can Stem Cell Transplantation Be Applied?
Stem cell applications are mostly used in hereditary retinal diseases, optic nerve diseases and hereditary corneal diseases. Among the retinal diseases, retinitis pigmentosa (popularly known as night blindness or chicken black), Stargardt’s macular dystrophy, especially the dry type of age-related macular degeneration (yellow spot disease) and other degenerative retinal diseases can be listed. Optic nerve diseases include optic atrophies caused by glaucoma, idiopathic, traumatic, hereditary or other causes. In these diseases, stem cell therapy can be applied if classical treatment methods do not yield results and the disease continues to progress.
How is Stem Cell Transplantation Performed in Eye Diseases?
Stem cell application is basically performed in 4 ways.
Subretinal Application: It is applied under the retina following vitrectomy surgery. It is an intraocular application.
Intravitreal Application: It is applied directly into the eye with a needle injection without vitrectomy.
Suprachoroidal Application: It is applied under the tissue called choroid under the retina by preparing a pocket outside the eye,
Subtenon Application: It is injected with a needle into the layer outside the eye called tenon.
In intraocular applications (subretlnal and intravitreal), the efficacy is high but the risk of complications is also high. The risk of complications is minimal in extraocular (suprachoroidal and subtenon) applications. Other than these, intravenous or optic nerve applications are rarely used,
What is the Effect of Stem Cells and What is the Duration of Effect?
The main purpose of stem cell application is to stop or slow down the progression of the disease and prevent progressive vision loss with the help of secreted growth factors. This treatment does not completely cure the disease. In 60% of the treated patients, vision improvement and visual field enlargement can occur. In 30-35% of patients, there is no visual improvement and the progression of the disease may slow down. In 5-10% of patients, the treatment may have no benefit and the disease may continue to progress. Success is never 100%. If the visual acuity before surgery is good, the visual field loss is low, the number of healthy retina and optic nerve cells is high, the probability of success after treatment increases. The earlier the treatment is performed, the better the outcome. Today, the longest followed-up patient group has a 5-year follow-up, and it is thought that the effect of the treatment can last up to 3-5 years on average. The duration of effect may vary individually according to the type of disease and may be shorter or longer than the stated duration. The maximum duration of effect is not yet known. If the effect decreases, stem cell treatment can be repeated. Stem cell treatment will not benefit the patient who has no vision at all.
Are There Risks of Stem Cell Therapy?
There may be stinging, itching, redness and swelling in the eye for a few days after the application. These complaints can be alleviated and relieved with medication. You may have a stinging complaint due to the stitch in your eye, this stitch will dissolve and fall off spontaneously within 2-3 weeks. You can return to your normal life 3 days after the procedure. As with all eye surgeries, complications such as increased eye pressure, infection, pain during eye movements, swelling of the lids, retinal edema, vitreous hemorrhage, detachment, and decreased vision can be seen very rarely after the surgical procedure. In case of a possible complication, additional procedures and treatments may be required to correct the complication. The high amount of growth factors secreted after stem cell application can stimulate retinal and optic nerve cells, leading to different images. After the application, some patients may have vision problems in blue, red, yellow, gray tones that persist for a few months. In addition, there may be occasional complaints of foggy and blurred vision, shimmering vision, and these complaints are expected to decrease and disappear over time. It is extremely unlikely that the MSCs used will cause any infection or allergic reaction. These cells are tested for all kinds of infections. The stem cells used do not carry antigens that cause tissue rejection (HLA) and therefore the risk of developing a tissue rejection reaction is very low. The tumorigenic potential of the stem cells is extremely low. To date, no tumor formation has been reported in the medical literature in any patient who has undergone CCM application.
Does Stem Cell Therapy Affect Other Treatments to be Performed in the Future?
After intraocular applications, there may be some conditions that may prevent other applications from being performed. However, since the suprachoroidal and subtenon applications to be applied to you do not enter the eye, it does not affect other future applications.
What is the preferred type of application in our hospital?
Mesenchymal stem cells (MSCs) are preferred as the cell type in our clinic. Umbilical cord, adipose tissue or bone marrow can be used as the source, and the most preferred one among these is umbilical cord-derived mesenchymal stem cell due to its high growth factor secretion potential.
Suprachoroidal and/or subtenon application is preferred as it is safer and does not interfere with other treatments to be performed later. These applications are very safe as they are extraocular applications.
The surgical procedure can be performed under general or local anesthesia according to the patient’s request. The surgery can be performed in one eye or in two eyes in the same session according to the patient’s request. After the surgery, the patient is given medication and drops to protect against infection for 1 month. Follow-ups are performed as often as your physician deems appropriate after the surgery. Complete eye examination, visual field, OCT and, if necessary, electrophysiology, angiography and ultrasonography tests are performed. During follow-ups, if deemed necessary by your physician, additional treatments may be recommended to increase the effectiveness and survival of stem cells. These additional treatments may include transcorneal electrical stimulation (Okuvizyon), platelet rich plasma (PRP), additional stem cell applications.
General Treatment Risks and Side Effects
Allergic shock during administration, although never reported
- Infection of the patient despite all safety precautions
- development of fever, rash, redness at the site of application within the first 48 hours
Additional problems that may be life-threatening but have never been reported
Depending on the problems that may develop after the application, the physician may not allow the next application or may change the application method by informing again:
Recurrence of the above-mentioned risks in each repetition of the application
- Transmission of disease from cells despite all kinds of examinations
Development of cancer, although never reported
- Weakened immunity, a tendency to infections or, conversely, autoimmune diseases (loss of function in all or some organs as a result of the immune system attacking other normally healthy organs of the body), the development of antibodies against given cells, the possibility of alloimmunization
After stem cell application, depending on the level of the disease, genetic background, personal factors or complications that develop, the amount of visual improvement may vary, some patients may not have any visual improvement at all, and even in rare cases, existing vision may be lost.
All these procedures are performed only upon the request and consent of the patient and/or his/her legal representative. Apart from the known complications that may occur, there may be other complications that may arise due to the very newness of the application and have not yet been identified.
Patients and their relatives should be aware of the possibility that the stem cell application may not be clinically and/or laboratory useful.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Contact
- Karanfil avenue . Alkaranfil street No: 4 Ofis No: 1 Beşiktaş / İstanbul
- +90 850 220 17 21
- info@checkupway.com

