Robotic Spine Surgery
Robotic spine surgery is a surgical procedure performed with modern medical technologies in the world’s leading surgical centers. Robotic surgery is generally applied in the treatment of spinal disorders such as kyphosis, scoliosis, canal stenosis, slipped disc and herniated disc surgery, which occur in the back and waist parts of the spine. Robotic systems, which enable spine surgeries to be performed with high precision and accuracy, minimize the risks that may occur in the treatment of spine diseases.
The most important advantage of spine surgeries performed with robotic systems is that the surgical procedure is performed with small incisions and the screws are inserted into the vertebrae with high accuracy and precision. The most accurate placement of screws and other implants greatly reduces the most feared risks of spine surgery such as vascular and nerve injury and paralysis. Thus, it offers a safer and more successful surgical experience for both patients and surgeons. With all these features, robotic technologies usher in a new era in spine surgery.

What is Robotic Spine Surgery?
Robotic spine surgery is a minimally invasive surgical procedure that guides the doctor through all the delicate processes from planning the surgery to placing the implants in the spine in the most appropriate position and angle. Implants such as pedicle screws, rods and cages are used in the surgical treatment of various physical disorders such as slipped discs, multilevel herniated discs, canal stenosis and scoliosis. These types of spinal implants are used for different purposes such as fixing the vertebrae together, correcting structural defects and curves in the spine, maintaining the gap between two vertebrae, immobilizing part of the spine by holding the vertebrae together.
In order for the results of spine surgery to be successful; it is important that the implants are placed in the spine in 3D (3 dimensional) in the most accurate way. In order to plan this process in 3D and to implement it according to the plan, extremely precise technical measurements are required.
The most accurate placement of screws and other implants reduces the most feared risks of spine surgery, such as vascular-nerve injury and paralysis. Thus, technically more precise and safer surgical procedures are performed and more successful results are achieved.
Robotic Surgery in the Treatment of Spine Diseases
The state-of-the-art MAZOR robotic system is used in the surgical treatment of problems in different parts of the spine such as the back, waist, sacrum and sacroiliac joint. Some of the spine diseases where robotic spine surgery is applied are as follows:
- Canal Stenosis (Spinal Stenosis),
- Low Back Dislocation (Spondylolisthesis),
- Scoliosis,
- Kyphosis (hunchback),
- Lumbar Hernia
- Spine Fractures
Surgery is not always the first choice in the treatment of structural or painful conditions, except in patients with urgent fractures of the spine and severe neurological dysfunction such as weakness in the legs and incontinence. Non-operative methods such as medication, bracing, physical therapy, exercise and spinal injections should be applied first. However, surgical treatment is recommended for patients whose complaints do not improve despite regular treatment. Delay in surgical treatment of spine diseases can lead to serious problems in patients.
Advantages of Robotic Spine Surgery
Robotic spine surgery has many advantages such as high accuracy in screw placement, less blood loss and low risk of complications. The advantages of the new generation robotic system MAZOR in spine surgery are as follows:
- High accuracy: Robotic spine surgery provides 99.5% or more accuracy in placing pedicle screws or other implants into the spine.
- Short and fast recovery time: Robotic spine surgery allows patients to recover faster and easier from even the most complex spine surgeries. Research shows that patients who undergo robotic spine surgery experience shorter hospital stays and faster recovery.
- Less radiation: In robotic spine surgery, patients and the healthcare team are less exposed to radiation. Especially with the use of the O-Arm device during surgery, the amount of radiation exposure of patients is further reduced.
- Minimally invasive surgical procedure: In surgeries performed with the robotic spine surgery system MAZOR, small surgical incisions are applied. This results in less bleeding during surgery, less scarring and faster healing after surgery.
- Reduced operation time: In surgeries performed with the robotic spine surgery system MAZOR, the time for screw placement in the vertebrae is shortened. While the placement time of a screw in traditional spine surgery is approximately 6-7 minutes, this time is approximately 2 minutes in robotic spine surgery.
- Surgery planning: Each patient’s spine shape and anatomy is customized for the specific surgical plan.
- Postoperative pain: After surgery performed with the robotic spine surgery system, patients have less pain during the recovery period. During this period, patients move more comfortably and experience an easy recovery process.
- Risk of infection: Patients have a lower risk of infection after surgery with the robotic spine surgery system MAZOR compared to traditional spine surgeries.
- Revision surgery Since robotic spine surgeries are performed with high accuracy, the need for another surgery, called revision surgery, is reduced.
- Risk of complications: The robotic spine surgery system MAZOR provides highly accurate screw placement, reducing the risk of muscle weakness or paralysis due to spinal cord or nerve injury.
Why High Accuracy in Pedicle Screw Placement is Important?
Accuracy is critical in robotic spine surgeries for two main reasons. First, an incorrectly placed screw, even by a few millimeters, can lead to ongoing back pain, slower recovery and repeat surgery. In addition, placing pedicle screws in the wrong position in the spine can cause excessive load on the screw, which can cause damage to the screw.
The second reason is that spine surgeries are performed close to sensitive nerve structures and the spinal cord. If the screws placed in the spine are placed in a way that causes damage to the spinal cord, it can lead to paralysis and nerve damage. Depending on the screw size not being adjusted; if the screws advance too far into the interior, it can cause injuries to the internal organs.
How is Robotic Spine Surgery Performed?
In robotic spine surgery, as in traditional spine surgery, pedicle screws, rods or cage-type implants are inserted into the damaged spine area between two vertebrae. In surgeries performed with MAZOR, the robotic system used in spine surgery, these procedures are planned with extremely precise and detailed calculations. In addition, the surgeon’s ability to follow the operations performed during the surgery simultaneously and in 3D ensures that the surgery is performed in accordance with the plan.
In robotic spine surgery; CT (Computed Tomography) images of patients before surgery or X-ray images obtained from the O-Arm device during surgery are transferred to the MAZOR robot computer. Then, a special 3D surgical plan is created for each patient on the screen and the position, angle and dimensions of the pedicle screws are determined. This allows the surgeon to anticipate the problems that may occur during surgery and to perform the surgery with fewer incisions.
In this process, the surgeon monitors the determined trajectory, screw size and angle in real time and in 3D. Spine surgeries performed using the robotic spine surgery system MAZOR are performed faster and with higher accuracy. This significantly reduces complications that may occur during or after surgery.
Robotic spine surgeries are performed in three different ways: closed, minimally invasive and open.
In closed spine surgeries (endoscopic spine surgery), screws are not inserted into the spine. However, robotic systems can be used to access the spine during surgery. In robotic spine surgery performed with the minimally invasive method, 1cm incisions are made in the areas where pedicle screws will be placed and procedures are performed with minimal incisions.
When Should Robotic Spine Surgery Be Considered?
Physical therapy, exercise, corset, medication and spinal injection treatments can be applied before robotic spine surgery is decided. However, despite all treatments, surgery should be considered if you have pain that makes your daily life difficult, numbness in your legs and conditions that affect your social life. In case of serious symptoms such as weakness in the legs, bowel and bladder control due to spinal disorders, patients need urgent surgery.
Patients’ knowledge about spine surgery helps to reduce their concerns about the surgery. It is also effective in managing the pre- and post-operative process in the best way. For this reason, it is important for patients who will undergo spine surgery to get information about robotic spine surgery by researching the surgery options, methods and technologies to be used.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Scoliosis, How is it Treated and Operated? What are the Risks?
Scoliosis, also known as curvature of the spine, affects millions of people in the world and more than 2.5 million people in Turkey. Every year, thousands of children start corset treatment for scoliosis and thousands of people with severe curvature undergo scoliosis surgery.
The age of onset of scoliosis, which can develop in infancy or early childhood, is usually 10-15 years old. Even if you or your child has a mild spinal curvature, you may not always notice any symptoms. However, early detection of scoliosis can reduce its long-term negative impact on quality of life. Therefore, scoliosis awareness is important not only for parents but also for all people and institutions that care for children, including teachers. One of the first steps is for parents to monitor their children for signs of scoliosis or for health screenings in schools. Every year, June is recognized as Scoliosis Awareness Month to raise awareness about scoliosis worldwide and increase public awareness. Even if you are not aware of it at the moment, it should be taken into consideration that you or your child may have a curvature of the spine. You can read the rest of our article to learn about scoliosis (curvature of the spine), its symptoms and treatment methods and to determine the steps you will take. If you think that you or your child has scoliosis symptoms, you can consult our specialist physicians.
What is Scoliosis (Spinal Curvature)?
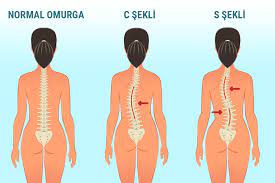
Scoliosis (curvature of the spine) is a 3-dimensional spinal deformity in which the spine bends sideways to form an “S” or “C” shape. Our spine is made up of bones called vertebrae, which are stacked on top of each other. A healthy spine has a natural curvature that helps us bend and move. However, when our spine curves more than this natural curve, creating a sideways curve, a condition known as scoliosis occurs.
In order for the curvature of the spine to be defined as scoliosis, it must be a curve of at least 10 degrees. This angle is also known as the “Cobb angle”, a measure of curvature. There can be as little as 10 degrees of curvature or as severe as 90 degrees or more. The treatment of spinal curvature is planned according to the severity of the condition and the main goal is to relieve the symptoms.
The curvature can occur anywhere in the spine, but most commonly in the back and lumbar spine. Scoliosis can be congenital and can occur in any age group. However, it is most common in adolescents between the ages of 10 and 16. Most of these are scoliosis of unknown cause (idiopathic).
What Causes Spinal Curvature (Scoliosis)? What are the Types?
There are various causes of spinal curvature; congenital scoliosis, i.e. congenital scoliosis, can occur, or spinal curvature can occur due to other diseases such as cerebral palsy, muscular dystrophy, spina bifida. Spinal curvature may not always be recognized. You may learn that your child has scoliosis when you go to the doctor with complaints such as back pain or back pain or during health screenings at schools.
Contrary to popular belief, factors such as carrying heavy backpacks, sleeping on your side and poor posture do not cause spinal curvature. In most cases, the cause of spinal curvature is unknown, i.e. idiopathic scoliosis. Although the cause of this type is unknown, genetic factors are thought to be effective. There are 3 types of idiopathic scoliosis depending on the age at which the deformity develops.
Infantile idiopathic scoliosis develops after birth until 3 years of age
Juvenile idiopathic scoliosis develops between 4 and 9 years of age
Adolescent idiopathic scoliosis develops between 10-18 years of age
Adolescent scoliosis is the most common group, accounting for approximately 80% of all idiopathic cases. Adolescence is generally a time of rapid growth. If any abnormality is detected at this stage, it should be closely monitored to see if the curve is progressing. In cases detected at an early stage, treatment is possible with methods such as follow-up, spinal curvature exercises and corset use. The most common cause of scoliosis in adults is the deterioration of the spinal discs as they age, i.e. disc degeneration.
There are also structural and non-structural types of spinal curvature. In the case of non-structural curvature, the structure of the spine is normal, but a condition such as a difference in leg length or an infection causes the curvature of the spine. When the underlying cause is corrected, the spinal curvature is also corrected. In the structural type, injuries, congenital defects, metabolic conditions cause spinal curvature and if left untreated, the curvature can be permanent.
What are the Symptoms of Scoliosis?
Spinal curvature of 10 degrees or more is defined as scoliosis. However, mild curves of 10 degrees usually do not show any symptoms. As the curvature increases to 20 degrees and above, symptoms begin to be noticed.
If you have a spinal curvature during adolescence and did not notice it at an early stage, you may notice the development of scoliosis symptoms as you age. In children, scoliosis symptoms should be monitored as spinal curvature does not cause much back pain.
Symptoms of scoliosis in childhood can usually be listed as follows, as shown in Figure 2;
Shoulder curvature, different shoulder heights,
Irregular hip alignment,
The arms are not straight next to the body when the child stands straight,
The two sides of the back are at different heights when the child bends forward.
In adults, back pain is often the first symptom of spinal curvature. As the spine curves, it can put pressure on nearby nerves and cause complaints such as weakness and numbness.
Some of the symptoms of scoliosis in adults are as follows:
- Different shoulder alignment,
- Irregular hip alignment,
- Irregular waist line,
- Numbness, weakness or pain in the legs,
- Difficulty standing upright,
- Feeling of fatigue.
Treatment of spinal curvature is successful with early intervention. If you notice any symptoms in yourself, your child or a relative, you can contact us for early diagnosis and treatment and consult our specialist physicians.
How is spinal curvature treated?
Spinal curvature treatment is planned to relieve complaints such as back pain and to prevent the progression of the curvature. In most cases, a mild curvature of 10-20 degrees does not cause any complaints and your doctor will ask for periodic check-ups to see if the curvature is progressing.
If the curvature of your spine has started to cause a noticeable deformity in your body posture or complaints such as back pain, or if the curvature was severe when first detected, different treatment methods are applied depending on factors such as age, severity, location and progression of the curvature, and bone maturity.
Some spinal curvature treatment methods other than surgery are as follows:
- Corset for curvature of the spine,
- Physical therapy and rehabilitation
- Exercises for curvature of the spine,
- Schroth method.
The use of a corset for spinal curvature during the period of growth in children can help to stop the progression of the curvature.
What is Scoliosis Surgery?
There may be cases where the angle of curvature in the spine continues to increase despite treatments such as physical therapy, spinal curvature exercises and corset use. In severe cases where this curvature is over 45 degrees, scoliosis surgery is recommended. Scoliosis surgery is performed to correct the abnormal curvature of the spine and relieve complaints. Scoliosis surgery is the last option due to the risks and complications. However, some of the signs that indicate the need for surgical treatment include
- Exacerbation of back and leg pain caused by curvature of the spine,
- Failure to benefit from non-operative treatments,
- Progression of the curve of the spine (over 45 degrees).
Leaving a progressive curvature of the spine untreated can lead to serious health problems such as worsening pain and breathing difficulties. It is therefore important that you carefully consider the decision to undergo surgery and work with your doctor to determine the best option for you.
How is spinal curvature (scoliosis) surgery performed?
The methods used in scoliosis surgery differ from person to person. For example, in children with ongoing bone maturation, surgical methods that adapt to the growth of the spine with extensible systems or scoliosis surgery can be applied.
With extensible systems, rods and screws used to help correct the curvature of the spine are fixed to the spine. Every 6-12 months, your surgeon adjusts the length of the rods to adapt to the growth of the spine.
One of the common methods used for scoliosis surgery is spinal fusion. In this technique, two or more vertebral bones are fused together into a single bone to correct the curvature of the spine. The surgeon straightens the spine by inserting rods and screws. The surgeon then places small pieces of bone, called bone grafts, into the area like a patch. The bones of the spine are then fused together and the bones grow together to form a single bone.
Is Spinal Curvature (Scoliosis) Surgery Risky?
The question of whether scoliosis surgery is risky is one of the most curious ones. Spine surgeries require extremely sensitive surgical procedures as they take place around the nerve roots and spinal cord. Damage to a nerve during surgery can cause neurological damage and complications such as paralysis. Therefore, it is quite normal to be concerned about the decision for surgery.
Spine surgery carries some significant risks due to its proximity to the main blood vessels and nerves (spinal cord). Knowing the complications and possible risks after scoliosis surgery is extremely important for the surgical process and afterwards.
Complications such as infection, nerve damage, blood loss, intestinal and bladder problems are among the risks of scoliosis surgery. Additional risks associated with scoliosis surgery include loss of spinal balance and failure of the bones to heal and fuse properly.
The risks of scoliosis surgery include the following:
- Infection
- Excessive blood loss
- Deep vein thrombosis
- Complications associated with the lungs
- Stomach and intestinal problems
- Neurological complications due to nerve and spinal cord damage
- Problems such as breakage or displacement of materials such as screws and rods used in surgery
The most serious complications after scoliosis surgery are neurological complications, that is, risks related to the nervous system. These risks include loss of sensation, weakness and numbness in the legs and feet, impaired bowel and bladder function and paralysis. Some of these may resolve over time, but there are also permanent conditions.
Although neurological damage and paralysis are rare risks, their effects can be devastating. It is therefore important to be aware of the possible risks and know your options.
Robotic Scoliosis Surgery and Spine Surgery
In order to minimize the risks of spinal curvature surgery, modern technologies have been developed that allow the surgery to be performed with high precision. The most important of these technologies is robotic spine surgery. Thanks to the use of robotic spine surgery, scoliosis surgeries are much more reliable today.
In scoliosis surgeries performed with robotic spine surgery;
- Surgical instruments such as implants and screws are placed in the most accurate way
- Surgery is performed with high accuracy and precision
- An operation plan suitable for each patient’s own spine anatomy is made
- Thus, risks such as nerve injury and paralysis are minimized
Scoliosis surgery to prevent the progression of spinal curvature and correct the deformity of the spine is beneficial for many patients. However, before making the final decision for surgery, remember to carefully consider the potential risks and the safest options to reduce these risks with your doctor.
What Should Patients Pay Attention to After Scoliosis Surgery?
The recovery process after scoliosis surgery varies from person to person and according to the complexity of the surgery. Factors such as the type of surgery, your general health condition and your age affect the recovery process. There are some points that patients should pay attention to during this process. For example, you should not bend over, lift loads, drive a car or do too much physical activity in the first few weeks.
One of the most important issues you should pay attention to after scoliosis surgery is infection. To prevent infection, the surgical site should be kept clean and dry. You should also take the medication prescribed by your doctor regularly to prevent pain and the risk of infection.
We can list the things to be considered after scoliosis surgery as follows:
- In the early days, plan to have someone with you who can help with some basic care needs and daily tasks.
- Avoid movements such as bending, heavy lifting.
- If your doctor has recommended a postoperative corset, take care to use it regularly and avoid risky movements.
- You will be given instructions to follow at home before you are discharged from hospital. Follow these recommendations as closely as possible.
- School-age patients can usually return to school partially within one month after surgery. However, you need to follow the time frame set by your doctor to return to activities such as physical education and exercise.
- In the first period after scoliosis surgery, you should not drive. Potholes and bumps in the road are dangerous as they can cause sudden movements. As you continue to heal, your doctor will allow you to drive.
- About 6 weeks after the spinal fusion surgery, your surgeon will order X-rays to evaluate the process. Accordingly, he/she will decide which activities you can continue or which you should avoid.
- If you have a job that does not require intense physical activity, you can usually return to work 4-6 weeks after surgery. However, it may take a little more time before you can resume more strenuous work.
- Do not neglect to follow your controls in the postoperative period and consult your doctor if you have any questions.
With the latest developments such as robotic spine surgery, most patients can be discharged more quickly and experience a faster and more painless recovery. As the only center that performs robotic spine surgery in Turkey, you can contact us for more information and evaluate your options with our surgeons.
Frequently Asked Questions About Scoliosis Surgery
At what degree of curvature of the spine does scoliosis require surgery?
For curvatures of 45 degrees or more, scoliosis surgery is required to reduce the curvature or prevent its progression. Conditions such as problems with lung function (difficulty breathing), severe back and leg pain, and difficulty in standing are signs that scoliosis surgery is needed due to severe spinal curvature. Today, modern surgical methods (robotic spine surgery) can significantly improve abnormal curvatures of the spine.
How long does it take to recover from scoliosis surgery?
The recovery period after scoliosis surgery varies depending on the type of surgery and the individual. You are usually discharged from the hospital after 3-4 days. You will gradually return to your activities within 2-6 months depending on your recovery status. Children usually return to school in 4-6 weeks after surgery. After spinal fusion, it takes approximately 6-12 months for the spine to heal completely and return to your old activities.
Are the screws removed after scoliosis surgery?
In the surgical treatment of scoliosis, your surgeon corrects the curvature of the spine using screws and rods. Removing the screws and rods requires a second operation. This causes further damage to the spine and surrounding tissues. Therefore, screws and rods do not need to be removed unless there is an infection or fracture.
Does the curvature of the spine recur after surgery?
Scoliosis (curvature of the spine) is not expected to recur after surgery. However, risks such as failures in the surgical method or postoperative complications can sometimes lead to an increase in the curvature of the spine. In other cases, if the postoperative follow-up is not performed properly in children who are still growing, the curvature of the spine may increase slightly.
In cases where scoliosis surgery is required, a completely individualized surgery plan should be made. Although modern medicine and technological methods minimize the risks associated with spine surgery, do not forget that every surgical intervention has potential risks. Therefore, always share your fears and concerns about surgery with your orthopedic surgeon. You can evaluate your options and make the final decision together with your doctor.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
What is Humpback (Kyphosis)?

Kyphosis (hunchback) is a deformity of the spine that causes the upper back to appear more curved and hunched than normal as it bends forward. The spine structure generally consists of 3 parts:
- The cervical spine consists of 7 vertebrae, which are located at the top of the neck and allow us to move our neck
- The thoracic spine includes 12 vertebrae in the back,
- The lumbar spine consists of 5 lumbar vertebrae in the lower back.
In a healthy spine, each section has a natural curve when viewed from the side. This natural curvature of the spine is seen as a hollow in the lumbar and cervical regions and a slight hump in the back region, which bulges outwards. The natural hump angle in the back is between 20-45 degrees
The natural curvature of the healthy spine is important for balance, supports our posture and helps us to stand upright. However, if this curvature is more or less than it should be, it is difficult to stand upright and posture disorders can occur. A back curvature angle of 50 degrees or more is known as hyperkyphosis or kyphosis (hunchback).
What are the Types of Kyphosis?
This disease, which can occur at any age, is more common in adolescents and older women. The most common causes of kyphosis in children and adolescents are as follows:
- Postural Kyphosis: This is the most common type of hunchback that occurs most often during adolescence and develops due to poor posture. Generally, this type of hump can be corrected with methods such as posture correction and kyphosis exercises and does not cause serious problems in adulthood.
- Scheuermann’s kyphosis Scheuermann’s kyphosis is a developmental type of kyphosis, meaning it occurs during growth. It affects the upper back and causes the spine to bend too far forward in the back. It is named after the Danish radiologist who first described this condition. It is more serious than postural kyphosis and can cause pain in some cases. Standing or sitting for long periods of time worsens the pain.
- Congenital Kyphosis: This is a congenital condition that occurs when the development of the spine is not normal while the baby is in the womb. As the curvature of the spine becomes more pronounced as the child grows, kyphosis surgery is usually required.
The severity of the curvature of the spine and hunchback varies from person to person. Generally, the greater the curve, the more severe the symptoms and complaints of kyphosis. In severe cases, a severe curvature of the back can cause pain or pressure on the lungs, leading to heart and respiratory problems. Kyphosis surgery should be performed if the hump angle is over 75 degrees and the curvature tends to progress.
What are the Symptoms of Kyphosis?
Apart from the abnormal curve of the back and the hunched appearance, sometimes there may be no symptoms or the patient may only complain of mild back pain. However, in severe curvatures, the patient’s back may cause significant hunchback and other symptoms.
Depending on the severity of the back curvature, the symptoms of kyphosis are as follows:
- Back pain and stiffness
- Tenderness in the spine
- When leaning forward, the upper back appears higher than normal
- Difference between right and left shoulder heights
- Difficulty looking up and across
Symptoms of severe hunchback include difficulty breathing and eating, and rapid fatigue. In addition, the symptoms worsen as the curvature of the back increases.
If you are experiencing symptoms of hunchback or if your complaints are increasing over time, you can consult our spine health specialists without delay. Please contact us about the most up-to-date treatment methods.
What Causes Humpback?
Hunchback can be congenital, but it can also occur during adolescence or later in life for various reasons. It is more common in young people whose bones grow rapidly. Also, as we age, our vertebrae lose their flexibility and the spine starts to lean forward, which can be the cause of hunchback.
There are different causes of hunchback. For example, postural kyphosis can be caused by posture disorders, such as carrying heavy bags. Scheuermann kyphosis is caused by a structural defect in the spine due to the vertebrae not developing properly. Congenital kyphosis is a congenital type and develops due to problems in the spine while still in the womb.
The causes of hunchback are usually the following:
- Impaired posture
- Scheuermann’s disease
- Aging
- Collapse of the back vertebrae due to osteoporosis
- Spinal injuries and fractures
- Infection
- Cancer and cancer treatments
- Metabolic problems
- Neuromuscular diseases
- Spina bifida
How is Humpback (Kyphosis) Diagnosed?
The diagnosis of kyphosis requires a detailed medical examination. During the examination, your doctor will check your balance, range of motion, reflexes and muscle strength. To better visualize the curvature of the spine and to observe any spinal deformity, you will be asked to bend forward at the waist with your arms at your side to assess the hump in your back. In addition, a medical history should be taken and, if the patient is a child, a history of development at birth or during growth.
After the symptoms have been examined, radiological examinations such as X-rays, computed tomography (CT), magnetic resonance imaging (MRI) will be ordered to confirm the diagnosis and make a treatment plan. X-rays usually confirm the diagnosis of kyphosis and determine the degree of curvature. However, if the patient experiences muscle weakness, an electromyography (EMG) test, which measures the function of nerves and muscles, will be required.
In cases of kyphosis that occur in adulthood, additional tests are needed to determine the underlying cause. Investigations such as bone density measurements to determine how strong your bones are and blood tests to look for infection.
How is kyphosis (hunchback) treated?
Early diagnosis is extremely important for the treatment of kyphosis, especially in children and young people. Most mild spinal curvatures go unnoticed as they do not cause any symptoms or complaints. In mild cases, exercises and methods such as kyphosis bracing are recommended to improve posture and strengthen the muscles in the back. However, in more advanced cases, there are complaints of pain, severe spinal deformities and even breathing difficulties. Patients with severe hunchback may require kyphosis surgery to reduce excessive spinal curvature and relieve symptoms.
Correcting your posture, physical therapy and exercises to strengthen your back muscles are usually sufficient to correct hunchback caused by poor posture. However, for the treatment of kyphosis due to structural spinal disorders, treatment options should be evaluated according to age, gender and severity of spinal curvature.
Non-surgical methods applied in the treatment of humpback are as follows;
- Painkillers are used to relieve back pain.
- Physical therapy and exercise help to strengthen back muscles, increase spinal flexibility, relieve back pain and improve posture.
- Kyphosis corset; kyphosis corset (humpback corset) is used to prevent the progression of curvature in children with mild to moderate kyphosis who continue to grow. It is generally recommended to use a kyphosis brace until the skeletal structure reaches maturity. In adults, bone growth is complete and the brace may not help to correct the curvature of the spine. However, in women, a brace is recommended for kyphosis caused by collapse of the vertebrae due to osteoporosis (bone loss).
In order to follow the progression of spinal curvature in young people and children, it is very important to continue to follow up with careful observation of the family and regular medical examinations.
Kyphosis Surgery
Kyphosis surgery is recommended for patients with a hump angle of more than 75 degrees as a result of examinations and tests. Young people with hunchbacks that cause severe pain or appearance concerns may also prefer to correct this deformity with surgery.
Kyphosis surgery is performed in the following cases;
- In cases where the curvature of the spine is very pronounced (75 degrees or more)
- In the presence of pain that cannot be controlled with medication
- Problems such as difficulty breathing
- If neurological symptoms occur
- In cases where spinal curvature progresses despite other treatments
Kyphosis surgery helps to correct the curvature of the spine, improving the appearance of your back and relieving back pain. In cases where kyphosis surgery is required, you can benefit from surgery both aesthetically and in terms of eliminating complaints about your health.
Kyphosis surgery is usually performed with a surgical technique called spinal fusion, in which the vertebrae causing the curvature of the spine are joined together. Spinal fusion is the most common surgical procedure used to reduce the degree of curvature in the spine.
Spinal fusion surgery for kyphosis is similar to a welding procedure. The vertebrae causing the hump are fused together into a single solid bone. This reduces the degree of curvature.
During humpback surgery, the surgeon accesses the spine through an incision in the middle of the back. Metal screws and rods are used to help align the vertebrae. Once the vertebrae are aligned, small pieces of bone called bone grafts are placed into the spaces between the vertebrae. In this way, similar to the healing of a broken bone, the bone fragments placed between the vertebrae grow over time so that the vertebrae fuse together.
The aim of kyphosis surgery is to correct the hump within safe limits. The surgery takes 4-8 hours. After the surgery, you may need to stay in the hospital for 3-4 days or more depending on your general health condition. You may be asked to wear a back support corset for up to 9 months to support your spine during the postoperative recovery process. You can gradually start school or light work within 4-6 weeks after kyphosis surgery. You can usually return to non-impact sportive activities 1 year after surgery.
It should be kept in mind that kyphosis surgery carries some risks like every surgical procedure. In addition to general surgical risks such as infection and bleeding, there are risks such as paralysis due to damage to the spinal cord and nerves passing through the spine. For this reason, it is important to research your options when deciding on spine surgery.
Robotic Kyphosis Surgery
Robotic spine surgery is a new generation technology that minimizes the risk of spine surgeries and enables the surgery to be performed with high reliability and precision. Kyphosis surgery can be performed with robotic spine surgery. Thanks to robotic technology, screw placement in the spine during surgery is performed with an accuracy rate of over 99.5%, which minimizes the risks associated with surgery such as nerve damage, paralysis and vascular injury. In addition, robotic spine surgery is performed with the best adaptation to the unique anatomical structure of your spine.
Some of the advantages of kyphosis surgery with robotic spine surgery include
- During surgery, surgical instruments such as screws are inserted into the spine in the most accurate and precise way,
- Surgery is performed in the most appropriate way for your anatomy,
- Procedures such as screw positioning in the spine are monitored simultaneously with 3D imaging during surgery, which minimizes the margin for error,
- High accuracy and precision minimize the risks of spine surgery,
- Postoperative recovery is painless and faster.
Frequently Asked Questions About Humpback (Kyphosis)
Can sports correct hunchback?
Postural kyphosis caused by poor body posture is usually corrected by posture correction, physical therapy and kyphosis exercises. Studies have also shown that sports and exercise have positive effects on kyphosis.
Which doctor should I see for treatment of kyphosis?
Kyphosis (hunchback) is a condition caused by a deformity of the spine. Therefore, you should see an orthopedic doctor who specializes in the diagnosis and treatment of spinal disorders.
Which movements can correct a hunchback?
Kyphosis exercises and stretches to strengthen your back muscles are recommended for the prevention and treatment of hunchback due to posture disorders. As an example of a hunchback exercise, you can try the Superman movement; lie face down on a flat surface and stretch your hands forward. Keep your head in the center, looking at the floor and try to lift your arms and legs up towards the ceiling. Hold for 3 seconds and repeat the movement 10 times.
You can start kyphosis exercises with a doctor or physiotherapist, and it will be useful to repeat them at least 3-4 times a week to see results over time.
How long does it take to treat kyphosis?
There are different types of kyphosis that require different treatments. Depending on the cause of the kyphosis, the severity of the spinal curvature and age, treatment options and treatment times will vary. For example, children with mild to moderate kyphosis are asked to wear a kyphosis brace until bone growth is complete. In severe cases requiring kyphosis surgery, recovery after surgery may take 4-6 weeks or more.
Depending on the cause, kyphosis (hunchback) can be treated with non-surgical methods in many cases when diagnosed early. However, if the curvature of the spine progresses, it may cause serious problems. In this case, you should consider kyphosis surgery to lead a healthier and more active life.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Kyphoplasty / Vertebroplasty?
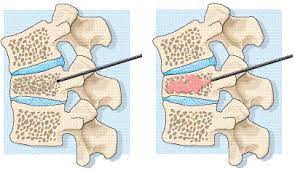
Kyphoplasty / vertebroplasty are methods used to treat collapse fractures that occur in the body of the vertebral bones that make up the spine. Collapse fractures in the vertebrae cause the height of the spine to decrease and the spine to bend forward. This results in back pain and hunchback.
Osteoporosis (osteoporosis), which is caused by a decrease in bone density, is the main cause of vertebral compression fractures. Another cause is tumoral conditions that weaken the bone structure.
Who can undergo kyphoplasty / vertebroplasty?
To undergo a kyphoplasty / vertebroplasty procedure, you must be suffering from progressive pain in your spine caused by a collapse fracture due to osteoporosis or a tumor. These patients often have difficulty moving and functional limitations due to the fracture.
Radiological imaging tests such as X-rays, computed tomography, magnetic resonance imaging (MRI) and bone scintigraphy can be used to diagnose spinal fractures. Bone density measurement should also be performed in patients with osteoporosis.
What should be done before kyphoplasty / vertebroplasty?
- Physical examination is performed
- X-ray images of the spine are taken
- The patient is informed about the disease
- Allergy history of the patient is questioned
- Medications used by the patient are recorded
- Routine blood tests are performed before the intervention
- Stop eating and drinking 6 hours before the procedure
- Aspirin etc. blood thinners are discontinued if possible
How is kyphoplasty / vertebroplasty performed?
Depending on the spine surgeon’s preference, the procedure can be performed under local or general anesthesia. During the procedure, the patient lies face down. The location of the fracture is determined with the help of a device called fluoroscopy, which can provide moving images, and local anesthesia is applied to the skin at the fracture level. Afterwards, a needle called trocar, which is designed to be intertwined with a cannula, passes through the skin and rests on the broken bone.
The trocar, which is placed in the appropriate position under fluoroscopic visualization, is advanced into the bone. After the trocar takes its final position, the inner needle is removed and the outer cannula is left in the bone. The balloon sent through this cannula is then inflated inside the broken bone, allowing the collapsed vertebra to regain height. The cement, which has been prepared outside and has the consistency of putty, is then injected into the vertebral bone through this cannula. Depending on the doctor’s preference, a balloon may or may not be used. If a balloon is used, the procedure is called kyphoplasty, if not, it is called vertebroplasty.
What are the risks of kyphoplasty / vertebroplasty?
Kyphoplasty / Vertebroplasty is a very low-risk procedure. There is a low risk of infection and bleeding. If osteoporosis (osteoporosis) is present, complaints of back pain, numbness and tingling may increase. You may need osteoporosis treatment to reduce these risks.
Recovery after kyphoplasty / vertebroplasty
Kyphoplasty / Vertebroplasty is a daily procedure and does not require hospitalization. As soon as you come to your room after the procedure, you may feel that the pain is relieved. However, sometimes it may take a few days for the pain to subside. You can leave the hospital and go home the same day. Driving may be difficult after the procedure. We therefore recommend that you have someone with you.
You may feel pain at the entry point of the trocar, which can be controlled with painkillers for a few days. It will be useful to apply ice therapy to prevent swelling. If there are signs of infection such as redness, swelling, discharge in the area where the procedure was performed, excessive bleeding, increasing pain, pain in the legs, numbness, loss of strength, contact your doctor.
You can return to daily activities immediately, but you should not lift heavy loads for the first 6 weeks after the procedure. We recommend following a light exercise program for the spine.
Conclusion
Usually within 48 hours after the procedure, the pain associated with the fracture subsides and the patient regains mobility. In some patients, the pain may disappear immediately after the procedure. The majority of patients regain their pre-fracture condition within days. After the procedure, 75% of the patients return to their active lives due to the regression of the complaints related to the vertebral fracture.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Treatment methods in lumbar hernia
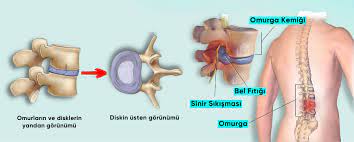
Lumbar disc herniation is a serious health problem that concerns a large part of the society, negatively affects the quality of life of the person, causes loss of workforce and functional limitations. Lumbar disc herniation constitutes a significant portion of doctor’s visits. In the treatment of lumbar disc herniation, most of the patients’ complaints are relieved with medication, corset, physical therapy and injections applied to the spine. However, surgical treatment becomes necessary in cases where non-surgical treatments fail.
Microdiscectomy is a technique that has been widely used in the surgical treatment of herniated discs for many years. In microdiscectomy operations, a 2 cm long incision is usually made. The muscle tissue is removed from the bone through the incision. Some bone tissue must be removed to enter the spinal canal. After the bone and connective tissue on the spinal cord is removed, the spinal cord membrane and nerve root are set aside and the hernia is accessed. The procedure is performed under a microscope.
Endoscopic discectomy (closed herniated disc surgery), on the other hand, has gained popularity in recent years due to the fact that it is performed through a smaller incision without the need to scrape muscle tissue and remove bone tissue. Due to less soft and bone tissue damage, closed herniated disc surgeries result in less pain and faster recovery.
What is closed herniated disc (endoscopic discectomy) surgery?
Endoscopic discectomy surgery is a closed surgical technique that can be performed through an 8 mm incision. A tube with a camera is sent through this small incision into the herniated disc. Working instruments are also sent through the tube to perform the surgery. After this stage, the surgery continues under endoscopic image guidance and monitored.
In endoscopic discectomy surgery, there is no need to remove muscle tissue from bone tissue. Bone tissue removal is not necessary most of the time, and when it is necessary, a very limited amount of bone is removed. In short, endoscopic discectomy is a technique that respects soft tissue and bone. It does not disrupt the natural spinal anatomy.
In which cases is endoscopic discectomy surgery performed?
Endoscopic discectomy, i.e. closed herniated disc surgery, can be performed on any patient who requires surgical treatment for a herniated disc.
– If there is severe back and leg pain and the person has difficulty in maintaining daily functions such as standing or walking,
– Incontinence or inability to pass stool or urine,
– Experiencing neurological symptoms such as increasing weakness and numbness in the leg muscles,
– In cases where medication, physical therapy and other non-surgical treatments do not result in a significant improvement in symptoms.
What are the advantages of endoscopic discectomy surgery?
The advantages of endoscopic discectomy surgery include the use of smaller incisions and less tissue damage;
- There is less bleeding during surgery.
- Patients complain of less pain after surgery.
- Patients can stand up and walk more quickly.
- They can leave the hospital and go home the same day.
- Patients can return to work earlier.
- Since no or less bone tissue is removed, the normal anatomy of the spine is not disturbed..
- Less scar tissue is formed compared to open surgery. This prevents adhesions and nerve compression caused by excessive scar formation that can be seen during tissue healing.
- The staining technique used in closed herniated disc surgery allows the herniated disc tissue to be distinguished from healthy disc tissue. Thus, healthy disc tissue can be preserved.
- In closed herniated disc surgery, there is a continuous flow of fluid at the surgical site for imaging. This fluid flow ensures that the area is continuously washed and reduces the risk of infection.
- Since it can be applied with local anesthesia, the patient is protected from the risks of general anesthesia.
- Nerve roots are not pulled aside as in open surgery. For this reason, nerve root damage, which can occur due to stretching in open surgeries, is less common in closed herniated disc surgeries.
- Once the learning curve of the surgical team is complete, the procedure can be completed in a shorter time compared to open surgery.
Conclusion
In herniated disc surgery, endoscopic discectomy, i.e. closed herniated disc surgery, is as successful a technique as microdiscectomy surgery. The risk of scar tissue formation after closed herniated disc surgery is also lower. Since the spinal structure is preserved with the endoscopic discectomy technique, patients recover more easily after closed herniated disc surgery.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Joint Prosthesis Surgery

It is the surgical treatment of disorders and other joint diseases caused by injury or strain of the joints, which play an important role in the movement of the human body. The most common reason for prosthesis surgeries is joint calcification that cannot be adequately treated with other treatments. In joint prosthesis surgeries, the worn and damaged surfaces of the joint, which are calcified and unable to function as a result of various traumas, diseases and disorders, are removed and replaced with artificial joint parts. In joint prosthesis surgery, methods such as partial prosthesis or complete prosthesis can be applied depending on the situation.
The most common prosthesis surgeries are knee, hip and shoulder joints. The most common reason for full knee replacement surgery is unresponsive knee joint calcification.
Nowadays, a new era has started in this branch of surgery with personalized kinematic prosthesis surgery, robotic joint prosthesis surgery and newly developed long-lasting prosthesis designs, which have started to be used especially in knee prosthesis surgeries.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Knee Replacement

The knee joint is one of the largest joints in our body and has the widest range of motion. Thanks to the hinge-like mobility of the knee, it allows the knee to bend and unbend straight. The knee is actually formed by two joints coming together. These joints are the tibiofemoral (between the tibia and the thigh bone) and the patellofemoral (between the kneecap and the thigh bone). Loading on the articular surface is absorbed by the cartilage covering the articular surface, especially the meniscus and ligaments.
The contact surfaces of the knee during its movements are covered with a flat, smooth and slippery surface called articular cartilage. This provides a slippery and low-friction surface. Thus, during knee movements, movement occurs painlessly and without friction between the bones.
There are two menisci in the knee, the inner and outer meniscus. These C-shaped cartilaginous cushion-like menisci protect the cartilaginous structure as it slides over each other during movement. These structures also act as shock absorbers, distributing the load over the entire knee joint. Thus, impacts that could cause point damage are spread in such a way that they do not cause damage to the joint.
Ligaments are strong connective tissue fibers that connect the bones together. They allow you to move smoothly and painlessly when walking, bending and straightening your knee. Wear and tear of the articular cartilage can lead to tearing of the meniscus and damage to the ligaments, which can lead to knee instability. This causes pain and loss of function.
The knee joint is surrounded by a layer of soft tissue called the capsule and contains joint fluid. This fluid, known as synovial fluid, is produced by a thin membrane inside the joint capsule called the synovium. The synovial fluid lubricates the joint and nourishes the cartilage and connective tissues within the joint capsule.
Osteoarthritis is also known as "osteoarthritis", "degenerative arthritis", "arthrosis" or "osteoarthritis". Osteoarthritis may be the result of wear and tear on the articular cartilage over time with aging, but it may also be associated with a genetic predisposition. The loss of cartilage causes the bones to rub against each other. The content of the synovial fluid in the joint begins to change and deteriorate. When there is advanced calcification, small protrusions (osteophytes) form on the bone corners facing the joint. As a result of calcification, patients complain of knee pain, stiffness, loss of movement, deformity, limping, difficulty walking and squatting.
Knee arthritis can be diagnosed after the evaluation, physical examination and radiographs of the patient who applies to the outpatient clinic with the complaint of knee pain. X-rays may show narrowing of the joint space, bone loss and cysts due to friction and abrasion in the bones in cases where the space between the bone structures that make up the joint is completely lost, and in more advanced stages, bone loss and cysts can be seen.
The Oxford Knee Score test is performed to assess the degree and function of knee arthritis. This score is used to understand the severity of arthritis in the knee. It can also be used to measure recovery after knee surgery. Patients with knee pain are asked 12 questions that assess their function in daily life. A score of 48 is a normal knee score. Patients with an Oxford Knee Score of 25 or less are usually recommended for total knee replacement surgery.
When is knee joint replacement surgery performed?
The aim of knee replacement is to improve the patient’s daily life functions. When arthritis progresses, it is difficult to walk short distances, shop, get in and out of the car, walk up and down stairs, and do gardening. If complaints persist despite the use of painkillers and anti-inflammatory drugs, weight loss, physical therapy, injections into the knee, knee braces or canes, knee replacement surgery is required.
Knee replacement surgery
Knee replacement surgery is a surgery performed by restoring the joint surfaces of the bones with implants suitable for the actual anatomy. Knee replacement is mostly applied in the treatment of advanced knee arthritis.
Knee replacement was first tried in the 1960s and tested with different surgical techniques and implants. Today, it is applied as a successful and reproducible procedure using up-to-date technological tools. Knee replacement is a safe and successful treatment for patients with arthritis in the knee that does not respond to conservative treatments, to improve physical function and for a painless knee joint.
Which materials are used in knee replacement?
The type of prosthesis and materials to be used in knee replacement are selected according to the patient. Prosthesis components are usually made of titanium or metal produced from chromium-cobalt alloys.
The prosthesis is fixed to the bone with a special filling material called cement or by allowing the porous structure of the prosthesis to integrate with the natural bone. A plastic spacer made of polyethylene is placed between the tibial and femoral implant surfaces of the knee joint.
Most femoral components are made of metal alloys (cobalt chromium) or metal-ceramic alloys (oxidized zirconium). The patellar component and the tibial insert component are polyethylene plastic. The tibial component is made of cobalt chromium (metal alloy), titanium (metal alloy) and polyethylene.
Types of knee replacement
There are two basic types of knee prosthesis in general use. These are partial (unicondylar) and complete knee replacement. The choice of prosthesis type is determined according to the area and severity of the joint calcification. The aim of both types of prosthesis is similar. It is to replace damaged cartilage and bone surfaces with new surfaces that can slide freely on each other to restore movement and function to the joint.
Both types of prosthesis have metal parts in contact with the bones and a polyethylene plastic interface placed between the two parts. There is no mechanical connection between the parts. Therefore, some of the natural ligaments in the knee must be intact to ensure joint stability.
The tibiofemoral joint (the joint between the femur and tibia) has two articulating surfaces, one on the inside and one on the outside. In partial knee replacement, only one of these articulating surfaces is replaced, whereas in total knee replacement, both articulating surfaces are replaced. Patients who undergo partial knee replacement have better range of motion and better joint sensation. Another type of prosthesis, the patellofemoral joint replacement between the kneecap and thigh, is designed to replace the articular surfaces between the kneecap and the femoral trochlear groove. The back surface of the kneecap is covered with polymer plastic, while the groove area in the femur is replaced with metal.
How is a total knee replacement surgery performed?
The knee joint is accessed after a skin incision of approximately 15 cm in front of the knee joint. Small bony protrusions on the bone edges are removed. Then the anterior cruciate ligament, internal and external menisci and in some cases the posterior cruciate ligament are cut and removed. With the special tools in the sets of the prosthesis to be used, bone incisions are made from the upper part of the tibia and the lower parts of the femur with a chainsaw and worn cartilage and bones are removed. After this process, the trial implants of the prosthesis to be used are placed and the movements, balance and alignment of the knee joint are evaluated.
After this stage, the appropriate prosthesis parts are attached to the bone surfaces with the cement used for this surgery. A polyethylene plastic piece is placed between the metal prosthetic surfaces to allow the cement to freeze and adhere to the bone. Afterwards, the joint capsule is repaired and the skin tissue is closed. Total knee replacement surgery usually takes around 40 minutes.
Recovery after knee replacement surgery
Rehabilitation for knee replacement starts within 24 hours after surgery. The physiotherapist starts a program of appropriate exercises to increase knee movements, strengthen the muscles and prevent circulation and clotting problems very soon after the operation.
Patients start walking with a cane, walker or crutches within the first 24 hours after surgery. Walking distance and frequency increase over time. Patients are usually able to drive a car 2-4 weeks after surgery and can return to their normal activities 6 weeks after surgery. Full recovery and return to full strength and mobility may take up to 4 months. Usually one month after surgery, patients are much more mobile than they were before knee replacement surgery.
In 90% of patients, the knee prosthesis is expected to function without problems for an average of 20 years. However, prostheses do not last forever, they have a lifespan. After 20 years, general wear and tear can loosen the prosthesis.
Risks and complications of knee replacement
DVT (deep vein thrombosis): DVT is a blood clot, usually in the veins of the legs. The blood clot can break away from the vein and attach to the veins in the lungs. This is called pulmonary embolism. Pulmonary embolism is a serious complication and can cause sudden shortness of breath, general deterioration or, very rarely, death.
The following measures should be taken to prevent deep vein thrombosis:
- After the operation, you will be given light ankle and toe exercises. These exercises help your blood circulation to be more regular.
- The use of pneumatic devices to prevent thromboembolism after surgery passively helps blood circulation.
- After surgery, the use of blood thinners every day has a protective effect.
Infection Infection is a rare but serious complication with an incidence of 0.5 to 1% after knee replacement surgery. The risk of infection can be reduced with the use of antibiotics and necessary sterilization measures, but these measures cannot completely eliminate the risk.
Tourniquet pain This is a transient and rare complication of a tourniquet applied to the thigh. Numbness, stiffness and pain may occur with prolonged tourniquet application.
Nerve damage: Damage to the nerves around the knee area may occur. The most common causes of nerve injuries may be due to the instruments used during surgery and nerve compression and direct damage, as well as prolonged tourniquet use. Tourniquets are used during surgery to allow the surgeon to see the surgical field and to minimize blood loss. The nerve damage usually causes a temporary loss of sensation. It completely resolves within 2-3 months and does not cause loss of function.
Wear and loosening of the prosthesis: Due to the friction between the prosthesis parts over time, there may be wear and tear in the prosthesis parts, especially in the polyethylene plastic part, and loosening between the interface with the bone in the metal parts.
Conclusion
Knee replacement is a low-risk, successful and safe surgery performed on patients who experience pain, difficulty in walking and limitations in activities of daily living due to arthritis in the knee joint. Knee replacement is expected to function without problems for an average of 20 years in 90% of patients.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Partial Knee Replacement

Knee joint structure
The knee joint is one of the largest joints in the body, made up of three bones. The main structures that make up the knee joint are the thigh (femur), shin (tibia) and kneecap (patella) bones. The femur and shin bone form two articular surfaces, the inner side and the outer side (tibiofemoral joint). Osteoarthritis of the knee joint usually starts on the surface on the inner side of this joint. Another joint is formed between the thigh bone and the kneecap (patellofemoral joint).
In a healthy knee joint, the bones facing each other are covered with cartilage tissue. The cartilage tissue forms a smooth surface that allows the bones that make up the joint to move freely.
Knee joint arthritis
Due to aging, previous knee fractures, obesity, professions where repetitive knee movements are performed and genetic reasons, wear of cartilage tissue may occur and the calcification process may begin. As the cartilage thickness decreases, pain during knee joint movements and difficulty in walking begin. In addition to cartilage wear over time, deterioration in the bone tissue under the cartilage tissue and the formation of sharp protrusions in the joint cause restriction of knee movements. In the early stages of osteoarthritis, methods such as medication, physical therapy, exercise and intra-articular injections can be applied.
Restricting daily activities such as kneeling and rising, climbing up and down stairs, and cycling can also reduce symptoms. In cases where osteoarthritis progresses, no response can be obtained to the treatment methods mentioned above. In this case, surgical treatment comes to the agenda. In knee arthritis, these three joint surfaces are not always affected to the same degree.
In the Turkish population, arthritis, which is usually seen on the inner side of the tibiofemoral joint between the thigh and shin bones, both starts earlier and progresses more severely.
For this reason, sometimes arthritis in the inner or outer tibiofemoral joint area of the knee is so advanced that prosthesis is required, while other parts of the joint may not be affected. In such cases, the aim should be to preserve the intact cartilage tissue and intervene only in the part of the joint with significant arthritis.
How and when is partial knee replacement surgery performed?
If the arthritis in the knee joint does not affect the entire joint, but is limited to only a part of it, a so-called partial knee replacement surgery is appropriate. In this method, the entire knee joint is not replaced. Partial prosthesis surgery can be performed on one or two of the inner side, outer side and back of the kneecap joint parts of the knee. Thus, the patient is offered an alternative option to a full knee replacement.
If it is performed only on the inner or outer lateral joint side, it is called unicondylar partial knee replacement. In addition, if it is also applied to the back of the kneecap, it is called bicondylar partial knee replacement. In partial knee replacement surgery, the cruciate ligaments are preserved, less bone is removed and smaller incisions are made.
With partial knee replacement, only the part of the joint affected by arthritis is operated on and only the joint surface on that side is replaced. Since the surgical area is more limited, the surgical incision is smaller, there is less blood loss, the risk of infection is reduced and recovery is faster.
In the last 15 years, with advances in technology and surgical techniques, partial knee replacement has become a more widely available option for selected patients. Approximately 10-15% of patients with knee arthritis are suitable for partial knee replacement.
Who is not suitable for partial knee replacement?
Partial knee replacement is not suitable for every patient. Choosing the right patient for unicondylar knee replacement is considered one of the most important steps in terms of achieving a good functional result and the life of the prosthesis. Partial knee prosthesis is not recommended in cases such as overweight, calcification spread throughout the joint, advanced deformity (braces leg or bow leg), very limited joint movements, joint calcification caused by rheumatic joint disease and obesity. Although there is no significant restriction on patient age, it is generally preferred in patients over 40 years of age.
Patellofemoral knee replacement
The patellofemoral joint is a joint between the patella (kneecap) and the femur, the thigh bone, with the patellar articular surface. During knee bending and unbending movements, the kneecap slides over the groove of the femur. Excessive patellofemoral friction caused by malalignment of the kneecap or fractures and dislocations of the kneecap can lead to severe cartilage loss on these joint surfaces. Due to calcification that develops after cartilage loss, it causes complaints such as pain, burning and noise in the kneecap area, especially in movements such as knee bending, squatting and going up and down stairs.
Patients with calcification in the patellofemoral joint part of the knee achieve good results after medication, intra-articular injections, exercise and physical therapy, along with changes in their habits. If the complaints persist despite these treatments and the patient’s life is significantly affected, partial knee replacement surgery called patellofemoral prosthesis is recommended.
Patellofemoral knee prosthesis, which was first introduced in the 1970s, did not achieve the desired results due to the lack of suitable implants and technical difficulties. However, nowadays, thanks to advances in implant design and materials, as well as advances in partial knee replacement surgical techniques, good results are obtained as in total knee replacement surgery. In patellofemoral joint replacement surgery, the damaged cartilage behind the kneecap and on the articular surface of the femur is removed. A polyethylene plastic button-shaped implant is inserted into the patella, while a thin metal piece is inserted into the femoral groove. In this way, the patellofemoral joint is restored without friction and pain, and the joint is restored.
Conclusion
If the arthritis in the knee joint does not affect the entire joint, but is limited to a part of it, partial knee replacement is appropriate. This method preserves the healthy surfaces of the joint as the entire knee joint does not need to be replaced. Partial prosthesis surgery can be performed on one or both of the inner lateral, outer lateral and posterior patella joint parts of the knee. The most appropriate method for you will be determined by your orthopedic surgeon together with your examination findings and radiological examinations.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Knee Prosthesis Revision

Knee prosthesis revision is a prosthesis replacement surgery performed in patients who have had knee prosthesis surgery before. In this surgery, known as “reoperation”, the prosthesis is removed and a new prosthesis is inserted.
In some cases, it may be necessary and sufficient to replace a part of the prosthesis in the joint, while sometimes it may be necessary to completely replace all prosthesis parts. It is an operation that requires detailed preoperative planning, special prosthesis sets and materials, experience and a longer operation and recovery period compared to the first prosthesis.
Who needs knee replacement revision surgery?
90% of patients who undergo total knee replacement use the prosthesis for about 20 years without any problems. When the functions of the knee joint deteriorate due to wear, loosening and inflammation of the prosthesis parts; difficulty in walking and pain in the knee begin. Patients who undergo knee replacement at an advanced age can use their prosthesis for a lifetime without any problems.
At younger ages and especially in those who maintain an active lifestyle, the knee prosthesis may wear out over time and its function may deteriorate. However, today, with newly developed high-tech prostheses and applications such as kinematic surgical technique and robot-assisted knee prosthesis surgery, prosthesis life can be extended in young and active people.
What are the most common reasons for knee prosthesis revision surgery?
Infection: It is a potential complication that can be seen after knee replacement as in other surgeries. It can occur while in the hospital, after going home and even years later. The risk of infection after knee replacement surgery is less than 1%. If infection develops, loosening of the prosthesis may follow. Patients in this situation have complaints such as knee pain, swelling, redness, increased temperature and sometimes discharge.
When the infection is detected early, treatment with washing, surgical cleaning (debridement), replacement of the plastic spacer by leaving the metal parts in place is sufficient. However, in case of late-onset or late-detected infections, a 2-stage revision surgery is performed. In the first stage, the prosthesis is removed, the joint is cleaned and washed and a cement filling with antibiotics is placed in the joint. After a few months of antibiotic treatment, when it is determined that the infection situation has improved, the second stage is started and a new knee prosthesis surgery is performed.
Gaps and instability in the knee: Over time, the function of the ligaments that support and stabilize the knee joint may deteriorate as a result of wear and tear on the knee prosthesis. The function of the knee is impaired because the ligament balance required when standing, moving the knee or walking is disrupted. In this case, revision surgery is performed to replace the worn prosthetic part or parts in the knee.
Stiffness Sometimes, after knee replacement surgery, a limitation in the range of motion required to perform daily activities may develop. It may be caused by excessive healing tissue that forms around the joint during the healing period. In the early period, “manipulation under anesthesia” is performed to open the joint movements.
You will be given anesthesia so that you do not feel pain during this procedure. The doctor bends your knee to open the adhesions. In most cases, this procedure is successful in improving range of motion. However, sometimes the knee remains stiff. If extensive scar tissue or the position of components in your knee limits your range of motion, revision surgery may be required.
Wear and loosening: Over time, friction between the prosthetic components can cause wear and tear, loosening and fracture of the prosthetic components. For a knee prosthesis to be functional, the prosthesis must be firmly attached to the bone. Cement is often used for this. However, over time, if the bone attachment of the prosthesis weakens, the prosthesis may loosen and the knee may become painful.
The causes of loosening are not always clear. Factors that can cause loosening include activities that strain the knee joint, knee replacement in people who were active at an early age, overweight and wear of the plastic spacer between the two metal components of the prosthesis.
Due to the wear of the plastic spacer called the insert, small particles accumulate in the joint and the body’s immune system develops a reaction against them. This reaction causes bone destruction called osteolysis in the healthy bone around the prosthesis. With osteolysis, the bone that supports the prosthesis is destroyed and the prosthesis bone attachment weakens and the prosthesis loosens. After loosening, the balance of the knee is disturbed and causes pain. In such a case, knee prosthesis revision surgery is required.
Fractures around the prosthesis; These fractures are fractures in the bone around the components of the knee prosthesis. These fractures are often the result of a fall and usually require knee prosthesis revision surgery. In order to decide what to do in revision surgery, factors such as the quality of the bone, the type and location of the fracture, and whether the prosthesis is loose or not should be evaluated.
Examinations before knee prosthesis revision surgery
Some laboratory tests and radiologic imaging tests are used to learn more about the condition of the knee.
X-rays are the first test requested to evaluate the condition of the prosthesis and the bone structure. Bone scintigraphy, one of the other imaging tests, can help determine whether the prosthesis has loosened when there is no clear evidence of loosening on the X-ray. Bone scintigraphy can also provide information on whether the loosening is due to infection or wear and tear. Computed tomography (CT) is another imaging method used to better reveal the bone structure and to examine it in 3D.
Laboratory tests; blood tests are requested to determine whether there is an infection. In addition, in cases of loosening of the knee and prosthesis, a fluid sample taken from the joint may need to be examined to differentiate the infection. Various laboratory analyzes are performed to determine whether there is infection in the fluid taken from the joint using a syringe.
How is knee revision surgery performed?
Knee replacement revision surgery is more complex and takes longer than the first knee replacement. While the first knee prosthesis surgery takes around 40 minutes, prosthesis revision surgery can take 1-2 hours. In knee prosthesis revision surgery; the joint is accessed from where the scar from the previous knee surgery was. The presence of infection is re-evaluated. All metal and plastic parts of the prosthesis are evaluated to determine which parts of the prosthesis are worn, loose or dislocated. The prosthetic parts are carefully removed to protect the bone. If a cemented prosthesis was previously used, the cement residue is removed. After this stage, the bone surfaces are prepared for the revision prosthesis.
In some cases, significant bone loss may have occurred. If this is the case, metal reinforcements and platform blocks can be added to the main components of the prosthesis to compensate for this. After these procedures, the knee revision implant is cemented into the bone and anchored. The joint capsule is then repaired and a drain is placed to drain blood and fluid from the joint and soft-closed.
Risks and complications of knee replacement
As with any surgery, there are some risks involved in knee replacement revision surgery. Since it is longer and more complex than the initial knee replacement, the risk of complications is also higher. Possible risks and complications in knee prosthesis revision; wound dehiscence,
Infection, bleeding, limitation of movement and stiffness, bone fracture, nerve or vessel damage, clot formation in the vessel, pulmonary embolism can be listed.
After knee prosthesis revision surgery, the majority of patients regain their functions with a painless and stable knee joint. However, it may not always be possible for the pain to completely disappear and the knee joint to regain its former mobility.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Joint Replacement Surgery

Hip joint structure
The hip joint consists of a head and a socket. The head of the thigh bone, the upper end of the femur, is also called the femoral head. The socket, called the acetabulum, is part of the pelvis, the pelvic bone. The femoral head rotates in the socket like a ball, allowing the leg to move forward, backward and sideways. In the hip joint, the cartilage tissue covering the articular surface of the femoral head and acetabulum allows the joint to move freely. In a normal healthy hip, the cartilage tissue covering the head and the socket ensures that the joint surfaces are smooth and slippery. Thanks to the cartilage tissue, which can be seen as the space between the head and the socket on hip x-rays, it allows the joint to slide easily with even less resistance than ice sliding on ice.
The labrum surrounds the outer edge of the acetabulum, which forms the socket of the hip joint, like a gasket, holding the femoral head in place. The labrum consists of a special layered cartilaginous structure. This structure ensures that the hip joint is stable during a wide range of motion. The hip joint is a multi-axial joint and has a wide range of motion. The wide range of motion makes it possible to perform daily activities such as walking, running, sitting, sitting cross-legged and leg extension.
What is hip joint arthritis?
When the cartilage structure deteriorates or is damaged, the comfortable sliding mobility in the joint is also impaired. The cartilage wears and the friction between the surfaces increases. As a result, the area of wear on the cartilage widens and deepens. Over time, the cartilage tissue covering the bones that make up the hip joint disappears, and bone begins to rub against bone. The smooth ball-like shape of the femoral head also deteriorates and it starts to rotate uncomfortably in the socket. Thus, the leg’s inward and outward rotation movements are restricted at first, and over time, other movements become difficult.
When calcification occurs in the hip joint due to the wear of the cartilage covering the surface of the bones forming the hip joint, pain in the hip and limitation in movements develop.
People with hip osteoarthritis have difficulty walking, sitting on and off a chair, and squatting. Patients who previously walked with a slight limp start to limp significantly with the weakening of the muscles around the hip.
How is hip joint arthritis diagnosed?
When hip arthritis is suspected, hip movements are evaluated during the examination. In addition, movements such as walking, sitting, standing and squatting are evaluated. X-rays and, if necessary, blood tests are taken to detect the problem in the hip joint. In addition, hip joint ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI) may be ordered depending on the situation. In order to differentiate pain radiating from the lower back to the hip, the lumbar region may also need to be evaluated and additional tests may be required.
What are the treatment options for hip arthritis?
Weight loss: During daily movements, the hip is loaded approximately 3 times the body weight. If this load is reduced by losing weight, the pain also decreases. As a result of the reduced load on the hip, wear and tear on the joint will also decrease and the progression of arthritis will slow down.
Activity control: Avoiding activities that cause hip pain as much as possible will reduce pain. Workplaces of those who work in jobs that require squatting or bending the hip excessively should be adjusted.
Physical therapy: Helps to reduce hip joint pain and increase movement and muscle strength.
Strengthening the muscles around the hip:
Maintaining and strengthening the flexibility of the muscles around the hip is important for comfortable daily life activities. Hip exercises to be performed within the framework of the program recommended by the physiotherapist help the person to walk more comfortably by increasing joint mobility.
The best activities for hip arthritis are exercises in the pool and swimming.
Intra-articular injection: In hip arthritis, orthobiologic injections such as pain and inflammation relieving cortisone or regenerative platelet rich plasma (TZP, PRP), stem cells can be applied into the joint under ultrasound guidance.
Drug treatment: Various pain medications can be used to reduce pain in line with the doctor’s recommendation.
Using an assistive walking device: The load on the hip can be reduced by using a cane or a cane with a brace. Patients with hip arthritis should take the cane in the hand on the side of the healthy hip. For example, if you have arthritis in your right hip, the cane should be in your left hand. This will help you walk more painlessly and smoothly.
When should hip joint replacement surgery be performed?
Not every patient with hip arthritis may need hip replacement surgery. The pain can be reduced and controlled with the measures and treatments mentioned above. However, despite the precautions taken and painkillers used, hip replacement surgery is required in patients with widespread and significant calcification in the joint who have pain in the hip during daily work and activities, difficulty in walking, limping or night pain.
The most common reason for hip replacement surgery is hip joint arthritis, but it can also be performed in hip bone fractures, hip dislocation-related arthritis or in some other cases.
What is hip joint replacement?
Hip prosthesis surgery relieves pain and restriction of movement in people with hip joint arthritis and restores mobility to the hip joint.
There are three different types of hip replacement;
- Total hip replacement (most common)
- Partial hip replacement
- Hip joint surface replacement
The most common hip replacement surgery is a total hip replacement. With a total hip replacement surgery, artificial implants are placed in the socket (acetabulum) and femoral head, which are damaged due to calcification in the hip. The damaged femoral head is cut out and replaced with a stem implant made of a metal alloy and a ball-shaped head made of ceramic, cobalt chrome or oxinium. Oxinium is known to be the most durable metal alloy ever used. The implant placed in the socket consists of a polyethylene plastic implant or ceramic implant surface placed on a titanium metal implant.
The other two types of hip replacement surgery are usually performed for patients of certain age groups and activity levels. The difference between partial hip replacement and full hip replacement is that only the femoral head of the hip joint is replaced, while the socket is not intervened. It is a hip replacement surgery usually performed in elderly patients with hip fractures. Hip prosthesis surgeries, in which only the surfaces of the femoral head and the socket section are replaced, are prosthesis surgeries that are applied in young and active patients and save time before full hip replacement.
Recovery after hip joint replacement surgery
Most patients who undergo hip replacement surgery start walking the day after surgery with a walker or cane with bracelets. Sitting, getting up, getting in and out of bed, walking using a walker and climbing stairs are practiced. Patients who can perform these movements in a balanced manner are given a home exercise program and are discharged from the hospital if they are in good general health.
What should be considered after hip joint replacement surgery?
In the first 3 months after total hip replacement surgery, the following precautions are very important. These measures will both accelerate recovery after hip surgery and reduce the risk of the prosthesis coming out of its socket.
- Do not sit on a low chair, sofa or toilet.
- Use high chairs and high toilet seats.
- Use a pillow for support in the car seat.
- Do not sit cross-legged or cross your legs.
- When sitting, always keep your knees lower than your hips.
- Do not bend your leg more than 90 degrees from the hip.
- Place a pillow between your legs when lying on your side.
When can I return to normal life and work after hip replacement surgery?
The age, occupation, other diseases (such as diabetes, cardiovascular disease, obesity), habits and the condition of the joint determine how long it takes to return to normal movements. Based on these criteria, the orthopedic surgeon determines when you can safely return to normal activities. Usually this can vary from 4 weeks to 4 months.
Recovery after surgery will take several months. Strenuous movements in the early period can negatively affect the healing process. Since the peripheral muscle strength has weakened over the years due to hip arthritis, this affects patients’ compliance with exercises, endurance and balanced walking in the postoperative period.
Walking: If your walking is not stable, you can continue to use your cane. The cane will help you walk without limping until your muscle strength improves.
Sportive activities: Activities such as brisk walking, dancing, swimming can usually be started about 2 months after surgery. However, it is important to consult your orthopedic doctor before starting your activities.
Driving a car: You can start driving 4-8 weeks after right hip replacement surgery. In left hip replacement surgery, you can start driving a car with automatic transmission earlier with the permission of your orthopedic doctor.
What are the risks associated with hip joint replacement surgery?
As with all major surgeries, total hip replacement surgery has some risks and possible complications. Necessary precautions are taken before and after surgery to prevent these risks and complications.
Although rare, complications that may occur include; side effects of anesthesia, blood loss requiring blood transfusion, vascular and nerve injury, deep vein thrombosis and pulmonary embolism, infection, fractures around the prosthesis, dislocation of the prosthesis, leg length difference, loosening of the prosthesis.
Does a hip joint prosthesis have a lifespan?
Studies show that 95% of patients who undergo hip replacement surgery are in very good functional condition 10 years after surgery. After 20 years, the success rate is between 80% and 85%. The durability of new surface materials and cementless prostheses, which have been developed and produced in recent years, is even longer.
Conclusion
Pain and limited mobility caused by hip arthritis are not your fate. The success rate after total hip replacement surgery is high. More than 90% of people who undergo hip replacement surgery for hip arthritis live the rest of their lives pain-free and comfortable.
Unassisted walking after hip replacement surgery significantly improves the quality of life of patients.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Prosthesis Revision

What is hip replacement revision?
After total hip replacement surgery, most patients continue to use this prosthesis for the rest of their lives and do not experience any problems. After wear and loosening of the prosthesis parts placed in the hip joint due to mechanical or biological reasons, their function may deteriorate. In order to restore the hip joint and make it functional again, the surgical procedure to replace part or all of the prosthesis is called hip replacement revision surgery.
The rate of patients who need revision hip replacement after their first hip replacement surgery is around 20%.
The most common reasons for hip prosthesis revision;
1- Recurrent dislocation of the hip prosthesis
2- Mechanical problems (implant wear – loosening or fracture)
3- Infection in the joint
Recurrent hip prosthesis dislocation
The structure of the hip replacement parts is similar to the natural hip (a ball and socket). For the hip prosthesis to work well, the ball (femoral head) must always remain inside the socket (acetabulum). Two main factors keep the femoral head inside the socket in the hip;
- Positioning the femoral head of the hip in the socket at the appropriate orientation and angle,
- To maintain the relationship between the head and the socket, it needs to be supported by strong muscles and ligaments around the hip joint.
The hip replacement is designed to have a wide range of motion. However, trauma or certain hip positions can force the hip head out of the socket. This condition is called hip prosthesis dislocation.
Hip prosthesis dislocation is very rare in patients who follow the advice given by your orthopedic doctor and are in good general health. However, the risk of dislocation is higher in elderly patients with weak muscles, debilitated patients, patients who have hip replacement after a hip fracture or multiple hip surgeries. Especially in cases where important muscles and tendons around the hip joint are damaged, recurrent dislocations may occur. Before the revision surgery to prevent recurrent dislocation, X-rays and computed tomography examinations are performed to evaluate the possible causes of dislocation and the condition of the hip prosthesis.
In hip replacement revision surgery, it may be necessary to replace all or part of the prosthesis. Especially in new types of hip revision prosthesis developed to prevent recurrent dislocation, the dual joint structure between the prosthesis head and the socket prevents the prosthesis head from coming out of the socket. In some cases, dislocations are prevented by attaching a clamp that prevents the head from dislocating inside the hip socket. Proper healing of the soft tissues around the hip after surgery is very important for the success of the operation. For this reason, it may be necessary to use a corset for a few weeks after surgery. After surgery, patients should follow the recommendations of the orthopedic doctor and avoid putting the hip in positions that may cause a new dislocation.
Mechanical problems of the hip prosthesis (wear, loosening, fracture)
The parts of the hip prosthesis that move against each other will gradually wear out during regular use of the prosthesis. The younger and more physically active the patient, the faster the wear. Depending on the type of prosthesis used, plastic (polyethylene), cement, ceramic or metal wear particles are produced after continuous and repetitive friction.
The patient’s immune system recognizes these wear particles as foreign (as they are not a natural part of the body) and creates an immune response similar to an allergic reaction. This immune response causes bone damage and destruction called osteolysis. Osteolysis weakens the bone support surrounding the prosthesis and causes loosening of the prosthesis.
After loosening of the prosthesis, the attachment of the prosthesis to the bone weakens and the position of the prosthesis shifts. Abnormal loads on the displaced prosthesis parts may cause pathological fractures in the weakened bone.
Mechanical wear and tear leading to loosening of prosthetic parts are the most common mechanical problems. However, a fall or similar trauma can cause fractures in the prosthetic parts. In patients who are scheduled for revision surgery due to wear, mechanical loosening or fracture, the worn, loosened or fractured prosthetic parts are removed and new prosthetic parts are inserted. If there is loss of the bone to which the prosthesis is attached and supported, it is necessary to use bone grafts taken from the patient or ready-made bone grafts. In some cases, the surgeon may ask the patient not to put full weight on the operated leg for the period required for the prosthesis to hold on to the bone.
Hip replacement infection
Infection can occur at any time after surgery. The risk is higher in the first six weeks after surgery. After this time, the risk of infection is lower. Sometimes prosthesis infections can occur in mouth, teeth and gums, lung, urine and skin infections as a result of germs (bacteria) being carried to the prosthesis site through the blood. Symptoms of infection include pain, fog, discharge, increased temperature and redness in the hip. However, it is sometimes necessary to suspect the presence of an infection even in the presence of pain and further blood tests and laboratory examination of the fluid sample taken from the joint should be performed.
It is important to identify the bacteria that cause prosthesis infections. For this purpose, a fluid sample is taken from the hip joint and laboratory examination is performed. If infection is detected after the examination, antibiotic treatment is started by determining the type of bacteria and the drugs to which the bacteria are sensitive.
Sometimes the bacteria may be resistant to antibiotics or there may be multiple bacterial infections. In these cases, bacteriophage therapy can be used to achieve successful results in resistant joint infections. Bacteriophages eliminate only the bacteria to which they are sensitive, while they do not harm human cells at all.
Treatment of hip prosthesis infections
When a hip prosthesis infection is diagnosed, the type of causative bacteria is decided according to its antibiotic sensitivity, the time of infection (early or late), the type of prosthesis used and the patient’s general health. Your doctor will inform the patient about the benefits and drawbacks of each treatment option and the process.
- Surgical cleaning of the inside of the joint (debridement), removal of sediment and particles inside the joint, washing of the joint and antibiotic treatment; It is applied when diagnosed within 3 weeks after the onset of symptoms. After surgery, antibiotic treatment is given in the form of injections for 3-6 weeks in accordance with the causative bacteria and then treatment is regulated with low-dose antibiotic pills for a long time.
- Two-stage revision surgery: If more than 3 weeks have elapsed since the onset of symptoms and the causative bacteria cannot be identified, in the first stage, the prosthesis fragments are removed, the bone and soft tissues are cleaned, and the space between them is temporarily filled with a cement cavity sealant with antibiotic added. This is usually followed by a 6-week antibiotic treatment. In the second stage (usually 10-12 weeks after the first stage), the gap-closing material is removed and a new revision prosthesis is placed after surgical cleaning. After this second stage, antibiotic treatment is continued for some time.
- One-stage revision surgery; If diagnosed within 3 weeks after the onset of symptoms, if the causative bacteria can be identified, in special cases where extensive debridement and washing can be performed, a one-stage revision is performed, the prosthesis is removed, the bone is cleaned and a new prosthesis is placed. Antibiotic treatment is then continued for 6-8 weeks.
What should be considered to reduce the risk of hip replacement revision?
Some of these can be prevented by being aware of the possible risks after hip replacement, such as infection and mechanical problems. Dislocations can be prevented by following the doctor’s advice and recommendations.
Some types of prosthesis infection can be prevented by early treatment when there is an infection anywhere in the body. Natural wear and tear of the prosthesis usually does not cause pain or discomfort. For this reason, it is very important to have regular check-ups after hip replacement. Physical examination and radiographs should be performed at specified intervals.
Things to keep in mind before hip replacement revision surgery
During revision surgery, it may be necessary to replace one or more parts of the hip prosthesis. The replacement of the loosened part of the prosthesis can be safely performed without bone damage or loss. However, if the part of the prosthesis that is well attached to the bone needs to be replaced, there is usually some bone loss. In addition, some of the muscles around the hip will be damaged, which will affect the strength of the hip and the patient’s hip function. The results of hip revision surgery are not as predictable as the results of the initial hip replacement. Complications may occur more frequently.
Hip revision surgery is technically more difficult than the first hip replacement surgery. It should not be seen or compared to “changing the tires on a car”. The results of the surgery and the durability of the prosthesis are less predictable than the first surgery. Every revision surgery involves some loss of muscle, bone or both. The operation time is usually longer and the risk of complications is higher than with the first operation.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Fracture Surgery

Fractures are the most common condition encountered in emergency admissions to the Department of Orthopedics and Traumatology. Fractures usually occur due to traumas such as traffic accidents, falls and blows. However, in people with osteoporosis, i.e. bone resorption, bone tumors or similar diseases that reduce bone strength, spontaneous fractures can be seen even without a serious impact. Bone fractures can be open or closed, sometimes accompanied by injury to vessels, nerves or internal organs, and can be life-threatening. Soft tissue, ligament, muscle, cartilage injuries or joint dislocation may also be seen in the fractured area. Orthopedics and Traumatology specialists perform both closed and open surgical treatment and follow-up of fractures, while also intervening in secondary problems such as nonunion or infection. With the technological and scientific advances in fracture surgery in recent years, fractures can heal more quickly and patients can return to their daily lives in a short time.
- Common fractures in orthopedics;
- Elbow fractures in children
- Hip fractures in the elderly
- Arm and forearm fractures
- Thigh and leg fractures
- Wrist fractures
- Ankle fractures
- Spine fractures
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Pediatric Orthopedics

Pediatric Orthopedics is the department that deals with the diagnosis, non-surgical treatment and surgical treatment of all kinds of bone, muscle, joint, tendon, ligament problems from birth to infancy, childhood, adolescence and youth. The main difference of pediatric orthopedics from adult orthopedics is that it deals with the treatment of the age group whose bones, muscles and joints are still growing and developing. The response of the child’s musculoskeletal system to injuries and infections is different from the adult body. Biomechanical and deformities of the musculoskeletal system that occur congenitally or during development, traumatic problems caused by falls and accidents are evaluated and followed up by pediatric orthopedic doctors.
- Some of the treatments applied;
- Treatment of fractures and dislocations
- Congenital hand, arm, leg, foot anomalies
- Congenital neck and spine problems
- Ultrasound-guided hip development
- Surgical treatment and follow-up of hip dislocations
- Foot sole analysis and orthotics
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is developmental hip dislocation (hip dysplasia)?

The hip joint is a joint that plays an important role in performing many movements such as standing, sitting, running and squatting thanks to its high mobility. Anatomical structure and harmony are extremely important in a healthy joint.
Developmental hip dislocation is a condition that occurs in infants and young children when the hip joint does not develop properly. The part of the thigh bone called the femur, where it joins the hip, is ball-shaped and forms a joint by sitting in a round socket in the hip bone. This joint is called the ball and socket joint because of its structure. In the case of developmental dislocation of the hip, the femoral head cannot fit firmly in place, so the hip joint harmony is disrupted. This structural defect in the hip joint progresses as the baby grows. The joint can sometimes dislocate completely.
Developmental hip dislocation in infants is one of the most common diseases in pediatric orthopedics. It is a disease that is more common in girls than boys and can lead to serious disabilities if not treated early.
Symptoms of developmental hip dislocation may not appear in newborn babies and young children who are not severely dislocated until they can walk. In cases where the symptoms of developmental dislocation of the hip are not recognized by the family, the dislocation may be recognized by the doctor during routine hip dislocation examinations.
What are the symptoms of developmental hip dislocation?
The symptoms of developmental hip dislocation are as follows:
- Legs that turn outward or appear to be of different lengths,
- Limited range of movement (e.g. legs cannot scissor outwards),
- Unsymmetrical leg and hip folds in unilateral dislocations,
- Delays in motor development, including functions such as sitting, crawling and walking,
- Walking with a limp
- Noise from the hip joint during movement,
- Pain in the hip starting at a young age,
- Early development of arthritis due to joint wear.
Early diagnosis and treatment of developmental hip dislocation is very important. If treatment is delayed, lifelong hip problems may occur.
According to research
- Developmental hip dislocation can affect 1 or both hips, but is more common in the left hip.
- It is more common in girls and first-born children.
- About 1 or 2 out of every 1000 babies have a developmental dislocation of the hip that needs to be treated.
What causes developmental hip dislocation?
The causes of developmental dislocation of the hip in infants are not known, but factors that can cause this condition include
– Low levels of amniotic fluid in the womb,
– Various congenital diseases,
– The mother’s hormones cause laxity in the child’s hip joint,
– Congenital hip dislocation can occur due to reasons such as poor posture of the baby in the womb.
What are the risk factors for developmental hip dislocation?
- It is more common in girls.
- Children with a family history of hip dislocation are more likely to have hip dislocation.
- Neurological causes such as cerebral palsy (cerebral palsy), a condition in which the brain is deprived of oxygen due to birth, or spinal closure defects (spina bifida) also increase the risk of hip dislocation.
- Depending on the position of the baby in the womb, the risk of hip dislocation is higher in babies born breech (breech birth).
- Swaddling a baby who is prone to hip dislocation at birth can lead to hip dislocation.
Early treatment of developmental hip dislocation is very important for the baby’s development and future. Risk factors and symptoms should be evaluated and treatment should be carried out at the earliest possible time.
Treatment of developmental hip dislocation
Early treatment of developmental hip dislocation in the first 6 months of life can be done with the use of a device and some simple precautions. The orthosis (device) prescribed and fitted by the orthopedic doctor keeps the baby’s hips in a fixed position and ensures that development continues normally. As a result of treatment in the first 6 months, the rate of complete recovery is close to 100%.
In treatments performed after the first 6 months, surgical intervention may be required to put the joint in the appropriate position. A plaster cast is applied after the surgical procedure. The hips are then checked again to make sure that the joints are fixed. If developmental dislocation of the hip is not recognized or treated, the hip joints wear out prematurely and early-onset arthritis (joint degeneration) can occur while the person is still in their 20s. Early treatment of developmental dislocation of the hip affects the future.
Can developmental dislocation of the hip be prevented?
- Babies should never be swaddled; if the legs are swaddled, hip development slows down.
- The baby should be dressed in comfortable clothes in which the hip and knee joints can move freely.
- Keeping babies’ legs together during breastfeeding negatively affects hip development.
- From the newborn period onwards, babies should be held in a position that ensures the normal development of their hips. In particular, carrying with a device called a kangaroo is a suitable position for hip development.
According to research;
- Developmental hip dislocation can affect 1 or both hips, but is more common in the left hip.
- It is more common in girls and first-born children.
- About 1 or 2 out of every 1000 babies have a developmental dislocation of the hip that needs to be treated.
Early treatment of developmental dislocation of the hip is very important. Keep in mind that the longer the diagnosis is delayed, the more difficult surgical treatment will be and joint degeneration may develop at an early age.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Clubfoot-pes equinovarus (PEV)

Clubfoot, also known as pes equinovarus (PEV), is a congenital deformity of the foot that occurs in approximately 1 in 1000 live births. The affected foot tends to be smaller than normal, with the heel turning inward and the forefoot turning inward. In cases of clubfoot-PEV, the Achilles tendon is tense and prevents the foot from pulling upwards from the ankle. This position is called the “crop” and it is impossible to place the foot flat on the ground. Since this congenital deformity begins in the womb, the deformity of the foot is usually quite severe after birth and cannot correct itself.
Four classic components of clubfoot-PEV:
Equinus: This is the fixed downward position of the foot from the ankle, and the foot cannot be brought from the ankle to a flat-footed and upward position. This deformity is caused by a strained Achilles tendon.
Varus Inward rotation of the heel
Adduction Inward rotation of the foot giving it a kidney or bean-shaped appearance
Supination: The bottom of the foot pointing inwards and upwards when it should be pointing downwards.
Why do children have clubfoot-PEV?
It is still not clear what causes clubfoot-PEV deformity. The most common type is the so-called idiopathic type, which is of unknown cause. It is widely accepted that many genetic and environmental factors are effective in the development of clubfoot-PEV. As the baby grows in the womb, clubfoot-PEV is caused by abnormal development of muscles, tendons, bones and even veins. Clubfoot-PEV is approximately 2 times more common in boys than in girls. In 50% of cases, this deformity is seen in both feet. If the first child has clubfoot-PEV, the risk of subsequent children having it is 2-5%.
The risk of clubfoot-PEV is higher in association with certain nervous system diseases (cerebral palsy, spina bifida, spina bifida, tethered cord, arthrogryposis), various connective tissue disorders (Larsen syndrome, diastrophic dwarfism) and certain biomechanical conditions (oligohydramnios, tethered bands).
In cases of clubfoot-PEV associated with these diseases or disorders, early surgical correction is often required, as the foot deformity is usually more severe.
How do I know if my child has clubfoot?
Clubfoot-PEV is easily diagnosed during the first examination of the newborn. Clubfoot-PEV can also be detected by prenatal ultrasound in the womb. If clubfoot-PEV is diagnosed before birth, we recommend that you schedule an appointment with the pediatric orthopedic clinic to discuss treatment options after birth.
During the initial examination, a detailed prenatal and birth history and family history will be taken from you. You will also have a full physical examination. It is known that babies born with clubfoot-PEV have a slightly higher risk of developing developmental dysplasia of the hip (DDH). DDH, also known as congenital dislocation of the hip, is a developmental joint disorder in which the normal hip joint is not fully formed because the socket (acetabulum) where the ball-shaped head of the thigh bone (femur) is located is too shallow. For this reason, a detailed hip assessment and hip ultrasound are recommended during the examination for clubfoot-PEV.
Clubfoot-PEV is a deformity that will be permanent if left untreated; it will not resolve spontaneously. The deformity and limitation of movement will continue to worsen over time with secondary bone changes that develop over the years. Uncorrected clubfoot-PEV in a child or adult leads to loss of function and disability. Due to the abnormal development and deformity of the foot, children who have to walk by stepping on the tip and outside of their feet cannot walk in a balanced and fast gait.
How is clubfoot-PEV treated in children?
Clubfoot-PEV can be of different degrees in each child. The treatment process begins immediately after the diagnosis of clubfoot-PEV. It is important to start treatment of clubfoot-PEV as early as possible. The orthopedic doctor will determine a treatment plan based on the child’s age, general health and medical history. In addition, the severity of the condition, the child’s tolerance and parental preference should be taken into account in the treatment plan.
The long-term goal of all treatment is to try to correct the clubfoot, facilitate the child’s normal growth and development and achieve as normal a foot as possible.
The gold standard method in the treatment of idiopathic clubfoot-PEV is the Ponseti method, which is also recommended by the World Health Organization.
Ponseti method in the treatment of clubfoot-PEV in children
Dr. Ignacio Ponseti of the University of Iowa, USA, pioneered this treatment method in the 1940s. Ideally, treatment should begin immediately after birth. The treatment involves gradual correction of the clubfoot-PEV foot with serial manipulations at regular intervals and fixation with a plaster cast. The ligaments and tendons of the foot are stretched with gentle weekly manipulations. The foot is then fixed in this position with a cast that extends above the knee to maintain the degree of correction achieved and to soften the ligaments. Thus, the displaced bones are gradually aligned at the correct angle.
In addition to manipulation and serial casts, the Ponseti treatment method involves a small surgical procedure called Achilles tendon lengthening (Achilles tenotomy) with a small incision through the skin in the last stage to ensure adequate mobility of the ankle in about 85% of patients.
After the tenotomy, the length of the Achilles tendon will increase and the ankle deformity, i.e. the deformity of the foot from the ankle downwards, will be reduced or completely eliminated.
Following Achilles tendon tenotomy, the foot remains in a long leg cast for three weeks. After three weeks, the long leg cast is removed and the child is fitted with a special orthopedic device known as a Denis Browne. The shoes attached to the device are fixed to the device in a special position. The device is worn full time (23 hours a day) for the first 2 months after the last cast is removed. Afterwards, the wearing time is gradually reduced until the age of 1 year, and after the age of 1 year, the device is worn only while the child sleeps (10-12 hours a day). It should be kept in mind that clubfoot-PEV has a very high recurrence rate when the device is not used properly and for the appropriate duration.
When should Ponseti treatment be started in a baby with clubfoot-PEV?
When a baby is born with clubfoot-PEV, an orthopedic doctor experienced in the Ponseti method should start correction treatment as soon as the diagnosis is made. Ideally, a cast for congenital clubfoot should start immediately after birth. However, treatment with the Ponseti method has been shown to be effective even when started several months late.
When is surgical treatment for clubfoot-PEV in children?
In cases of clubfoot-PEV with severe deformity, surgery may be necessary if the desired improvement is not achieved with manipulation and serial casting treatment. Surgical correction is usually not performed until the child is 6-9 months old. In children with clubfoot-PEV, surgery is performed to align the foot in a more normal position.
Surgery usually consists of lengthening the taut tendons in the foot and loosening the joint capsule.
In case of dynamic inward rotation of the foot in children treated with the Ponseti method, surgery for tendon transfer may be necessary.
How long does orthopedic treatment for clubfoot-PEV last?
To ensure that clubfoot-PEV deformity does not recur in children, it is important to keep them under regular control for several years after the treatment (plaster cast or surgery). Recurrence is most common in the first 2 years following treatment. However, clubfoot-PEV can also recur several years after casting or surgery. If clubfoot-PEV recurs, it is treated again with manipulation-plastering or additional surgery. Therefore, it is usually recommended to continue follow-up until the end of growth (around 18 years of age).
Conclusion
Orthopedic treatment of babies born with clubfoot-PEV is usually successful. Children who start treatment early can participate fully in sports and games, as the development of their feet will normalize. The long-term goal of the treatment is to give your child a balanced foot structure that is as normal as possible and that is correctly placed on the ground.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Flatfoot in Children

Flatfoot (pes planus) is when the sole of the foot lacks arch and the inner-mid part of the foot touches the ground more than normal. The arch on the inside of the sole of the foot supports the body when standing or walking. If this arch on the inner side of the foot is missing, it can cause some problems as the body pain is not transferred evenly to the sole of the foot.
Contrary to popular belief, all children are born with flat feet. Due to the thick fatty tissue on the soles of the feet, newborn babies have flat feet. With the shrinkage of this fatty tissue, after about 3 years of age, children begin to develop an arch on the inner side of the sole of the foot. This curve continues to develop until about 4 to 10 years of age.
What are the types of flatfoot in children?
In naturally occurring flatfoot in children, it is seen that the arch of the foot disappears when the child steps, and the arch reappears when the child sits or stands on tiptoe. This is called flexible flatfoot in children.
Rarely, children may also have rigid flatfoot. In this case, when the child sits or stands on tiptoe, there is no arch in the sole of the foot and the sole is flat in all cases. Again, in some rare cases, rigid flatfoot can be detected and treated immediately after birth. Painless flexible flat feet in childhood usually do not cause any problems in adulthood.
Why do some children develop flat feet?
Flexible flatfoot is caused by laxity of the ligaments that support the bones and joints in the foot. Flexible flatfoot is seen in almost all people, especially in people with widespread joint laxity (joint laxity) and who have more flexible joint movements than other people. Hereditary (familial) flatfoot can also be seen.
Flexible flatfoot is seen in some genetic diseases (e.g. children with Down Syndrome). Rigid flatfoot can also occur as a result of abnormal foot development or due to genetics or other diseases such as cerebral palsy (CP), myopathy (muscle disease).
People with tarsal coalition, an abnormal fusion of the two bones in the feet, have problems with their feet before and during puberty. In children with a congenital vertical talus (congenital vertical talus) and a rigid sandal foot appearance (rocker-bottom), complaints may begin at walking age.
What are the symptoms of flat feet in children?
Flexible flatfoot in childhood does not cause any complaints in most children. In studies, approximately 50% of children under 3 years of age have flexible flatfoot, while this rate decreases to 25% between 3-6 years of age.
Parents or relatives are usually the first to notice flat feet in children. The reason why children consult an orthopedic doctor is often the concern of parents or relatives about the appearance of the foot. Flexible flatfoot can cause pain and deformation of shoes in some children during school.
Children with rigid flat feet may experience more severe problems. Pain and complaints of restriction in physical activities, especially in sports or active games, are the leading reasons for children with rigid flat feet to consult an orthopedic doctor.
Symptoms that children may experience with flatfoot:
- Pain in the feet or legs, especially pain, tenderness and cramping in the soles of the feet.
- Outward tilting heel appearance
- Change in the way you walk.
- Pain or discomfort in the foot when walking.
- Difficulty with physical activities such as sports and outdoor play.
How is flat feet diagnosed in children?
Flatfoot is diagnosed by physical examination and radiologic imaging methods. Physical examination starts with observing the gait of the child as he/she enters the room. The orthopedic doctor examines the external appearance of the foot from the back, front and bottom while the child is standing and sitting on the examination table. The foot is checked for skin findings such as callus formation due to abnormal load balance. Range of motion of the joints is measured passively (by the doctor) and actively (by the patient moving the joints themselves) and noted. Especially muscle strength assessment and evaluation of muscle shortness are important for differentiating flatfoot due to other diseases.
The position of the heel and the arch of the foot are evaluated while standing. If the arch of the foot is formed by lifting the tip of the toe or lifting the thumb upwards; flexible flatfoot is diagnosed. If the toe does not arch with standing or lifting the thumb upwards; rigid flatfoot should be considered.
Imaging methods may be requested by the doctor at the first application in flexible flatfoot. X-ray and ultrasound examinations can be performed. In addition, foot base image called podography and pressure analysis may be requested. In hard flat feet, computed tomography (CT) and magnetic resonance imaging (MRI) examinations may be required when radiography is not sufficient. Especially in tarsal coalition disease, which develops as a result of fusion of the foot bones and is the most common cause of hard flatfoot in adolescence, CT or MRI is often required for diagnosis.
The severity of the disease can be classified according to the measurements made on anteroposterior and lateral X-rays of the foot taken while standing, giving load. In addition, the presence of tarsal coalition is investigated with oblique X-rays.
How is flat feet treated in children?
As mentioned above, there is no need for treatment in children with flexible flat feet who have no complaints. However, in children whose orthopedic doctor thinks that the course may be progressive, exercise and insoles may be started.
Contrary to popular belief, there is no scientific evidence that insoles placed in shoes correct flexible flatfoot. However, in severely deformed feet with complaints of pain or functional limitation, insoles may improve the shape of the foot and thus relieve the complaints. The most commonly used insoles are patient-specific insoles that support the inner arch of the foot and UCBL (University of California Brace Laboratory) insoles. In children with pain complaints, ankle stretching and exercises to strengthen the sole muscles should be started along with the use of insoles.
Treatment options for severe flatfoot in childhood vary according to the disease. In children with congenital rocker-bottom and congenital vertical talus, serial casts and surgical treatment may be required to correct the foot position from birth.
Rigid flatfoot is a clinical condition that must be treated in childhood and early treatment is especially important to prevent articular cartilage destruction.
In short, in the treatment of childhood flatfoot, whether flexible or rigid, non-surgical methods such as insoles, exercise and physical therapy should always be applied first, but surgical treatment should be considered in children who do not respond to these methods.
Non-surgical treatments applied in children with flat feet
Rest, medication and cold application: Rest with medication and/or ice application can be applied especially in the treatment of flatfoot associated with tendonitis or in the treatment of patients with flexible flatfoot who develop spasm in the peroneal muscles, in order to suppress complaints that increase with activity and to regress inflammation. These treatments are usually applied for 2-3 weeks.
Shoes and insoles: Soft insoles with medial arch support (inner arch support) made specifically for the patient are the most common treatment option. The type of insoles recommended as effective is UCBL insoles, which are also made with patient-specific measurement. In most patients, insoles provide a reduction in complaints as they prevent the collapse in the inner arch. However, if there is no response to the treatment, it should not be continued persistently, and further examinations, investigations and treatments should be initiated instead.
Exercise and physical therapy: Especially in children with Achilles tendon tension, a regular exercise program at home is of great importance in reducing complaints and in the course of the disease.
Strengthening and stretching exercises for the tendons that allow the front part of the foot to turn inward and outward are also very effective in the formation of a dynamic arch of the foot. Especially in flexible flat feet, each patient should be included in an exercise and/or physical therapy program before deciding on surgical treatment.
Methods applied in flatfoot surgery in children
Although there are many options for surgical treatment, there is no definite justification for the need for surgical treatment. The only valid reason for surgical treatment is the failure of non-operative treatments and the persistence of pain and functional limitation of the child. In surgical treatment, soft tissue surgeries (tendons and ligaments) and bone surgeries can be performed together or separately. Today, with a current surgical method called arthroereisis, joint movement can be restricted and the arch of the foot can be formed.
In arthroereisis surgery, which is used in flexible arthropedic surgery in children, an implant screw is inserted into the foot joint through a very small incision and the arch of the foot is corrected. This method is applied with a small surgical intervention. The results of arthroereisis surgery are extremely favorable clinically and radiologically.
In terms of timing in surgical treatments, some surgeons advocate correction in the early period, i.e. before the age of 10, while the development of the foot continues; some authors advocate intervention in the foot after the age of 10. In general, instead of waiting for a certain age in childhood flatfoot surgery, it is more appropriate to decide according to the patient’s complaints and physical examination. Especially in children with inflexible flat feet, surgery may be needed much earlier.
You should consult an orthopedic doctor when the following findings occur in your child;
- When you notice that the arch of the foot is not sitting or stepping
- Tires easily when standing or does not want to walk because of pain
- When you notice difficulty in moving the foot in and out while playing sports or playing outside and an abnormality in foot placement, especially when running
- When you notice a crushing and bending in your child’s daily shoes, especially towards the inside
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Cerebral Palsy Clinic

Cerebral Palsy is a group of permanent disorders that occur in infancy and early childhood and are characterized by movement and developmental disorders caused by non-progressive problems in the developing brain. Motor disorders in Cerebral Palsy are also accompanied by sensory, perceptual, cognitive, communicative and behavioral problems, epilepsy and secondary bone, muscle and joint problems.
The aim of cerebral palsy rehabilitation is to identify functional and structural disorders in the body and take necessary measures, minimize restrictions in movements, improve skills, and support participation in society.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Muscular distrophy
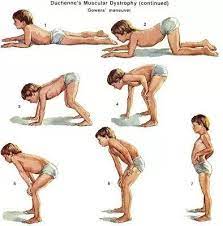
Muscular dystrophy is a group of genetically inherited muscle diseases with a progressive course. Muscle diseases are inherited genetically. Many diseases can occur when disease-carrying genes in the mother, father or both are passed on to children. The prevalence of consanguineous marriages in Turkey is the most important factor increasing the incidence of muscle diseases. Sometimes muscle disease can also occur in children of people who have no family history of the disease. This occurs as a result of spontaneous mutations in genes (changes in gene structure that can lead to diseases).
Muscular dystrophy is a disorder that starts in childhood, is more common in boys and causes symptoms such as muscle weakness, deformities in the joints and spine, difficulty in movements, rapid fatigue, respiratory system-related deficiencies, difficulty walking and climbing stairs.
What are the symptoms of muscular dystrophy?
The biggest problem caused by progressive muscle weakness in muscular dystrophy patients is the loss of the ability to perform activities and functions. Especially due to the weakness of the muscles around the hips; it leads to inadequacy in many functional activities such as getting up from the floor, walking and climbing up and down stairs, and negatively affects the level of independence of children. As a result of progressive and widespread muscle weakness, body alignment may be impaired. Shortening of some muscles and consequent limitations in ankle, knee and hip joint movements may occur, especially due to strength imbalance in the muscles around the joints. Curvature of the spine called scoliosis may occur due to increased weakness in the muscles of the trunk and the child sitting on one side without support.
Symptoms of muscular dystrophy
- Muscle laxity, weakness
- Difficulty getting up from the floor
- Difficulty going up and down stairs
- Gait disturbances, falls
- Inability or inability to run
- Deformities of the arms and legs
- Deformities such as scoliosis and kyphosis in the spine
What are the types of muscular dystrophy?
–Duchenne Muscular Dystrophy: It is the most common type of muscular dystrophy and occurs in approximately 1 in every 3500 live male births. Patients are male and females are usually carriers. Especially the shoulder and hip muscles close to the trunk are involved and as the disease progresses, muscle weakness is observed in the muscles of the arms and legs. The disease usually manifests itself between the ages of 3 and 6, but may also manifest itself before the age of 3 in the form of a delay in walking. Waddling, difficulty in climbing stairs and tiptoe walking are the early signs of the disease. The ankle does not come backwards, the knee does not become fully straight, and increased lumbar collapse are among the common findings in Duchenne muscular dystrophy patients.
Pseudohypertrophy (pseudohypertrophy), especially in the calf muscles, is a typical finding of the disease. As the disease progresses, joint stiffness (contracture) may develop. Since the disease affects the muscles, it also affects the heart and respiratory system.
–Becker Muscular Dystrophy: Similar to Duchenne muscular dystrophy, but the age of onset is later and deterioration in muscle function progresses more slowly. In some patients, symptoms are observed early, while in others gait starts to deteriorate after the age of 20. As in Duchenne, Becker muscular dystrophy also causes respiratory and cardiac problems.
–Emery-Dreifuss Muscular Dystrophy: It is a rare muscle disease that develops due to a genetic defect in the X chromosome. The disease is characterized by slow progression of muscle disease, heart muscle disease and early joint stiffness. Early findings include clumsiness, weakness and tiptoe gait.
Other types of muscular dystrophy include rare types of muscular dystrophy such as limb-girdle muscular dystrophy and fascioscapulohumeral muscular dystrophy.
How is muscular dystrophy diagnosed?
Genetic examination is important for the early diagnosis of muscular dystrophy. Blood tests, EMG (electroneuromyography) and muscle biopsy are required to diagnose these patients. In addition, radiologic imaging methods such as X-ray, muscle ultrasound, MRI (magnetic resonance imaging) are also used if necessary.
What is the treatment for muscular dystrophy?
Although there is no definitive treatment for the disease, pediatric neurology, chest diseases, physical therapy and rehabilitation, orthopedics departments follow-up and treatments are applied to eliminate additional problems that arise. Supportive drug treatments are given when necessary. Studies on gene therapy are ongoing.
Muscular dystrophy not only affects the movement system but also the heart and respiratory system. A multidisciplinary approach is very important in the follow-up of the disease. Physical therapy and rehabilitation programs in children with muscular dystrophy can prevent joint stiffness (contractures) and prolong mobility. Patients should not be overtired while exercising, and regular rest breaks should be given in daily life and during exercises.
The main goal of orthopedic surgical interventions is to maintain the functional status of the patient. The most important problem in children who lose their walking capacity and become wheelchair-bound is the resulting spinal deformities. Orthopedically, joint stiffness can be treated with loosening surgeries and spinal deformities can be treated surgically.
Conclusion
Muscular dystrophy is a muscle disease frequently seen in boys, characterized by delayed walking, waddling gait and muscle weakness, and in the late period, joint stiffness, deformities and dysfunctions that develop due to muscle weakness. Early diagnosis and treatment of muscular dystrophy is important.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Perthes Disease

Perthes’ disease, or Legg-Calve-Perthes’ disease in its full medical name, is a vascular blood supply disorder of the growth plate of the femoral head in the hip joint in childhood. Due to this blood supply disorder, the bone tissue in the femoral head loses its vitality and avascular necrosis occurs. Although more than 100 years have passed since Perthes’ disease was first described, its cause and treatment are still unclear.
Generally, orthopedists’ treatment preferences are shaped according to age, radiologic appearance and examination findings of the patient. The main aim of both non-surgical and surgical treatment is to reduce the hip pain of the child, to maintain the range of motion and to ensure the compliance of the hip joint. Thus, deformity of the femoral head and damage to the articular cartilage can be prevented in the early period and calcification of the joint can be prevented in the future.
Who has Perthes’ disease?
According to studies, the incidence of the disease varies between 0.2 and 19.1 per 100,000. Although Perthes’ disease is common in children between the ages of 4 and 10, it can be seen at any age throughout skeletal development. It is more common in boys than girls. It is usually seen in one hip joint, but about 10% are bilateral. There is little evidence of genetic predisposition. Since it is not seen together in twin children, it is thought to be related to environmental factors.
What are the causes of Perthes’ disease?
The most emphasized definition of Perthes’ disease is the definition of “predisposed child”. The definition of a predisposed child includes factors such as abnormal growth and development, malnutrition, hip joint trauma, hyperactivity, attention deficit, environmental factors and exposure to smoking. In children diagnosed with Perthes’ disease, wrist x-rays may show retardation in bone age compared to their peers.
A clear link between the mechanism of the disease and growth arrest has not yet been established. Children with diseases such as sickle cell anemia, thalassemia, leukemia, lymphoma, hemophilia, clotting disorders may also have impaired blood supply to the growth cartilage of the femoral head. However, the exact cause of Perthes’ disease has not yet been established.
What are the symptoms of Perthes’ disease?
Generally, the first thing that families notice is the child’s limping while walking. The limp increases with physical activity and recedes with rest. The second most common complaint is pain. Children may describe pain in the buttocks, groin, thighs and sometimes the knee. The pain increases with physical activity and peaks especially in the evening. Night pain in the hip is common in Perthes’ disease. Another symptom is the development of limitation of movement in the hip joint.
In the history of the patients, families often mention a past trauma and state that the pain goes away after rest. They may especially say that their child is more active than other children and runs and jumps more. Usually, compared to their peers, these children are underdeveloped and smaller. However, it is important to remember that Perthes’ disease can also occur in a fat and less active child.
What is the natural history of Perthes’ disease?
The natural history of Perthes’ disease depends on factors such as age and the extent to which the femoral head is affected, but there is no consensus on the importance of these risk factors. Today, the effect of the age of onset of the disease on the outcome is very clear. It has been shown in many studies that the outcome of the disease is much better in children younger than 6 years of age and even younger than 4 years of age. However, it should be kept in mind that the prognosis of Perthes’ disease in a child younger than 6 years of age may be poor, albeit to a lesser extent.
In the early stages of Perthes’ disease, the patient usually has no symptoms and the disease may be detected incidentally by X-rays taken for a different purpose. In the later stages, complaints such as pain, limping and difficulty in movement occur in children.
The site of avascular necrosis may involve part or all of the femoral head. This causes the femoral head to collapse and its roundness to deteriorate. The body’s ability to regenerate dead tissue also applies to bone tissue.
In Perthes’ cases, bone that has lost its vitality is removed from the area by the body and the process of new bone formation begins. In this process, it must be ensured that the femoral head remains in the socket in the hip joint. The aim of the treatment of Perthes’ disease is to ensure that the femoral head remains in its socket in a harmonious manner and at the same time to support the body to clean and regenerate the dead bone tissue. The disease follows a self-limiting process and can be cured in about 2-5 years. Children diagnosed with Perthes’ disease may require lifelong follow-up.
How is Perthes disease diagnosed?
A differential diagnosis should be made with diseases that cause limping and hip pain in children. Most of the time, a differential diagnosis can be made with the evaluation of age, gender and duration of findings, a good physical examination and radiologic examination. History, physical examination and radiologic imaging methods are used in the diagnosis of Perthes disease.
Especially in the early period, magnetic resonance imaging, which is taken before changes occur on the x-ray, is very helpful in early diagnosis. In the advanced period, hip x-ray diagnosis can be easily made. A child with a limp and pain should be taken to an orthopedic and traumatology doctor immediately. Examination and evaluation by an orthopedic specialist is very important in early diagnosis. Early diagnosis of Perthes disease also affects its prognosis.
How is Perthes’ disease treated?
Surgical and non-surgical treatment options in the treatment of Perthes’ disease may vary according to the stage of the disease, the level of involvement of the femoral head, the age of the child and physical examination findings. Since the remodeling of the femoral head is rapid, especially in children in the age group affected by Perthes’ disease, non-surgical and surgical treatments that provide coverage of the femoral head constitute the main principle of treatment. The aim of treatment is to support the remodeling of the femoral head whose nutrition is impaired, to ensure that it is compatible with the hip joint socket and to prevent femoral head deformity.
In the early stages of Perthes disease, it is recommended not to load the joint. Depending on the stage of the disease, it may sometimes be appropriate to relieve the load by using a splint. Since the disease can last for 2-5 years, crutches should be used if necessary to rest the hip during periods of increased pain and limping. During these painful periods, children are usually not allowed to participate in sports activities.
Physical therapy and rehabilitation programs may be recommended to prevent or reduce conditions such as limitation of movement and loss of function. With the exercises, the muscles around the hip are strengthened and the tensions that cause joint movement limitation can be relieved.
In the future, if joint incompatibility occurs due to severe deterioration of the femoral head, surgeries to make the joint more compatible may be required. In surgical treatment, various osteotomies are used to prevent dislocation of the femoral head, to improve joint congruence and to prevent the compression of the damaged surface of the femoral head. Operations such as arthrodiastasis and femoral head reduction are also performed.
Conclusion
Perthes’ disease is a disease of the hip joint in children aged 4-10 years. Generally, the disease follows a self-limiting process and heals in about 2-5 years. Late diagnosis and cartilage tissue damage may lead to hip joint calcification in the future.
If your child has even mild hip and knee pain and limping, it is important to take him/her to an orthopedic doctor immediately for early diagnosis and treatment.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Metatarsus Adductus in Children

Metatarsus adductus is a congenital foot deformity in which the front part of the foot turns inward. Normally, when we look at the foot from the bottom, the outer part of the foot, which is roughly V-shaped, bends inward and the inner part bends inward. In babies born with Metatarsus adductus deformity in their feet, the foot is curved inward. The main difference from other congenital foot deformities is that the back of the foot, the heel, is not affected. The foot shape can be roughly compared to a bean.
What are the causes of metatarsus adductus in the foot?
In the formation of metatarsus adductus foot deformity, the exact cause of which is unclear; conditions such as posture disorder in the womb, compression and compression in the uterus are considered as possible causes.
Which children have metatarsus adductus?
Since mild forms of metatarsus adductus are frequently seen, it is difficult to determine the exact frequency. It can be seen in roughly 1 baby in every hundred live births. It can be seen frequently with diseases such as developmental hip dislocation and torticollis.
What are the symptoms of metatarsus adductus in the foot?
Metatarsus adductus can be recognized by the family immediately after birth or in the following period. The main finding is that the front part of the foot turns inward compared to the back part. There may be a protrusion on the outside of the foot and the 1st and 2nd toes may be separated. In the advanced period, it manifests itself as inward stepping in the walking child.
How is metarsus adductus diagnosed?
The diagnosis of metarsus adductus deformity in the foot is made by physical examination and imaging methods. In the physical examination, the severity of the disease is determined by evaluating the flexibility of the curvature in the anterior part of the foot. In flexible deformities, the anterior part of the foot can be corrected with manipulation, while in rigid deformities, the foot cannot be corrected with manipulation. Radiologically, inward rotation of the metatarsal bones, that is, the metatarsal bones of the foot, is observed.
What is the treatment of metatarsus adductus foot in children?
If the front part of the foot can be corrected with active movement and there is a flexible deformity, the family should be informed that this does not require treatment and will resolve spontaneously. The massage technique to be applied to the foot is shown and the patient is followed up.
In feet that do not correct actively but correct when stretched passively, treatment can only be performed in the form of follow-up, massage, special shoes, orthotics and plastering.
Plastering is recommended especially in children older than 6 months if foot deformity persists. In feet that cannot be corrected passively, casts are applied in the first treatment. If the foot is resistant to casting, soft tissue loosening can be performed surgically.
Conclusion
Metatarsus adductus is a congenital foot deformity characterized by inward rotation of the anterior part of the foot. Since it is common in children with developmental hip dislocation, hip ultrasound should be performed in these cases. The flexibility of the foot is important in the diagnosis and treatment of this disorder and while actively recovering feet do not require treatment, shoes or plastering are the first treatment options for passively recovering feet and plastering is the first treatment option for stiff and never recovering feet.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Limping and Gait Disorders in Children

Limping is a common gait disorder in children and the unknown cause causes anxiety in the family. A limp can be caused by a benign condition or it can be an early sign of a disease that may have a bad outcome. There are many causes of limping or abnormal gait in children. These can be pain or inflammation, muscle weakness or abnormal muscle activity, joint disorders or leg length inequality.
Diagnosis: A good history is the first step in diagnosis. In the history, the presence of trauma, existing diseases and the duration of the complaint are questioned. Severe complaints occurring in a short period of time may be due to trauma and may also be the main finding of joint inflammation. Complaints that have been present for a long time often require further investigation as they may be due to a chronic disease.
The history of the child is very important, especially in infancy when the child has difficulty expressing himself/herself, and the medical history should be taken from birth. For example, a history of premature birth and follow-up in incubators in neonatal intensive care can lead to a diagnosis of cerebral palsy with a delay in motor skills. Similarly, family history is very important in the diagnosis of most genetic diseases.
The examination starts with watching the child walk when he/she enters the room. It may be difficult to determine the location and intensity of pain, especially in young children. For this, the whole leg, i.e. hip, thigh, knee, calf, ankle and foot should be checked for range of motion and tenderness. Swelling, redness, limitation of movement and increased temperature in the sensitive joint are signs of joint inflammation.
Which tests are performed in gait disorders in children?
After the history and physical examination, imaging and laboratory tests are performed. If the pain cannot be localized on imaging, anteroposterior and lateral x-rays including the whole leg should be taken in young children. X-ray imaging is especially important in terms of excluding conditions that require emergency intervention. It can show not only fractures due to trauma, but also lesions in the bone, i.e. masses, as well as diseases that may occur in the growth plates.
Ultrasound (US), Computed Tomography (CT), Magnetic Resonance Imaging (MRI) may be requested as advanced radiologic imaging in the presence of physical examination, X-ray findings and in children with long-term complaints. Magnetic resonance imaging is especially important in the evaluation of disorders of intra-articular structures.
Laboratory tests are a very important step in the early diagnosis of a child with joint inflammation. Elevated inflammatory markers such as sedimentation, CRP and increased leukocytes in the complete blood count may indicate joint inflammation. This inflammation may be a temporary and benign inflammation of the joint (transient synovitis) or septic arthritis, which is a microbial inflammation of the joint and requires urgent surgical intervention. Advanced laboratory tests may be ordered for differential diagnosis in suspected multiple diagnoses. It should be kept in mind that follow-up is part of the treatment in children with a normal physical examination and laboratory tests.
Abnormal gait and limping patterns in children
Painful walking (Antalgic walking)
Antalgic gait, also known as painful gait, may be caused by painful conditions in the lower extremities, i.e. hips and legs, or may be observed due to a disease related to the lower back. In painful gait, the child walks by shortening the stepping phase of the gait, trying to give less load on that side or by hopping.
Trendelenburg gait (duck-like gait)
Trendelenburg gait is caused by weakness of the abductor muscles in the hip region, which open the hip sideways. The abductor muscles also stabilize the side of the hip that is in the swing phase when walking, i.e. not in contact with the ground.
Since the abductor muscle in the problematic hip joint is weakened, when the affected side is stepped on while walking, the opposite hip cannot be supported and the hip tilts to that side. This creates a gait that resembles a duck-like gait when bilateral in diseases such as hip dislocation. In addition to hip dislocation, Trendelenburg gait can also be seen in other diseases such as Perthes’ disease, which causes bony deformity of the hip joint.
Spastic gait
Spasticity is defined as involuntary excessive contraction of body movement muscles and spastic gait is typical especially in patients with cerebral palsy. In the form of spastic gait, fingertip gait due to tense Achilles tendon, and bent-knee gait due to tense hamstring muscles (muscles of the posterior group of the thigh) can be seen. The presence of only one of these can also cause hip flexion, knee flexion and toe-tip gait. Shear gait in the legs due to adductor muscles on the inner groin side of the hip may also cause spastic gait.
Short leg walk
It is the way of walking in children with leg length inequality. One-sided toe-tip walking can be seen to support the shorter side. At the same time, it can be observed that they walk by bending the leg at the hip and knee on the long side. In children with a small leg shortness difference, no obvious gait disorder may not be detected as a result of the body’s adaptation.
Causes of gait disorders in children according to age
Infancy (1-3 years) : A good history is very important in this period because this is not an age group that can express itself. The history should be as detailed as possible. Families may not mention a very minor trauma or event as they may not think that it may cause limping.
The examination starts with observing the child’s gait as mentioned above. In this age group, a gait pattern like in the adult period is not expected. Babies walk by spreading their legs wider and slightly bending their hips and knees to maintain balance. Babies cannot increase their stride length to walk fast, but they increase their pace, which leads to a fast and unbalanced gait. The most common conditions that cause painless limping or abnormal gait in infancy are developmental hip dysplasia (hip dislocation), leg length inequalities and neuromuscular diseases (cerebral palsy, spina bifida etc.).
Apart from limping, different gait patterns can also be seen during this period;
Tip-toe gait: Painless fingertip gait is one of the common reasons for referral to pediatric orthopedics. It can be idiopathic, that is, it can be seen without a specific cause, or it can be seen due to a neuromuscular disease involving the nervous system and movement system. The patient walks on tiptoes without a cause or due to tension in the posterior calf group muscles, holding the heel in the air. Leg length inequality should be suspected in unilateral cases. As mentioned above, differential diagnosis with a detailed history and physical examination is very important in these children.
Inward and outward stepping gait: Inward stepping while walking in infants is one of the most common reasons for families to consult pediatric orthopedics. The most common cause of this condition is angular changes in the upper part of the thigh bone (femoral neck). This value, which can vary by about 30 degrees in each person, also determines our comfortable sitting position on the floor. People with a greater upper thigh angle forward (increased femoral anteversion angle) sit comfortably in the W position because they can turn their legs inward more easily.
On the contrary, those with an upper thigh angle toward the back (those with a decreased femoral anteversion angle) sit more comfortably in the cross-legged position where the thigh is turned outward.
Therefore, inward pressing is observed more frequently in babies sitting in the W position. Most babies, especially those with a family history, have a high upper thigh angle (femoral anteversion angle) and have W sitting and inward pressing. Pressing in is often corrected with shoes, which leads to a misperception that shoes correct inward pressing. This is because the most common cause of inward pressing is upper thigh angular change, i.e. hip joint angular change.
Other possible diagnoses can be excluded by physical examination and radiologic imaging if necessary. Babies who do not have a bony deformity on physical examination are only followed up. The family is informed that the child’s normal gait will improve over time and this condition will improve between the ages of 4-7.
Waddling gait Waddling gait is a gait pattern observed in children with braces on their legs. Especially between the ages of 1-2 years, babies may have physiologically, i.e. naturally, braces (genu varum). This condition, called physiologic genu varum, can also be seen due to rickets, which often develops due to vitamin D deficiency in the diet. Findings of rickets can be detected with radiologic imaging methods in children with braces leg appearance that is more than normal in physical examination and becomes more prominent with walking.
Braces leg, genu varum, can also occur due to diseases affecting the growth plate and can be diagnosed by X-ray imaging. Blount’s disease, which is seen especially in mildly obese or obese infants and children, also causes deformity in the legs. In this case, early diagnosis and early treatment with appropriate orthoses and devices can prevent the progression of the disease.
In severe cases, surgical correction may be required. For this reason, children with a waddling gait and especially those with a braces leg appearance that becomes more pronounced with pressure should definitely be evaluated by an Orthopedics and Traumatology Specialist. Treatment is determined according to the severity of the condition and there are varying options such as follow-up, device and surgical treatment.
Childhood (4-10 years)
Investigating the cause of gait disturbance in this period is easier than in infancy as the child is old enough to express himself/herself. At the same time, abnormal gait decreases during this period and an adult-like gait is formed by the age of 7. Painful conditions in childhood should be taken seriously. Especially in this period, other possible diagnoses must be excluded before making the diagnosis of pain due to changes in the growth plates, which is frequently seen in this period and is popularly referred to as growth pain. The so-called growing pain, which is caused by growth plates, is frequently seen in the heel, bones of the foot and under the kneecap. Pain and limping after activity relieves with rest.
Depending on the history of the child, pain at rest or pain that wakes the child from sleep at night should be taken into consideration. In children of this age with pain at rest and night pain, further imaging tests such as magnetic resonance imaging-MR may be necessary to identify the underlying problem.
Adolescence (11-15 years)
The adolescent child can give the doctor a detailed history of the limp. He/she can also clearly express the location of the pain. In this period, especially in obese children, the slippage of the upper thigh growth plate, called femoral head epiphyseal slippage, can cause sudden onset or progressive limping in children. This age group is also prone to ligament tears and articular cartilage damage that may develop due to injury during sports.
Conclusion
It is important that limping and other gait disorders in children are investigated, the cause is explained to the family and their concerns are addressed. There are many causes of limping or abnormal gait in children. Limping can be caused by a benign, simple condition or it can be an early sign of a disease that can have bad consequences. Evaluation and follow-up of children with gait disorders by an Orthopedic Doctor provides early diagnosis and treatment.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Arthroscopy and Sports Surgery

Joint pain is common in people who are active in their daily lives, those who work in mobile jobs and athletes. Today, many conditions that cause knee, hip, shoulder, elbow, wrist and ankle joint pain are treated with arthroscopic surgery. These conditions are usually treated with minimally invasive and arthroscopic surgical methods. Thus, people can return to their active and sportive lives. Arthroscopic surgery is called arthroscopic surgery, which is performed with special surgical instruments through small incisions made to enter the joint. Arthroscopic surgery, also known as closed joint surgery, is a less risky surgery with a shorter recovery period. During arthroscopy, the physician can both identify the problem and perform the necessary surgical treatment by watching the inside of the joint on the screen. Today, all major joints can be treated with arthroscopic surgery.
- Advantages of Arthroscopic Joint Surgery;
- Surgical procedure with small incisions
- Protection of healthy tissues
- Less bleeding
- Faster and more painless recovery
- Quicker return to daily life
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Omuz ArtroskopisiShoulder Arthroscopy

What is arthroscopy?
Arthroscopy is a combination of the Latin word “joint” and the English word “camera”. It means examining the joint with a camera. When arthroscopy was first discovered, it was only used to visualize the inside of the joint. With the technological advances in the medical field, arthroscopic methods have also developed and arthroscopy has become a surgical treatment technique. Arthroscopy can be applied to many joints in the body. The most common joints are the knee, shoulder, ankle and hip joints. Especially the shoulder joint is a suitable joint for arthroscopy, where arthroscopic surgical techniques can be used for a wide range of purposes.
In which diseases can shoulder arthroscopy be applied?
The application area of shoulder arthroscopy is quite wide. However, the most common areas of application are muscle tear repair, treatment of recurrent shoulder dislocation, detection of some fractures, removal of free body or joint tumor from the joint, treatment of joint infection, treatment of cartilage problems, treatment of tendon problems.
How is shoulder arthroscopy performed?
Shoulder arthroscopy is a surgical procedure, which means surgery. For this reason, this procedure should be performed in the operating room, under the supervision of an anesthesiologist and under general anesthesia. Shoulder arthroscopy can be performed in a sitting or lying position. After the patient’s anesthesia is completed, the patient is positioned. Special operating room tables and special apparatus are required to give the patient the appropriate position. After positioning, the shoulder area to be operated on is prepared sterile and covered with special sterile drapes. After drawing the anatomical reference points around the shoulder with a pencil, a needle is inserted into the joint from behind and the joint is inflated with fluid. Then, a special camera tip called “scope” is inserted into the joint through approximately 1 cm incisions around the shoulder. After the disorders in the intra-articular and surrounding tissues are detected, the surgical intervention to be applied for the pre-operative diagnosis is started. Surgical intervention is performed with endoscopic, i.e. closed techniques.
In which diseases can shoulder arthroscopy be applied?
The application area of shoulder arthroscopy is quite wide. However, the most common areas of application are muscle tear repair, treatment of recurrent shoulder dislocation, detection of some fractures, removal of free body or joint tumor from the joint, treatment of joint infection, treatment of cartilage problems, treatment of tendon problems.
What are the advantages of arthroscopic, i.e. closed, shoulder surgeries?
Shoulder surgeries can be performed closed or open. In open surgery, relatively larger incisions are made and muscles and other soft tissues need to be separated from each other in order to bring the tissues to a position that can be seen visually.
Therefore, more muscle and soft tissue injuries occur during open surgery. This leads to more postoperative pain and a more difficult postoperative rehabilitation process due to soft tissue damage. Since closed, i.e. arthroscopic shoulder surgeries are performed through small incisions and without opening the joint, they cause less muscle and soft tissue damage, resulting in less postoperative pain and a more comfortable rehabilitation process. Another advantage of arthroscopic surgery is that the tissues can be seen under the magnification of the camera, allowing better evaluation of the damaged tissues.
What is the recovery process after shoulder arthroscopy?
As with any treatment, there is a certain recovery period after shoulder arthroscopy. The recovery process after shoulder arthroscopy depends entirely on the type of disease and the surgical technique applied.
After some surgical interventions, the patient can quickly return to active life, while after some surgeries, the patient may need to use a shoulder sling for a few weeks and then undergo physical therapy to protect the procedure performed.
What complications can occur after shoulder arthroscopy?
The incidence of complications in shoulder arthroscopy is very low in experienced hands with advanced training in this field. Complications that may occur are not specific to this technique, but are complications such as infection etc. that can be seen in any surgical intervention. However, as we mentioned before, shoulder arthroscopy is a specialized surgery requiring advanced arthroscopy experience, using advanced techniques and surgical instruments, and the risk of complications will decrease when performed by experienced surgeons.
Conclusion
Shoulder arthroscopy is a surgical method that uses advanced surgical techniques, allows surgery to be performed through small incisions around the shoulder, allows surgical treatment of different shoulder diseases, has proven effectiveness and has a low complication rate in experienced hands.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Arthroscopy
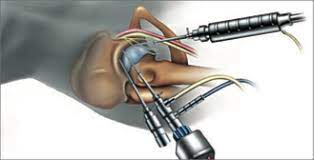
Hip joint structure
The hip is the joint that joins the thigh bone (femur) to the pelvis (pelvis). The head of the thigh bone (femoral head) is round like a ball. The femoral head is placed in the socket (acetabulum) formed by the pelvis and forms the hip joint. The femoral head and the socket that form the hip joint are covered with a smooth-surfaced, slippery cartilage layer. This cartilage tissue allows the two bones to slide and move easily over each other.
A thick cartilaginous ring-shaped structure around the acetabulum, the hip joint socket, is called the labrum. While the labrum increases the depth of the socket in the hip, it also provides the stability of the hip joint by wrapping the femoral head like a gasket. Numerous ligaments and muscle tissues in the hip also support the stability of the joint.
What is hip arthroscopy?
Hip arthroscopy is a technique of closed surgery that allows the orthopedic doctor to evaluate the bone, ligament and cartilage structure of the joint and to intervene surgically. Hip arthroscopy is a joint-sparing surgery that allows early detection and intervention of problems in the joint and thus prevents rapid calcification of the hip. Hip arthroscopy is a different and more difficult technique than other joint arthroscopies. For this reason, it requires specialized equipment, and for successful surgical treatment, the specialist performing the surgery must have advanced training and experience in this field.
During arthroscopic surgery of the hip, a camera is inserted through a small hole into the hip joint and the image of the inside of the joint is transferred to the screen. With the help of special surgical instruments inserted into the joint through other small holes, the orthopedic doctor performs the procedure by watching it on the screen.
During arthroscopic surgery, the intra-articular structures are seen very closely and magnified. Thus, diseased tissues can be detected and treated much better. Arthroscopic surgery of the hip allows direct access into the joint without damaging or injuring the surrounding tissues and intervening only in the diseased tissues. In arthroscopic surgery, soft tissues such as muscles and capsules that provide joint movements, which are difficult to heal and painful, are not touched at all. This is especially important in the hip. Thus, postoperative joint movements are painless and comfortable. This allows for early and accelerated rehabilitation. It allows an earlier return to active life and sports. Since smaller incisions are made compared to open surgery, the risk of infection is also lower. Hip joint arthroscopy is a day surgery that does not require hospitalization.
In which cases is hip arthroscopy performed?
- In the diagnosis and treatment of problems that have been proven to originate from the hip joint but whose clinical and radiologic cause cannot be elucidated
- Removal of cartilage fragments that have fallen into the hip joint, tissues formed in the joint, bone-cement fragments in the joint space in hip prostheses
- In the early stage of hip osteoarthritis
- Hip impingement syndrome
- Acetabular labrum tears
- Partial cartilage damage
- Iliopsoas tendon disorders and bursitis
- Iliotibial band release
- Gluteus minimus tendon repair
- Resistant synovitis cases
- Hip joint infection
Who cannot undergo hip arthroscopy?
In order to perform hip arthroscopy successfully, the joint space must be clearly visible on the X-ray image of the hip. If a joint space cannot be detected, the arthritis has progressed too far. In this case, it is not possible to relieve the patient of pain by removing free lime and cartilage fragments. Hip arthroscopy is also not possible in very overweight and obese patients.
How is hip arthroscopy performed?
The hip is the deepest joint in the body. Its ball-and-socket shape also makes it difficult to enter the joint.
At the same time, the femoral head is located quite deep in the acetabular socket, so it is more difficult to reach it with an arthroscope than in the knee or shoulder joint. This problem has been solved by the development of new surgical instruments. Therefore, unlike other joint arthroscopies, arthroscopic operations of the hip cannot be performed without advanced operating room conditions, “traction table” and “scopy”.
First of all, the leg to be operated on is placed on the traction table and the hip joint is opened by 1 cm by applying controlled traction. A camera system is inserted through a 1cm incision made in the hip joint, accompanied by a device called scopi, which gives an instant X-ray image on the screen. Surgical instruments are inserted into the joint through one or two other holes and the operation is performed.
During hip arthroscopy, the intra-articular structures are first evaluated by direct visualization. Extremely small structures that cannot be detected by X-ray, tomography or even MRI-magnetic resonance imaging are clearly visualized by projecting them onto a television screen. The surgeon arthroscopically evaluates the structures inside the hip, identifies the problem causing the pain and then begins the surgical treatment.
Depending on the disorder detected during hip arthroscopy and its degree, there are various surgical methods that the orthopedic surgeon can apply in treatment. For example, if there is a frayed tear in the labrum surrounding the edge of the acetabulum, the seat of the hip joint, the damaged part is removed, leaving only the intact, uninjured labrum tissue. If the tear in the labrum has not caused abrasion of the labrum and has a smooth edge, repair can be performed without cutting out a piece of the labrum. In cases with hip impingement syndrome, abnormal bone structures are filed down and reshaped. If the cause of hip pain is cartilage deposits that have fallen into the joint, they are removed and the inside of the hip joint is cleaned. Minor damage to the hip joint cartilage can be cleaned and necessary procedures can be performed. In the presence of recurrent resistant synovitis or intra-articular infection of the synovial membrane, adhesions and thicknesses detected in the joint are cleaned, the joint is washed and a biopsy can be taken.
Recovery period after hip arthroscopy
Patients usually stay in hospital for only one or two days after hip arthroscopy surgery. Depending on the surgical procedure, patients may need to walk with crutches or a cane with a bracelet for a while. It is important that the exercises prescribed by the physiotherapist according to the patient’s condition are performed regularly at home.
Complications that may occur after hip arthroscopy include: complications related to anesthesia, infection, bleeding and swelling, thrombophlebitis, small instrument breakage in the joint, nerve damage, pain or numbness. These complication rates are lower when comparing arthroscopic surgery methods with open surgery methods.
Thanks to the smaller incisions made in minimal surgical methods such as hip arthroscopy, it is possible to detect and treat the problem causing pain in the joint early, with less blood loss and less tissue damage. After hip joint surgery, which is a joint-sparing surgery, patients experience less pain and can move more easily during the recovery period. Most patients return to their daily lives after a short period of time.
Conclusion
Developments in hip arthroscopy have provided great success in eliminating the problem with closed surgery in the early period before it reaches advanced calcification in this joint. Conditions such as hip impingement syndrome and labrum tears can be treated with hip arthroscopy. Hip arthroscopy is technically more difficult than other arthroscopies. When hip arthroscopy is performed by experienced orthopedic specialists trained in hip arthroscopy, the clinical results and patient satisfaction are better.
What is hip impingement disease?
As a result of premature or incompatible contact of the ball part of the femoral head of the hip with the socket (acetabulum) during movement, impingement occurs at the edge of the joint. This causes pain in the hip, usually in the groin area or on the outer side. Initially, the pain is more pronounced during long walks or sporting activities, but over time it can also be felt in everyday life. Especially when sitting or squatting for a long time, the pain increases, causing complaints such as stiffness and difficulty in movement. This inappropriate contact and compression, which recurs over time, causes damage to the articular cartilage and leads to calcification of the joint. When hip osteoarthritis occurs, patients need hip replacement surgery to get rid of this persistent pain, limitation of movement and difficulty in walking.
How does hip impingement occur?
It is a disease caused by compression of the cartilage and labrum tissue in between due to excessive contact between the femoral head-neck junction and the acetabular socket during hip joint movement. Hip impingement disease can be seen in three types;
- Glass type: It is caused by a hump-like protrusion in the bone where the femoral head and neck meet in the hip joint.
- Pincer type: It is seen when the acetabular socket of the hip joint is deeper and the coverage area over the femoral head is increased. In this type; a fringe-like protrusion is formed from the roof of the acetabulum on the outer lateral edge.
- Cases with Cam and Pincer types together.
In the Pincer type of hip impingement, the femur hits the protrusion on the roof of the acetabular socket during movement, resulting in damage to the cartilage. In the Cam type, the bump at the femoral head-neck junction rubs against the labrum, causing damage and tearing of the labrum. In both cases, labrum tear and cartilage damage as a result of repetitive friction and compression results in calcification of the hip joint in the future. These protrusions and hump-shaped deformities in the hip joint begin to form during adolescence, but the cause is not yet known.
What are the patient complaints in hip impingement disease?
The first complaint of patients is sudden pain in the groin area that occurs with certain movements or after exertion. Hip pain may occur after prolonged sitting or walking. The pain is usually felt in the groin and on the outer side of the hip, but it can also radiate from the front of the thigh to the knee. In some patients, the pain may be accompanied by a sticking or clicking sensation in the groin. After the initial painful period, there may also be a period of complete painlessness. At first, the pain increases after sports or heavy work, but if hip impingement is left untreated during this period, the damage to the joint increases.
The pain-free period decreases and patients begin to complain of constant groin, hip and leg pain. This results in calcification of the hip joint. In hip arthritis, joint movements are restricted, difficulty in walking and limping occur. The pain may occur not only during movements but also at rest and at night. Patients with this condition can only be helped by hip replacement surgery.
How is hip impingement diagnosed?
Knowledge and experience with hip impingement disease has increased considerably in the last ten years. In the past, the appearance of glass and pincers on hip X-rays did not attract attention. It can still be overlooked by specialists who do not deal with this subject.
Unfortunately, this situation results in calcification in the joint due to the fact that patients cannot be treated in the early period. In fact, since patients with hip impingement disease are treated with diagnoses such as herniated disc, inguinal hernia, knee meniscus problem, the time between diagnosis and treatment can be prolonged.
An orthopedic doctor experienced in hip problems usually suspects hip impingement disease after listening to the patient’s history and performing an examination. Glass and pincer-type deformities can be detected on hip X-rays. Magnetic resonance imaging (MRI) can be used to evaluate the cartilage and labrum and to make a differential diagnosis for diseases such as avascular necrosis of the femoral head. Hip joint ultrasound can be used to dynamically evaluate hip impingement. At the same time, tears and paralabral cysts, especially in the outer side of the labrum, can be detected by ultrasound and, if necessary, diagnostic injections can be performed. Sometimes, in the early stages of hip impingement disease, no significant findings may be detected on MRI. In this case, detailed examination and X-ray evaluation provide the most valuable data in the diagnosis of hip impingement disease.
Treatment of hip impingement disease
The first step in the treatment of hip impingement disease is to take some precautions to reduce hip impingement. These include not squatting on the floor, not sitting in a low seat, not turning the hip inwards or outwards or avoiding excessive bending towards the body, avoiding strenuous sports activities and losing weight. During the painful period, rest, various painkillers and some anti-inflammatory medications can be used. Afterwards, a physical therapy and exercise program is recommended. In mild cases, platelet-rich plasma injection known as TZP or PRP can be applied to the hip joint and labrum under ultrasound guidance. Closed surgical treatment with hip arthroscopy is performed in cases that do not respond to the measures and treatments taken, or in cases where significant tear or cartilage damage is detected in the labrum.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is knee arthroscopy?
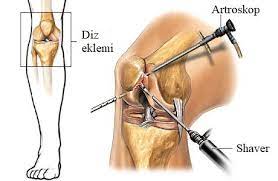
The word arthroscopy is derived from the ancient Greek words arthros (joint) and scopos (to look). Today, it is a closed surgical method applied by orthopedic physicians that enables the detection and treatment of damaged tissues by viewing the image of the inside and around the joints on the screen. In the past, open joint surgery called arthrotomy was used to gain access to the knee joint. A large incision was made in the knee, the kneecap was removed and the joint was exposed. This was a traumatic surgery that resulted in cutting the tissues around the knee and left patients in pain and with difficulty moving after surgery. The arthroscopic surgery method developed to solve this problem is a minimally invasive technique, meaning that it allows surgical treatment to be performed without damaging the surrounding tissues.
For knee arthroscopy, small skin incisions are made in two places on the knee. Through one of the incisions, a pen-sized arthroscope tool with a video camera inside and surgical instruments through the other, the orthopedic doctor performs the surgical procedure by watching the structures inside the knee joint on a screen. With arthroscopic surgery, patients recover more easily as a result of the treatment applied without damaging the tissues.
Generally, knee arthroscopy is applied for two purposes. The first is diagnostic arthroscopy, in which the orthopedic physician examines the structures inside the knee and identifies the problem causing pain. If there is no damaged or problematic condition within the joint, the procedure can be terminated. However, if a problem such as a meniscus tear is detected, the physician performs the necessary surgical intervention. This surgical procedure is called interventional arthroscopy. Since arthroscopy is performed through small incisions, it is less painful than open surgery and the recovery time is much shorter.
Knee joint structure
Your knee is the largest joint in your body and one of the most complex. The structures that make up the knee joint;
- Bones: The lower end of the thigh bone (femur), the upper end of the shin bone (tibia) and the kneecap (patella).
- Meniscus Menisci are thick, half-moon-shaped cartilaginous pads. There are 2 menisci in the knee, one on the inside and one on the outside of the joint. They act as “shock absorbers” between the femur and tibia bones, spreading and balancing the pressure on the joint.
- Ligaments The tissues that connect the bones to each other are called ligaments. The four main ligaments in the knee hold the bones together and keep the knee stable. These ligaments are the inner lateral ligament on either side of the knee, the outer lateral ligament and the anterior cruciate ligament and posterior cruciate ligament in the inner middle part of the knee.
- Articular cartilage: The ends of the femur and tibia and the back of the patella, the surfaces that make up the knee joint, are covered with articular cartilage. Thanks to the smooth and slippery texture of the cartilage, during the movements of the knee, the bones slide smoothly over each other and move comfortably without friction.
- Synovium: The knee joint is surrounded by a thin layer called the synovium. This membrane secretes synovial fluid, which lubricates the cartilage and reduces friction during movement.
In which cases is knee arthroscopy performed?
Knee arthroscopy is a closed surgical method that can be performed by an orthopedic physician in the diagnosis and surgical treatment of many problems that damage the cartilage surface and other soft tissues of the knee joint.
Diagnostic arthroscopy of the knee is performed to determine the cause of persistent knee pain or knee pain that cannot be explained by X-ray and magnetic resonance imaging (MRI) findings.
Although MRI is a highly sensitive radiologic imaging method, sometimes knee joint problems not seen on MRI are detected in diagnostic knee arthroscopy. Another important advantage of diagnostic knee arthroscopy is that the orthopedic surgeon can perform both diagnosis and surgical treatment in the same session.
Conditions where knee arthroscopy is applied
- For diagnostic purposes in detecting a problem in the knee joint
- Meniscus tear repair
- Removal of the torn section of the meniscus
- Anterior cruciate ligament reconstruction
- Posterior cruciate ligament reconstruction
- Removal of thickened synovial membrane
- Removal of thickened bands (plica)
- Correction of damaged cartilage surfaces
- Removal of bone or cartilage fragments inside the joint
- Reduction of intra-articular fractures
- Treatment of knee cap problems
- Treatment of knee joint infection
- In knee joint calcification, the particles that cause sticking in the joint are removed and the joint is cleaned.
Knee arthroscopy surgery
Knee arthroscopy can be performed under spinal (numbing of the lower back) or general anesthesia. For knee arthroscopy, small skin incisions are made in two places on the knee. Through one incision, a pen-sized arthroscope tool with a video camera is inserted and through the other, surgical instruments are inserted to access the inside of the knee. Light is shone into the joint through the arthroscope and the image of the inside of the knee is transferred to a screen. The orthopedic doctor performs the surgical procedure by watching the structures inside the knee joint on the screen. The duration of the surgery varies depending on the problem in the knee and the surgical procedure to be performed. Most knee arthroscopy surgeries take less than an hour. When the knee arthroscopy surgery is complete, the small incisions are usually closed with a simple stitch or covered with a bandage. As these incisions are very small, they will heal quickly.
Knee arthroscopy is usually a day surgery that does not require hospitalization. Once the patient is fully recovered from the anesthesia, they can go home the same day. Most patients need a cane with a brace or other assistance after arthroscopic surgery. The orthopedic surgeon will inform the patient when and how much weight can be placed on the foot depending on the surgical procedure. Although recovery after knee arthroscopy is much faster than recovery from traditional open knee surgery, it is important to follow the doctor’s instructions after returning home. The home exercise program prescribed after surgery should be followed regularly. Exercise will help both to increase knee movement and to strengthen the muscles around the knee. Recovery time after knee arthroscopy depends on the problem in the knee and the surgical procedure performed. For example, the recovery time after arthroscopic meniscus surgeries is 1-2 weeks in cases where only the torn part is removed, and 4-6 weeks after meniscal tear repairs.
Risks and complications of knee arthroscopy
The complication rate after arthroscopic surgery is lower than open surgery. However, as with any surgical procedure, there are potential risks and complications. These are usually lower in arthroscopic procedures. Sometimes the damage to your knee can be so severe that it cannot be completely reversed by surgery. Risks associated with knee arthroscopy include anesthesia risks, pain, limitation of movement, swelling in the joint, blood collection in the joint, infection, thrombophlebitis, cartilage damage, nerve damage.
Conclusion
Knee arthroscopy is a closed surgery method that is successfully used in both diagnosis and treatment of many knee problems. Since arthroscopy is a minimally invasive technique performed through small incisions, it does not damage the surrounding tissues. For this reason, patients are less painful after knee arthroscopy surgery and start moving in a short time. Most patients return to their old life in a short time after knee arthroscopy.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Meniscus Tears

Meniscus tears are one of the most common knee injuries. Although they are more common in people involved in sports, meniscus tears can occur in anyone, including children. A hard tackle on the soccer field can cause a meniscus tear, as can standing up quickly from a squatting position or making a sudden rotational movement while the foot is stationary. Patients with meniscal tears usually have symptoms such as knee pain, swelling, a feeling of locking and difficulty in fully extending the knee.
Structure and function of the menisci in the knee
In the knee joint, there are two C-shaped cartilaginous structures called menisci between the thigh and tibia, one on the inside and one on the outside. Menisci perform more than one task in the knee joint. First of all, they ensure that the two different bone ends that make up the knee joint fit together. They also increase the contact area in the joint, allowing the load on the knee to be distributed over a wider area and protecting the articular cartilage from high pressure. In addition, the menisci support the knee by preventing movements such as excessive sliding or rotation of the knee.
Damage and tearing of the meniscus can occur as a result of movements that overstrain the knee, sudden rotation and bending of the leg. The meniscus can be injured and damaged in different ways in many people from young to old. While meniscus tears usually occur in young people as a result of sudden movements, meniscus tears can occur in the elderly due to the wear and tear that has developed over the years, as a result of mild strain or even without strain. Meniscal tears lead to calcification of the knee joint over time. For this reason, it is extremely important for the health of the knee joint that follow-up and appropriate treatments are done on time and not to be late.
How do meniscal tears occur in the knee?
Direct injuries: These are injuries that occur as a result of direct blows to the knee. Falling on the knee, traffic accidents, direct blows to the knee during sports can cause this type of meniscus injury.
Indirect injuries: These are injuries that occur as a result of the torso rotating on the knee. In such cases, the knee joint and meniscus are damaged as a result of the body rotating on the knee while the foot is fixed on the ground. Uncontrolled rotation of the body on the knee due to loss of balance or tripping can also cause indirect injury to the meniscus.
Degenerative tears: With aging, calcification of the knee joint and wear and tear of the meniscus can occur. In older people with this condition, even a slight strain on the knee can cause a meniscus tear.
Is a torn meniscus always painful?
The pain caused by a torn meniscus may vary depending on the condition. Patients with a torn meniscus usually have symptoms such as knee pain, knee locking and swelling. The pain may become more pronounced when the knee is bent or weight is placed on it. Although most meniscal tears usually cause knee pain, tears that occur spontaneously or with mild strain may sometimes go unnoticed, especially in people who have arthritis in the knee with aging and wear and tear in the menisci.
Symptoms of a meniscus tear
Although it varies in each patient, the symptoms of a meniscus tear are generally as follows;
- Sudden onset of pain in the knee
- Sudden increase in previous pain in the knee
- Swelling and tenderness in the knee
- Sticking sensation in the knee
- Locking sensation in the knee
- Difficulty in bending and unbending the knee
- Difficulty walking, squatting, climbing up and down stairs
How is a meniscal tear in the knee diagnosed?
In order to diagnose a meniscal tear in the knee, the patient’s medical history, physical examination findings and appropriate radiological imaging methods should be evaluated together.
Medical history: Information is obtained about the exact location of the patient’s pain, how and when the pain started, during which activities the patient has difficulty, previous surgeries or previous treatments.
Physical examination: During the examination, the orthopedic doctor checks the patient’s knee joint, movements and gait. In addition to knee swelling, tenderness, range of motion and some special examination tests, a hip examination may also be performed for the differential diagnosis of pain reflecting from the hip to the knee.
X-ray An X-ray is a radiologic examination to see the bone structures and alignment in the knee. Even if the orthopedic doctor suspects a meniscus tear, he/she may order a knee x-ray first or in combination with other imaging to assess the amount of wear in the knee and to see if there is any other problem in the bone structures.
Magnetic resonance imaging (MRI): In general, the gold standard for diagnosing and evaluating a meniscal tear is magnetic resonance imaging of the knee. MRI imaging provides information about the location, shape and size of the meniscus tear. It also shows conditions such as cartilage damage or intra-articular swelling caused by a meniscal tear. It can also be monitored for problems in other structures outside the meniscus.
Advantages of MRI in the diagnosis of a meniscal lesion;
- It plays an important role in treatment planning by determining the location, type, position and extent of the tear.
- Other intra-articular structures (cartilage, ligaments, etc.) can also be evaluated.
- It also allows extra-articular structures to be seen.
- Radiation free.
Why is the location, type and shape of meniscal tears important?
In order to choose the most appropriate treatment for meniscal tears, accurate visualization of the location, shape, type and size of the meniscal tear is essential. In young, active people, if the location of the meniscal tear is on the outer side with good meniscal blood supply, meniscal repair is performed. Similarly, meniscal root tears should also be repaired. Most young athletes return to active sports life after meniscal repair. If the patient is elderly, or if the meniscus tear is on the inner side where blood supply is poor, or if the meniscus tear is too fragmented to be repaired, then the damaged section must be cut out. Types of meniscal tears include horizontal, longutudinal, radial, vertical, bucket handle, root tear and complex tears.
Types of meniscus tears
What are the options in meniscal tear treatment?
The treatment of meniscal tears varies depending on the shape, size and location of the tear and the patient’s complaints. Surgery is recommended for significant tears that negatively affect the integrity of the knee and other structures, especially cartilage, within the joint.
In the treatment of degenerative and small meniscal tears that are thought not to damage the joint and cartilage, non-surgical treatment options are primarily evaluated. However, if there is no response to these, surgery is considered.
Treatment of meniscal tears varies depending on the shape, size, location and complaints of the patient. Surgery is recommended for significant tears that adversely affect the integrity of the knee and other structures, especially cartilage, within the joint.
In the treatment of degenerative and small meniscal tears that are thought not to damage the joint and cartilage, non-surgical treatment options are primarily evaluated. However, if there is no response to these, surgery is considered.
Non-operative treatment methods for meniscal tears
- Rest: The knee joint is rested by avoiding movements that aggravate knee pain.
- Cold application: To reduce swelling and pain, cold can be applied to the knee 4-5 times a day for 20 minutes over a thin towel.
- Drug treatment: Painkillers and non-steroidal anti-inflammatory drugs may be used as recommended by the doctor.
- Physical therapy: Strengthening the muscles and ligaments surrounding the knee and legs can help increase range of motion and improve balance in the knee joint.
- Exercise A proper exercise program, started after the knee pain has subsided, helps to maintain long-term knee health.
- Intra-articular injections: Intra-articular injections may be preferred to reduce inflammation and relieve pain. In appropriate cases, platelet-rich plasma, known as TZP or PRP, taken from the patient’s own blood and prepared through a special process, can be injected into the joint and the outer edge of the meniscus.
Successful clinical results are obtained especially after ultrasound-guided TZP injections.
Surgical treatment methods for meniscal tears
Arthroscopic closed meniscus surgery is recommended for degenerative and small tears that do not resolve complaints such as knee pain, knee locking or limitation of movement despite other non-surgical treatment methods or for large meniscal tears that damage the articular cartilage. Meniscal surgery varies according to the condition of the damage and the patient. In some cases it is possible to repair a torn meniscus, especially in children and young people. The highest success in the surgical treatment of meniscal tears with knee arthroscopy is achieved in cases where the anterior cruciate ligament is intact and there is no wear in the cartilage tissue.
- Arthroscopic partial meniscectomy
If the location and type of meniscal tear is not suitable for repair, arthroscopic partial meniscectomy, a closed surgical technique in which only the torn part of the meniscus is cut and removed, is preferred.
Arthroscopic partial meniscectomy surgery aims to remove the torn and damaged part of the meniscus, leaving as much healthy meniscal tissue as possible. Patients usually recover quickly after arthroscopic partial meniscectomy surgery. They can immediately start to load on the operated leg and return to their daily lives in a short time.
- Arthroscopic meniscal repair
The menisci are not unimportant, as once stated, but rather are extremely important structures of the knee joint and have important roles in knee joint biomechanics. After meniscal injuries, the meniscus should be preserved and anatomically repaired, contrary to past practice.
Meniscal repair is a surgical procedure that involves suturing the torn meniscus. Meniscal repair allows the knee to regain its normal anatomy and, when the surgery is successful, provides good long-term results. However, meniscal repair is a major operation and the return to daily life is slightly longer compared to meniscectomy.
- Meniscus transplant
In patients whose menisci are severely damaged and need to be completely removed, transplantation of meniscal tissue has been introduced to prevent wear on the knee. Frozen meniscal tissues from cadavers are transplanted to the patient after being tested to prevent disease transmission.
Conclusion
Meniscal tear in the knee should not be considered only as an athletic injury. Meniscal tears and damages are an orthopedic problem that can be seen in all age groups. Depending on the location, shape and severity of the meniscus tear, treatment options vary from home medication and rest to various meniscus surgeries. With the right diagnosis and early treatment, your knee can regain its previous mobility and function
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Rejeneratif Ortopedi

Rejeneratif yani yenileyici tıp; hasar gören veya işlevini yitiren dokuyu onarmak için fonksiyonel hücreleri uyaran, doğal iyileşme sürecini canlandıran bir yöntemdir. Kök hücre uygulamaları, kısaca TZP veya PRP olarak bilinen trombositten zengin plazma enjeksiyonları, proloterapi gibi tedaviler, kas-iskelet sisteminde onarıcı hücrelerin uyarılmasına ve iyileşme sürecinin hızlanmasına yardımcı olur. Başta eklem kireçlenmesi ve kıkırdak hasarları olmak üzere pek çok kemik, kas, eklem ve bağ sorunlarında rejeneratif enjeksiyon yöntemleri uygulanabilir. Rejeneratif uygulamalarda hastaya uygulanan solüsyon yine hastanın kendi doğal kanı veya dokusundan elde edildiği için, vücudun ret etmesi veya alerjik yan etki yapması gibi durumlar meydana gelmez.
*Sayfa içeriği sadece bilgilendirme amaçlıdır. Tanı ve tedavi için mutlaka doktorunuza başvurunuz.
Hand Surgery

Our hands are structures in which many tissues work together in harmony and play an important role in our daily functions, communication and artistic skills. In order to maintain this complex structural and functional health of our hands, injuries, disorders and all painful conditions should be evaluated appropriately. Delay in the treatment of many hand problems that are considered simple can cause serious consequences that will affect the quality of life of the person. Hand surgery is the department that deals with the diagnosis and treatment of all kinds of injuries, deformities and painful conditions of the forearm, wrist, hand and fingers. The main aim of hand surgery is to restore the movement and function of the wrist, hand and fingers.
- Conditions in which hand surgery is frequently performed;
- Fractures and dislocations of the bones of the hand and forearm
- Soft tissue, ligament, tendon, nerve injuries of the hand
- Hand and finger deformities as a result of trauma or paralysis
- Persistent nerve compression, tendon and ligament problems
- Congenital hand and finger defects
- Osteoarthritis in the wrist and hand joints
- Infection, tumor in the hand
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is Nerve Compression in the Hand (Carpal Tunnel Syndrome)? What are the Symptoms and How is it Treated?
In daily life, do you feel pain in your wrist when you try to hold and lift some objects such as a teapot? When you try to hold a coffee cup, do you feel that your hand is not as strong as it used to be and do you feel like dropping it? Do you experience hand numbness that wakes you up at night? All these discomforts can be caused by carpal tunnel syndrome, which is common in the society and known as nerve compression in the hand.
Symptoms of carpal tunnel syndrome are usually seen as pain in the wrist, numbness and tingling in the fingers. However, you should consult a doctor before the symptoms of carpal tunnel syndrome start to affect your activities and sleep patterns. When carpal tunnel syndrome is left untreated, numbness, numbness and weakness may occur due to permanent nerve and muscle damage in the hand.
What is Carpal Tunnel Syndrome?
The medical name of the condition, which is generally known as nerve compression in the hand, is carpal tunnel syndrome. In our wrist, there is a narrow tunnel-like channel covered with bones on one side and connective tissue on the other. This channel is called “carpal tunnel”. The nerve known as the median nerve, which passes through the carpal tunnel, controls the movement of the fingers of the hand and especially the sensation in the first three fingers. As a result of the narrowing of the carpal tunnel to put pressure on the median nerve passing through it; it causes complaints such as pain, numbness, tingling and weakness in the hand. This emerging picture is known as “Carpal Tunnel Syndrome”.
What Causes Carpal Tunnel Syndrome?
Although the cause of nerve compression in the hand is not known exactly, there are some conditions that cause it to occur. Especially advancing age and gender are risk factors for carpal tunnel syndrome. The carpal tunnel area is relatively smaller in women than in men. Therefore, nerve compression in the hand may be more common in women.
Some of the causes and risk factors for carpal tunnel syndrome are as follows:
- Diabetes (diabetes),
- Pregnancy
- Obesity (obesity),
- Wrist fractures,
- Rheumatic diseases such as rheumatoid arthritis,
- Hypothyroidism (underactive thyroid gland),
- Mass formation in the carpal tunnel,
- Repetitive hand-wrist movements at home, at work, in sports,
- Use of vibrating tools or machines at work.
What are the Symptoms of Carpal Tunnel Syndrome?
Symptoms of carpal tunnel syndrome usually appear gradually. Complaints become more pronounced and progressively worse over time. Symptoms of nerve compression in the hand typically manifest themselves as one or more of the following:
- Burning, tingling or numbness in the palm and especially in the thumb, index and middle finger,
- Hand and wrist pain, numbness or tingling sensation that wakes you from sleep at night, partially relieved by shaking your hand,
- Numbness and tingling when holding the wrist in a fixed position, such as when driving a car or reading a book,
- Pain radiating from the wrist up the arm,
- Difficulty holding or grasping objects due to weakness in the hands and fingers,
- Numbness and tingling sensations that occur with repetitive movements such as knitting or dyeing,
- In advanced cases of carpal tunnel syndrome, the appearance of collapse as a result of weakening of the muscle on the palm side of the thumb.
The symptoms of a pinched nerve in the hand are quite specific. However, there are other neuropathies (nerve disorders) or degenerative conditions such as osteoarthritis of the hand that can cause similar symptoms. In order to determine the right steps in the treatment of carpal tunnel syndrome, an examination and evaluation by a doctor is necessary.
How is Carpal Tunnel Syndrome Diagnosed?
For the diagnosis of nerve compression in the hand (carpal tunnel syndrome), the patient’s complaints and history should first be learned. It is important to learn about the onset and duration of the complaints, the conditions that increase the complaints and other health problems, if any. A detailed examination of the patient is then performed.
To clarify the diagnosis, some tests specific to carpal tunnel syndrome are requested. With these tests, it is checked whether the complaints increase or not. Motor and sensory examination is used to check for muscle weakness and sensory deficits in the hand. If the physical examination supports the suspicion of carpal tunnel syndrome, electrophysiological tests are used to confirm the diagnosis. Electromyography, or EMG as it is also known, is performed. This diagnostic method determines the degree of nerve compression in the carpal tunnel by measuring nerve conduction velocities and evaluating the strength of the muscles. Since some other nerve and muscle diseases can also be detected during EMG, it is a guide in differential diagnosis.
An important point is to differentiate carpal tunnel syndrome from pain caused by neck hernia, spine, shoulder or elbow. If the patient has complaints related to these areas other than the wrist, it is useful to evaluate these areas with radiological imaging methods such as X-ray, magnetic resonance imaging (MRI), ultrasound in order to determine the actual source of the problem. In cases such as rheumatic disease, diabetes or goiter that cause carpal tunnel syndrome, various blood tests are required.
What are the Treatment Options for Carpal Tunnel Syndrome?
There are various surgical and non-surgical treatment options for the treatment of carpal tunnel syndrome to relieve pain in the hand and numbness in the fingers. Depending on your complaints and the degree of nerve compression, follow-up is started with the appropriate treatment. The aim of the treatment of carpal tunnel syndrome is to reduce and eliminate the conditions that cause compression and damage to the median nerve in the carpal tunnel.
Non-Surgical Treatment Options
Some of the non-surgical treatment methods for carpal tunnel syndrome are as follows:
Rest: Taking a break from repetitive movements that strain the wrist for a while will alleviate the numbness and painful process.
Medication: Various medications are used to reduce pain and pain caused by nerve compression. However, it should be kept in mind that medication does not eliminate the actual problem. Medications can be used on a short-term basis according to the doctor’s recommendation.
Using a wrist splint: A wrist splint (wrist brace) keeps the wrist in its natural position during movements in daily life and while sleeping at night. The wrist and the surrounding muscles, ligaments and joints are kept in the ideal position. Thus, there is less pressure on the tendons and nerve passing through the carpal tunnel and complaints are reduced. It may be recommended to use the wristband for a few weeks during daytime activities and at night when going to bed.
Cold application: One of the methods used in the treatment of carpal tunnel syndrome is cold application. Cold contributes to the reduction of swelling in the wrist and the relief of pain sensation. Cold application can be done 3-4 times a day for a period of 15-20 minutes. In order to avoid a rash-like reaction to cold on your skin, you should avoid direct contact of the ice with the skin. The cold pack can be applied by wrapping it with a thin towel or sheath.
Making changes in daily life: Although the complaints related to carpal tunnel syndrome can be controlled with various methods, the person may need to make some changes in their daily life or change their habits to prevent recurrence. Those who use vibrating tools such as drills should take more frequent breaks from their work. Office workers are advised to use ergonomic keyboards and supportive mousepads when using computers.
Injection treatment for carpal tunnel: In the treatment of carpal tunnel syndrome, when rest, use of wrist bracelets, cold application and medication do not respond, injection therapy is considered.
Physical therapy and exercise: Patients diagnosed with carpal tunnel syndrome are recommended a physical therapy and exercise program along with non-operative treatments. In addition, if necessary, a physical therapy program is also applied after surgery, increasing the mobility of the nerve and enabling the patient to use his/her hand comfortably.
Carpal Tunnel Syndrome Surgery
Not every patient needs carpal tunnel syndrome surgery. Carpal tunnel surgery becomes an option when non-surgical treatment options are not useful, when complaints begin to recur in a short time and in advanced cases such as melting of the muscles around the thumb due to nerve compression.
In carpal tunnel syndrome surgery, an incision of approximately 3-4 centimeters is made on the inside of the wrist. Then, the connective tissue forming the upper wall of the carpal tunnel is loosened and the structures passing through the tunnel are allowed to move freely.
After this procedure, which is usually performed under local anesthesia, the patient goes home the same day. Stitches are removed after 10-15 days. After the stitches are removed, massage is recommended to prevent stiffness at the wound site and an exercise program is recommended to regain the range of motion of the wrist.
Carpal Tunnel Syndrome During Pregnancy
In the later stages of pregnancy (usually starting from the 6th month), excess fluid (edema) accumulated in the body, which manifests itself as swelling in the hands and feet, creates pressure in the carpal tunnel in the wrist and compresses the structures passing through the tunnel. Compression of the median nerve in the carpal tunnel causes complaints such as numbness, tingling and pain in the hands and fingers.
As the edema in the body decreases after delivery, the pressure in the carpal tunnel will also decrease and the complaints usually disappear. Surgery may rarely be required. In order to reduce the complaints in the period until birth, it is recommended to rest from the non-surgical methods we mentioned, to use wrist braces, to apply cold, to do appropriate exercises and to stay away from movements that require bending the wrist. Carpal tunnel syndrome may occur due to many reasons and may also cause different complaints.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hand Thumb Root Joint Calcification
The thumb root joint of the hand is called the carpometacarpal (CMC) joint. The surface of the trapezoidal and first metacarpal bones that form the CMC joint in the hand is covered with cartilage. The function of the cartilage tissue is to allow the joint to glide and move easily. Osteoarthritis is a joint disease characterized by wear of the cartilage, adjacent bones and soft tissues, leading to joint pain and difficulty in movement. The movement and strength of the thumb in the hand is necessary in almost every activity; such as writing, opening a jar lid, buttoning a button. In the case of thumb root joint calcification, pain in the hand and difficulty in gripping and grasping prevent daily tasks.
– In women over 40 years of age
– With aging
– Repetitive movements of the thumb joint
– Presence of hand thumb root joint arthritis in the family
– Looseness of the ligaments of the thumb joint
– History of injury to the ligaments of the thumb joint
– Misalignment of the thumb bones
– History of previous thumb fracture
Who has arthritis of the thumb root joint?
Thumb root osteoarthritis is more common after the age of 40 and in women. Thumb root osteoarthritis often develops in both hands. The symptoms may even be more common in the non-dominant hand. It is thought that this condition is not related to the specific activities that the person performs, but has genetic or anatomical causes. Joint calcification causes friction during thumb root joint movements as a result of the wear of the cartilage at the mutual bone ends and narrowing and deformation in the joint, and its movements are limited over time. Thumb root joint calcification causes pain, limitation of movement and functional difficulties in the hand.
What are the symptoms of thumb root joint arthritis?
Patients complain of pain, swelling, stiffness, deformity and limitation of movement in the thumb root joint. Generally, there is tenderness and crunching sound in the BMC joint. In patients with thumb root joint arthritis, a bony tapering may develop outward at the wrist level of the 1st finger and a square appearance may occur in the hand.
Thumb root osteoarthritis can also be detected on X-rays before symptoms appear. Even if the patient feels little pain, it is possible that the arthritis is relatively advanced. This can partly be explained by the fact that the person changes his or her activities to accommodate the painful finger. However, this can result in less use of the hand and loss of strength.
Diagnosis of thumb root joint arthritis
In the examination, the patient’s strength between the thumb and index finger (pinch force), joint movements and the condition of the surrounding connective tissues are evaluated.
X-rays are taken to see the effect of calcification on the joint and bone structure. In advanced cases of thumb root joint arthritis, narrowing of the joint space and deformity are seen. Ultrasound can also be used to assess the condition of the soft tissues around the BMC joint.
How is thumb root joint arthritis treated?
The treatment method is decided by evaluating whether the complaints due to thumb root joint arthritis increase with daily activities, the pain condition and the patient’s expectations together. In addition, the natural course of the disease also affects the treatment. Some patients say that they can live with the condition but want temporary pain relief, while others say that they cannot use their hand as it is and want a radical approach.
The aim of treatment of thumb root osteoarthritis;
– Reduce pain, stiffness and inflammation
– Maintaining joint range of motion
– Reducing stress on the joint
– Increasing the function of the hand
– Preventing causes that can increase calcification
Non-surgical treatment of thumb root joint arthritis
In periods of intense pain due to thumb root joint arthritis, it is useful for patients to partially rest the joint by using a splint that supports the wrist and thumb. Various pain and anti-inflammatory (NSAID) medications can be taken, as well as intra-articular cortisone injections. Although this injection reduces pain and swelling, it often provides lasting relief that lasts for several months.
For a longer lasting effect, TZP (platelet-rich plasma), derived from the patient’s own blood, can be injected into and around the joint. Especially TZP injection into the joint and surrounding soft ligaments and soft tissues under ultrasound guidance gives clinically satisfactory results. Physical therapy and exercise program may be recommended according to the condition.
Surgical treatment of thumb root joint arthritis
Surgery is recommended in cases where non-surgical treatment of arthritis of the thumb root joint fails to relieve the pain and increases the loss of function. The surgical procedure usually provides excellent pain relief, but the degree of function and strength may vary. The most appropriate surgical method for the condition of the joint can be decided together with the orthopedic doctor. These surgeries are day surgery procedures that do not require hospitalization. After the surgery, a physical therapy and rehabilitation program is recommended for a varying time and duration depending on the technique applied.
There are various surgical techniques for thumb root joint arthritis;
Arthroscopic debridement: In cases where joint calcification has not progressed much, the joint is intervened into the joint with closed surgery. Cartilage fragments inside the joint are removed.
Resection arthroplasty: Partial or complete removal of the trapezoidal bone, which forms the base of the finger root joint, with reorientation of the tendon next to the thumb.
Joint fusion: The two bones forming the joint are frozen end to end. This operation relieves joint pain, but restricts movement.
Interpositional arthroplasty: It is performed by removing the worn parts on the joint surface and inserting soft tissue such as fascia-tendon or graft. The advantage is that there is a reduction in pain and no restriction in movements.
Joint implants and prosthesis: Joint surgeries with implants are not yet very reliable for this condition. Studies on new techniques and implants are ongoing.
Conclusion
Thumb root joint calcification is a condition that is more common especially in women over the age of 40 and causes pain and restriction in movements of the hand such as grasping, holding and pinching. Thumb splints and ultrasound-guided injections are beneficial. Successful results are also obtained with surgical methods applied in thumb root joint calcification.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Flatfoot in Adults
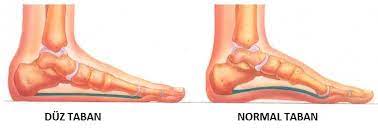
Flat feet, also known as pes planus, is a common condition in society. It can be caused by abnormal bone and joint structure of the foot, such as congenital tarsal coalition, or by soft tissue problems such as laxity in ligaments or weakness in muscles. Flatfoot in adults, on the other hand, is either the absence of the inner arch of the sole of the foot in childhood, which continues in adulthood after skeletal development is completed, or the loss of the inner arch of the foot due to some reasons that develop later.
Who has adult flatfoot?
- Those with flexible flatfoot in childhood
- People with loss of tendon function
- In traumatized people
- People with inflammatory joint rheumatism
- People with neurological diseases
- In the presence of tarsal coalition
What are the signs of flatfoot in adults?
The main finding in flatfoot is the loss of the longitudinal foot arch on the inner side. However, in adult flatfoot, this may be accompanied by pain, deformity, swelling and loss of function. The typical appearance of flatfoot is that the arch of the foot disappears and the heel turns outward when the foot is loaded. In people with flexible flatfoot, the arch of the foot disappears in the loading position, while the shape of the foot is normal when it is not loaded and the arch of the foot is present. Most people with flexible flatfoot do not have pain and limitation of function.
What are the causes of flatfoot in adults?
Flatfoot caused by subsequent loss of tendon function is one of the important causes of flatfoot in adults. Patients with tibialis posterior tendon insufficiency may experience pain in the inner and posterior part of the foot, swelling and tenderness in the inner part of the foot, early fatigue and loss of function in the foot.
Tibialis posterior tendon insufficiency can develop as a result of trauma, as well as inflammatory rheumatic joint diseases, joint calcification, neurological diseases and diabetes. Fractures and dislocations involving the foot and ankle are the cause of trauma-related flatfoot. In addition to the symptoms of flatfoot in these patients, symptoms such as limitation of movement, pain, swelling, tenderness and loss of function due to wear and calcification in other joints may also be observed. Weakness in the foot muscles plays a major role in flatfoot that develops due to neurological diseases. In flatfoot caused by such neurological conditions, muscle spasms or muscle weakness, neuropathic pain findings in the foot (burning, electrification, pins and needles, tingling) and sensory loss may also be observed.
How is flat feet diagnosed in adults?
Flatfoot is diagnosed by physical examination and radiologic imaging methods. The orthopedic doctor examines the external appearance of the foot from the back, front and bottom while the person is standing and sitting on the examination table. The foot is checked for skin findings such as callus formation due to abnormal load balance. Joint range of motion is checked. Especially the strength and endurance of the tibialis posterior muscle is evaluated. The position of the heel and arch of the foot while standing is evaluated. If the arch of the foot is formed by standing on tiptoe or lifting the thumb upwards; flexible flatfoot is diagnosed. If the arch does not occur with standing on the toe or lifting the thumb upwards; rigid flatfoot should be considered.
X-ray and ultrasound examinations of the patient’s foot may also be requested. In addition, foot base image called podography and digital pressure analysis are performed. Computed tomography and magnetic resonance imaging examinations may be requested if necessary.
Flatfoot problem and treatment in adults
Treatment options in adult flatfoot are primarily non-surgical treatment options, as in most orthopedic diseases, and surgical treatment if success is not achieved.
If there is no complaint despite flat feet in adults, there is no need for treatment. However, they may be advised to use appropriate shoes and not to gain excess weight. In the first stage in patients with complaints; activity modifications, weight loss, exercises, insoles, ice applications, drug treatments and physical therapy can be applied.
In the problem of adult flatfoot, digital foot sole analysis can be performed with today’s modern technology. The data obtained is digitally transferred from the computer to the automatic insoles making machine. Thus, patient-specific and the most suitable insoles for the patient’s foot structure can be produced.
Treatment of flatfoot in adults
If complaints of flatfoot in adults persist despite all treatments, surgical treatment options should be reviewed. Depending on the cause and severity of flatfoot in adults, surgical treatment applications may vary as procedures on ligaments and tendons, i.e. soft tissue surgeries, and procedures on bones and joints, i.e. bone surgeries and their combination.
If non-surgical treatment options fail in patients with flexible flatfoot and complaints, bone surgeries may be required in surgical treatment. In bone surgeries, tendon lengthening surgeries are performed together with cutting and correcting the heel bone, while with the arthroeresis method, foot deformity can be improved with a block screw placed in the joint without bone incision.
Surgical treatment options in tendon insufficiencies may vary from cleaning the inflammatory tissue to tendon transfers in complete insufficiency depending on the severity of the insufficiency. However, in late cases, bone surgeries may also be necessary due to secondary bone and joint deformities and degenerations.
In adults, the main treatment option for flatfoot that develops due to trauma and subsequent, advanced joint destruction is arthrodesis, that is, permanent freezing of the movements of the joint by surgery.
Conclusion
Knee insoles are a common condition in society. Strengthening and stretching exercises for muscles and tendons are very effective in patients with flexible flat feet and pain complaints. Especially before deciding on surgical treatment for flexible flat feet, each patient should be included in an exercise and physical therapy program and should use insoles.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Achilles Tendon Rupture

The Achilles tendon is the largest and strongest tendon in the human body. Tendons are cords of tough tissue that connect muscle to bone. The Achilles tendon is located behind the heel and connects the heel bone to the calf muscle. It helps a person to walk, run and jump. Achilles tendon rupture usually occurs above where the tendon attaches to the heel bone. It often occurs in the 30-50s, during a sports activity.
Why does the Achilles tendon rupture?
Although the Achilles tendon is very strong, there is sometimes a risk of rupture due to certain diseases or the use of certain medications, even without heavy sports activities. The rupture usually occurs during overloaded activities such as running, sudden stops or jumping. In those who have had Achilles tendonitis for some time, the tendon may also rupture during activities such as walking or light running, depending on the weakening of the tendon.
What are the symptoms of Achilles tendon rupture?
People who rupture their Achilles tendon during sports usually describe the event as follows;
– At that moment, I thought I was kicked in the leg from behind with a loud ‘pop’ sound, but when I turned around, there was no one around me…
Patient complaints of Achilles tendon rupture
- Severe pain behind the ankle, making it difficult to walk
- Swelling and bruising behind the ankle
- Significant tenderness
- Inability to rise on tiptoes
- The space formed at the back of the ankle above the end of the tendon after a tear.
How is Achilles tendon rupture diagnosed?
A physical examination alone is usually sufficient to diagnose an Achilles tendon rupture. X-rays are taken to detect the presence of concomitant Haglund’s or other bony abnormalities. Ultrasound and magnetic resonance imaging tests are performed to determine the severity of the Achilles tendon rupture and the degree of separation of the fibers.
How is Achilles tendon rupture treated?
The Achilles tendon has a long healing process due to its relatively poor blood circulation. If a complete rupture of the Achilles tendon is not treated promptly and appropriately, the function of the tendon will be impaired. Normal daily activities such as walking cannot provide the leg strength necessary for running and other sports activities. In Achilles tendon ruptures, plaster treatment can be applied depending on the patient’s condition or surgical treatment can be performed by suturing and repairing the severed tendon ends.
Plaster treatment
With a cast applied to the foot and ankle, the ankle is immobilized in a certain position and the ends of the severed tendon are brought closer together. This allows the tendon to heal slowly over time. For the treatment of Achilles tendon rupture in this way, a cast or splint is usually used for 8-12 weeks.
Surgical treatment
Surgical treatment of Achilles tendon ruptures allows for a faster recovery and results in a much stronger tendon than plaster treatment. The risks associated with surgery are opening of the surgical wound due to poor blood circulation in this area and infection.
In cases where early recovery and early return is desired, especially in the treatment of Achilles tendon rupture in athletes; surgical intervention is preferred to provide a stronger tendon healing with a lower probability of rupture again.
Conclusion
Achilles tendon rupture can occur in athletes, in people who are not regular athletes, during a sudden, strenuous sporting activity at the weekend or in people with weakened tendons due to Achilles tendonitis. As soon as the rupture is diagnosed, treatment should begin immediately to prevent loss of strength and improper healing. A physical therapy and rehabilitation program is recommended before returning to sport or daily life.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
What is a big toe protrusion (bunion)?

Bunion (also known as hallux valgus) is the name given to the bump-shaped protrusion that forms on the edge of the big toe. The cause of the protrusion in the big toe is the angular deformity that develops in the forefoot and thumb. When this deformity and protrusion progresses over time, it causes pain and difficulty walking. Bunions with big toe protrusion are usually familial. Although bunions are more common in middle-aged or older people, more often in women, they can sometimes develop even in adolescence. The formation of a bone spur on the big toe is usually bilateral, meaning that it occurs on both feet.
What are the risk factors for developing a bunion – bone spur on the big toe?
You may be more likely to develop a big toe bone spur – bunion – in your foot if you have the following conditions:
- Family history of bunions
- Inherited foot structure problems such as flat feet
- Structurally excessively loose connective tissue
- Injuries leading to foot deformities
- Inflammatory rheumatic diseases such as rheumatoid arthritis, gout
- Various neuromuscular diseases
Why does a big toe protrusion-bunion develop?
If the ligaments connecting the bones in the foot are structurally loose or become looser with age, there is enlargement in the forefoot area. The combination of pressure on the big toe joint and ligament laxity causes a shift and deformity of the forefoot bone angles. Eventually, the angle of the big toe root bone shifts and a bony lump forms. Over time, this causes the big toe to bend towards the second toe.
The main reason for the formation of a bunion, a bony protrusion of the big toe, is the looseness of the ligaments that stabilize the joint between the first metatarsal and cuneiform bones at the level of the big toe. As a result of this looseness, the angle of the bone’s posture changes and shifts, resulting in deformity and bunion development. Standing for long periods of time and ill-fitting narrow shoes can worsen bunion pain, but they do not cause a thumb protrusion in the individual foot.
What are the symptoms of bunions?
- Clubbing, deformity of the big toe
- Red, hard swelling of the big toe root joint
- Difficulty wearing normal shoes
- Inability to bend the thumb or pain when trying to bend it
- hammer finger formation on the finger
- Callus development in deformed areas
- Feeling of numbness at the tip of the big toe.
What is the clinical course of bunion?
Redness and tenderness develops on the skin in the area of the bony prominence of the big toe and pain starts, which increases when wearing shoes. Since this area of the foot both bears the load and bends during each step, the pain intensifies with walking. Calluses may form at the base of the first and second finger roots. Over time, the thumb may bend towards the second finger. With the pressure from the thumb, the second finger is pushed up and a hammer finger may form. When the angular disorder increases, the tip of the first finger may even touch the third finger. This can lead to various painful problems in the other fingers (metatarsalgia, neuroma). When the bone spur of the big toe – hallux valgus – progresses, calcification also develops in the joint.
How are bunions diagnosed?
During the foot examination, hallux valgus can be diagnosed by seeing the thumb bone protrusion. The orthopedic specialist tries to determine the effect of the bunion on joint movement or whether there are conditions such as pain, looseness, numbness in the foot.
X-rays of the foot in some special positions are required to determine the condition of the joints and bone angles. If necessary, tests such as ultrasound (US), tomography (CT), magnetic resonance imaging (MRI), electromyography (EMG) may also be requested for different evaluations.
What are the non-surgical treatment methods for bunion-hallux valgus?
Painkillers: During periods of intense pain, swelling and tenderness, the use of painkillers recommended by the doctor together with regional cold application reduces complaints.
Physical therapy Treatment with physical therapy devices and exercises can reduce pain and maintain joint mobility. It can also help prevent the angulation from increasing rapidly by balancing the muscle forces in the foot.
Injections: Cortisone injections can reduce pain and swelling in the big toe joint, but can damage the tissues if given too often. Prolotherapy and TZP (or platelet-rich plasma, also known as PRP), which are regenerative orthopaedics methods, can be used under ultrasound guidance to reduce pain and tighten loose ligaments.
Bunion pads and taping: Various bunion pads can relieve the area and partially alleviate the pain.
Shoe changes: Soft shoes with a wide, deep toe box reduce pressure on the toes.
Orthotics: Some orthotics, such as insoles placed in shoes, can help with angulation problems that can contribute to bunion formation. Placing a silicone support between the big toe and second toe can be comforting.
What are the surgical treatment methods for bunion-hallux valgus?
If the complaints such as pain and walking problems disappear with the treatment methods applied in patients with big toe bone protrusion-bunion problem, the patients are followed up. However, surgery should be performed in patients whose complaints persist despite the necessary treatments being tried, in patients who have walking difficulties or in patients who have an increase in angular distortion during follow-up.
In which cases is bunion surgery performed?
Bunion pain that does not improve with non-surgical treatment methods
- Failure to relieve pain despite shoe changes
- Painful limitation of movement in the big toe
- Increased angular distortion of the big toe
- Leaning of the big toe towards the little toes
- Deformities that begin to affect the second toe of the foot, causing additional painful conditions in the foot
Surgical techniques for the surgical treatment of hallux valgus:
There are many different surgical techniques described so far to correct bunions. The orthopedist determines the surgical technique to be applied according to the patient’s age, the severity of the bunion deformity, the angles in the bones and joints of the foot, arthritis and experience.
Surgical Techniques:
- Repair of tendons and ligaments
- Bunionectomy
- Osteotomy
- Arthrodesis
- Resection arthroplasty
Recently developed new surgical techniques increase patient satisfaction after surgery, as they eliminate the joint problem that causes hallux valgus and deformity in the foot with a 3D approach. Lapidus 3D surgery offers a more permanent solution by correcting the deformity in 3 dimensions.
Recovery period after hallux valgus surgery
Toe bone spur-bunion surgeries are usually day surgery procedures, meaning that the operated patients return home the same day. The success of the surgery is also related to how well the orthopedic doctor’s instructions are followed at home during the first few weeks after surgery. Since maintaining the position of the finger is very important for a successful recovery, the instructions regarding dressing care need to be followed exactly.
Usually, foot movements are restricted with a splint or boot for two weeks after surgery to allow the tissues to heal. The use of crutches may be recommended to avoid stepping on the ground and full body weight bearing.
Big toe bone spur-bunion surgery risks and complications
Complaints such as pain, swelling and difficulty in movement are common after foot surgeries and decrease over time. Undesirable conditions such as infection, nerve damage, vascular thrombosis, blood clot in the lung, nonunion of the bone, and recurrence, which can be seen after every surgery, may develop, albeit rarely. If pain and deformation persist, additional surgeries called revision surgery may be necessary.
Conclusion
Bony protrusion of the big toe – bunion – is a common condition in the community. When comfortable and appropriate shoes are not worn, bunions can progress and worsen in a short time.
If your pain does not go away despite non-surgical treatments, you should consult an orthopedic doctor to understand your surgical options. An operation to correct the deformity of the big toe can relieve pain and difficulty in walking.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
Ingrown Toenail
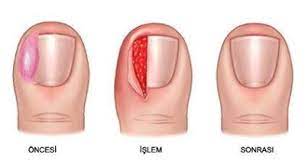
Ingrown toenail is a condition that develops when the inner or outer corner of the nail grows into the soft tissue. It is usually seen on the big toe. Although it is more common in adolescence, it is a common problem in all age groups.
What are the causes of ingrown toenails?
Ingrown toenails can have many causes:
- Incorrect cutting of the nail: This is usually caused by cutting the nail incorrectly, short, deep and rounded towards the root.
- Unsuitable footwear
- Crushes as a result of a blow to the finger
- Structural disorders of the nail and the surrounding soft tissue.
What are the symptoms of infection in an ingrown nail?
Swelling, hardness and tenderness in the soft tissue around the nail. When the soft tissue grows over the nail, bacteria enter the soft tissue and cause inflammation. When microbial inflammation occurs, redness, swelling, increased temperature and discharge are observed.
Treatment of ingrown nail
In mild cases and in the early period, treatment can be initiated with some applications to be done at home.
- Keeping toes and between toes dry and clean
- Placing a small piece of cotton wool under the ingrown corner of the nail once a day
- Use of antibiotic cream
- Wearing wide shoes or sandals
If the symptoms do not improve or worsen despite these applications, it is necessary to consult an orthopedic specialist without wasting time.
Surgical treatment of ingrown toenails
Most ingrown toenails heal without surgery. In case of an ingrown nail infection, oral and local antibiotics and dressings are applied. If the ingrown nail persists despite the applications and precautions taken, the ingrown part of the nail (a quarter of the entire nail) is cut and cleaned together with the nail bed called the nail root and the surrounding soft tissue covering. This procedure takes about 5-10 minutes under local anesthesia. The cleaned area is sutured to ensure early healing and a more aesthetic appearance is achieved.
How can ingrown toenails be prevented?
- It is recommended to wash the feet before cutting the nails to soften the nails or to cut the nails after a shower or bath
- When cutting nails, it is recommended to cut them straight, without rounding the corners, leaving them a little longer.
- Shoes that are suitable for your foot structure and do not squeeze the front side too much should be preferred
- It should not be too loose or too tight around the toes.
- It is necessary to protect the nail edges from bumps and scuffs
- If you have diabetes, your doctor’s recommendations for foot care should be followed exactly.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder and Elbow Surgery

Shoulder and elbow joint problems can occur due to strains or injuries in daily life and during sports activities, as well as due to falls, blows and accidental injuries. The difficulty in moving and using the arm that develops as a result of shoulder and elbow pain is a condition that negatively affects the daily lives of many people. In the surgical treatment of shoulder and elbow joints, procedures can be performed arthroscopically, i.e. closed joint surgery, or open surgery can be performed depending on the situation. Today, ligament, tendon, capsule repairs and some interventions to protect cartilage in shoulder and elbow surgery are performed arthroscopically. Open surgical methods are used in prosthesis surgeries for arthritis and in the treatment of some fractures.
- Conditions in which shoulder and elbow surgery is performed;
- Shoulder rotator cuff tears
- Recurrent shoulder dislocation
- Tennis and golfer’s elbow
- Ligament, tendon and nerve injuries
- Shoulder and elbow joint cartilage problems
- Calcification of the shoulder and elbow joints
- Shoulder, arm, elbow bone fractures
- Infection, tumor in the shoulder and elbow
- Infection, tumor in the shoulder and elbow
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Rotator Cuff Tear
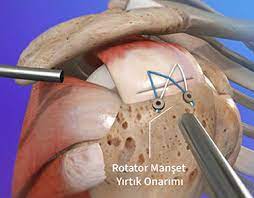
What is the rotator cuff in the shoulder?
The rotator cuff is the common name given to the 4 muscles that surround the shoulder head bone and have a similar function. These are the supraspinatus, infraspinatus, teres minor and subscapularis muscles. These muscles, which make up the rotator cuff, originate from the upper and posterior part of the shoulder blade and wrap the shoulder head bone like a cuff, and their tendons (tendons) attach to the bony protrusions on the outer and inner sides of the shoulder head. The main task of these muscles is to keep the rotator cuff balanced in the center of the joint during movements of the shoulder and to help achieve a healthy joint movement.
What is a shoulder rotator cuff tear?
Rotator cuff tears are usually caused by
It occurs in the tendons and at the attachment points of the tendons to the shoulder head bone. With advancing age, the tendons of these muscles weaken due to wear and tear. This leads to tears in elderly patients as a result of mild strain. In young people, rotator cuff tears usually occur after a trauma such as falling on the arm, having an accident, or being injured during sports.
What are the symptoms of shoulder rotator cuff tears?
The most common complaint in rotator cuff tears is shoulder pain. The pain is usually felt on the front and side of the shoulder and often radiates to the elbow. Increased shoulder pain, especially at night, is one of the typical findings of these tears. Other findings include limitation of movement in the shoulder and a feeling of loss of strength in arm movements. Patients with rotator cuff tears usually have difficulty with overhead activities. They also complain of not being able to move their hands behind their back towards their waist. Especially in patients with full-thickness and large tears in the rotator cuff of the shoulder, lifting the arm becomes extremely difficult and they feel weakness in the arm.
How is a rotator cuff tear diagnosed?
The orthopedic doctor evaluates the shoulder movements and the strength of the rotator cuff muscles. He/she determines the patient’s problems with using his/her shoulder in daily life. X-rays are first taken to detect the problem in the shoulder joint. In addition, tests such as shoulder joint ultrasonography (US) and magnetic resonance imaging (MRI) may be requested depending on the situation. In order to differentiate pain radiating from the neck to the shoulder, the neck area may also be evaluated and additional tests may be performed.
What are the treatment methods for rotator cuff tears?
Shoulder rotator cuff tears are generally divided into two as partial and full-thickness tears. In partial rotator tendon tears, treatment is started with cold application, rest and painkillers in the first stage. Then, physical therapy-exercise and regenerative injection applications to the shoulder, TZP (Platelet rich plasma), stem cell can be performed. However, surgery may be recommended in partial rotator cuff tears that do not benefit from all these treatments.
Although full-thickness rotator cuff tears usually do not respond well to surgical treatments, there is no harm in trying non-surgical treatments for a short period of time. In full-thickness rotator cuff tears, there is a risk of enlargement of the tear, retraction of the tendon and fatty degeneration of the muscle, so patients who undergo non-operative treatment should be followed more closely in this respect. In full-thickness rotator tendon tears that do not benefit from non-operative treatments, surgical treatment should be performed without delay to prevent additional problems.
How are shoulder rotator cuff tear repair surgeries performed?
Today, in parallel with the advancement of technology and medical techniques, most of the shoulder rotator cuff tears can be repaired with closed (arthroscopic) surgery. In closed shoulder surgeries, the patient, usually under general anesthesia, is operated on while sitting on a special operating room table. Small incisions about 1 cm in diameter are made in the shoulder joint area. Through these incisions, instruments and a special camera are inserted into the shoulder joint. After the disorders in the shoulder are detected with the help of the camera, the surgical procedure begins. Other problems accompanying shoulder rotator cuff tears can usually be treated in the same session.
After the tear area in the rotator cuff is detected, screws, usually 5mm in diameter, with threads behind them through special cannulas are inserted into the bone protrusion where the tear occurs. The threads behind these screws are passed through the torn tendon with special tools and techniques and the torn tendon is fixed back to the bone.
In the closed joint surgery technique performed with shoulder arthroscopy; since the surgery is performed through small incisions and without much damage to the surrounding muscles, the patient feels less pain after surgery compared to open methods and has a faster and more comfortable rehabilitation period.
What is the recovery period after rotator cuff tear repair surgery?
After arthroscopic, i.e. closed rotator cuff tear repair surgeries in the shoulder, patients leave the hospital on the same day or the next day depending on their general health status. In order to restrict movement in the shoulder and protect the healing of the repaired tendon, it is usually necessary to wear a padded shoulder strap for 6 weeks. Patients are advised to start doing elbow and wrist exercises immediately while wearing the shoulder sling to prevent swelling and limitation of movement in the arm. On the 10th postoperative day, the stitches are removed and the patient is allowed to bathe freely.
After the stitches are removed, you can start light passive exercises recommended by your orthopedic doctor and physiotherapist depending on the size, type and repair type of the tear. In some patients with poor bone quality and very large tears, such passive exercises may need to be postponed until the 6th week.
At the 6th week after shoulder closed rotator cuff tear repair surgery, patients are admitted to physical therapy and rehabilitation program. In this process, patients are encouraged to do assisted and active exercises to increase shoulder joint motion and strengthen their muscles.
Although it varies from patient to patient, physical therapy-rehabilitation programs continue for an average of 1 month. Patients who complete the physical therapy-rehabilitation program are given a home program and invited for follow-up visits.
After shoulder closed rotator cuff tear repair surgery, patients can start doing light work and driving in the 3rd month. After 6 months of rotator tendon tear repairs, people are allowed to do heavier work and return to sports.
What are the complications that may develop after surgery?
As with any surgery, some undesirable conditions may develop after arthroscopic closed rotator cuff tear repair surgery. Although relatively rare, the most common of these is restriction of movement. Postoperative limitation of motion may sometimes persist up to the 6th month. If significant restriction of motion still persists after 6 months after closed rotator cuff tear repair surgery, the stiff joint capsule can be loosened with closed surgical methods and range of motion can be restored.
Another complication that can be seen, albeit rarely, is recurrence of the tear, i.e. re-tear. The risk of re-tear is especially high in rotator cuff problems that are very large, operated late and have poor tissue quality. In case of a re-tear, the patient may need to be operated on again. If the tissue is suitable for surgical repair again, the tendon is sutured back into place. If the tendon tissue quality is very poor, a muscle membrane taken from the leg can be transplanted to the shoulder for repair.
Conclusion
Successful results are obtained with arthroscopic-closed repair surgeries in shoulder rotator cuff tears. When these tears are not treated appropriately, they can lead to wear and calcification in the shoulder, leading to conditions leading to shoulder prosthesis surgery. It is important that patients with complaints of shoulder pain, difficulty in movement and restriction of movement consult an orthopedic doctor as soon as possible without delay. As a result of the treatments to be applied, you can return to your daily life with a pain-free and comfortably moving shoulder.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Dislocation

What is shoulder dislocation?
The shoulder joint is a complex joint formed by the articulation of the shoulder blade, collarbone and the head of the arm bone. The bony head of the shoulder is surrounded by the joint capsule and various ligaments and muscles prevent the joint from dislocating. Normally, the articular surface of the head bone and the articular surface of the shoulder blade are in contact with each other in all angles of movement of the shoulder. The disruption of this joint harmony in the shoulder, as well as the disappearance of the relationship between the joint face of the head and shoulder blade, is called shoulder dislocation.
Why does shoulder dislocation occur?
Shoulder dislocations can occur for many different reasons. The most common of these is trauma. Shoulder dislocation usually occurs as a result of falling on the open arm. This type of injury is particularly common during fast-paced sports such as skiing, basketball and soccer.
Shoulder dislocation can also occur in similar falls or collisions in different sports.
Although most patients require a serious trauma to dislocate the shoulder, there are factors that facilitate shoulder dislocation in some patients. Especially in patients with diffuse ligament laxity, shoulder dislocation is more common. The risk of shoulder dislocation increases in patients with previous dislocation in the same shoulder and those who frequently practice overhead activities such as throwing sports.
What kind of damage can occur in the joint during shoulder dislocation?
When the shoulder joint dislocates, many structures in and around the joint can be damaged. Especially the anterior shoulder ligaments and the joint lip called labrum can be damaged. Apart from this, bone separation at the edge of the joint and collapse of the shoulder head bone may occur.
Again, tears may occur in the rotator cuff muscle tendons, which are more common in elderly patients. As you can see, joint dislocation is a serious injury and can cause significant damage to the tissues and bones around the joint.
What is the treatment for someone who dislocates their shoulder for the first time?
Treatment of a dislocated shoulder is urgent. The dislocation needs to be put back in place as soon as possible by a professional healthcare professional. In environments where medical facilities are available, i.e. health institutions, the dislocation should be performed under light anesthesia. The dislocation under anesthesia is more comfortable for the patient and the tissues are less damaged during the reattachment process as there is no need to force the dislocation. However, if medical facilities are not available and it takes a long time to reach medical facilities (in the mountains, at sea, etc.), the shoulder can be put back in place by people trained in this field.
After the shoulder is set in place, the patient is fitted with a shoulder strap called a “Velpau bandage”.
According to the recommendation of the orthopedic doctor, this sling is used by the patient for 1 to 3 weeks. If the patient’s pain persists after shoulder dislocation, if there is a feeling of dislocation after a certain period of time and if there is loss of movement, the patient may need an MRI. Because bone and soft tissues can be damaged during shoulder dislocation.
After some surgical interventions, the patient can quickly return to active life, while after some surgeries, the patient may need to use a shoulder sling for a few weeks and then undergo physical therapy to protect the procedure performed.
Surgery is rarely necessary after the first shoulder dislocation. However, if the patient is very young and an athlete, if serious damage has developed in the ligament and joint lip that holds the shoulder in place, and if there is severe bone collapse and bone loss, surgery may be required after the first dislocation as the risk of dislocation is high. Again, if large-scale rotator cuff tears occur after shoulder dislocation in elderly patients, surgery may be required after the first dislocation. If the above-mentioned conditions are not present, the first shoulder dislocation is usually treated with non-operative methods. After the shoulder is put back in place, strengthening exercises and, if necessary, physical therapy are started after using a shoulder strap for a few weeks and the patient is expected to regain his/her former function. After an average of 6 weeks, the patient can start full daily activities and after 3 months, the patient can start sports activities.
How is surgical treatment of shoulder dislocations performed?
Surgical treatment can be applied in patients who dislocate their shoulder for the first time, in patients with risk factors for re-dislocation and in patients with recurrent shoulder dislocation. In surgical treatment, damaged tissues are repaired or soft tissue or bone procedures are applied to prevent dislocation. The most common method used in shoulder dislocation surgery is repair of the joint lip injury (Bankart).
With the development of arthroscopic techniques, Bankart repair is now almost completely closed. In this method, the joint lip is repaired by placing 3 mm screws into the joint edge with the closed method and dislocation of the shoulder is prevented.
Again, if there is a collapse in the head bone, a muscle tendon can be transferred to the collapsed area (Remplisagge) to prevent the shoulder from dislocating again. More extensive open surgical methods can be applied in patients who dislocate again after surgery with the closed method, and in patients with severe bone loss with a tear on the joint surface. Latarjet surgery is the most common of these methods. In Latarjet surgery, a bone piece on the front of the shoulder is transferred to the front of the shoulder joint together with the tendons attached to it and fixed with screws. In patients with more soft tissue and bone damage, cadaveric bone transfer and complex soft tissue surgeries can be performed.
What is the recovery process after shoulder dislocation surgery?
The postoperative recovery process depends entirely on the surgical method applied and the size of the problem in the patient’s shoulder. However, in general, there is less pain after closed surgeries. After shoulder dislocation surgery, it is usually necessary to use a shoulder sling for a few weeks. Different exercises are started in the early and late postoperative period. Physical therapy may need to be started after a certain period. Generally speaking, the period after shoulder dislocation surgery can be summarized as 4-6 weeks of shoulder sling use, physical therapy period between 6 and 10 weeks, return to normal unrestricted daily life in the 3rd month, and return to sports activities in the 6th month.
Conclusion
Shoulder dislocation is a condition that should be treated urgently by professional healthcare teams. In some cases, surgical intervention may be required after the first dislocation and after recurrent dislocations. Successful results can be obtained with surgical treatments. After surgery, a sling should be used for a certain period of time and a physical therapy and rehabilitation program should be applied.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Shoulder Superior Capsule Reconstruction Surgery

What is superior capsule reconstruction surgery?
Superior capsule reconstruction (SCR) surgery, which has been developed in recent years, is a biologically based surgery that aims to protect the patient from shoulder prosthesis surgery, based on the principle of using patients’ own tissues, using advanced closed surgery techniques, developed for the treatment of irreparable rotator cuff tears of the shoulder joint.
The muscles called rotator cuff or rotator cuff are the common name given to 4 muscles that surround the shoulder blade and have similar functions. These muscles originate from the anterior upper and posterior parts of the scapula and wrap the shoulder blade like a cuff and attach to the bony protrusions on the side and inside of the shoulder blade. The main task of these muscles is to actively stabilize the shoulder blade in the middle of the joint during the movement of the shoulder joint, helping to achieve a healthy joint movement.
When large tears occur in these muscles, it causes impaired shoulder function and pain. The pain is usually felt in the front and side of the shoulder and often radiates to the elbow. Increased shoulder pain, especially at night, is one of the typical findings of these tears. Other findings include limitation of movement around the shoulder and loss of strength. These patients usually have difficulty with overhead activities. Patients often complain of not being able to move their hand behind their back. In patients with full-thickness and large tears, lifting the arm becomes extremely difficult and patients feel loss of strength.
If rotator cuff tears in the shoulder are not surgically repaired in the early period, the tear may enlarge and the muscle retracts and moves away from the bone. Since these muscles cannot function normally, fatty degeneration occurs within the muscle and the muscle loses its ability to contract completely. Muscles that develop fatty degeneration in this way and retract backwards at an advanced level cannot be repaired surgically, or even if they are repaired, the possibility of re-tear development is very high as a very tight repair will be obtained.
Shoulder superior capsule reconstruction is a surgical procedure using advanced closed surgical techniques developed in recent years, which allows the treatment of such late in the treatment of this type of rotator cuff tears in the shoulder region that are late in treatment, backward and accompanied by fat in the muscles, that is, irreparable rotator cuff tears in the shoulder region.
For which patients is shoulder superior capsule reconstruction surgery suitable?
Superior capsule reconstruction surgery is suitable for patients with large-scale, long-standing and neglected rotator cuff tears that are characterized as “irreparable”, meaning that the torn tendon ends have escaped backwards at an advanced level. However, SCR surgery will not be suitable for these patients if advanced wear has occurred in the shoulder joint due to the untreated tear.
In this case, the only option for patients with joint wear is reverse shoulder replacement surgery. To summarize, superior capsule reconstruction surgery is a suitable surgical treatment method for patients who have not yet developed wear in the shoulder joint, but have an irreparable rotator cuff tear.
How is shoulder superior capsule reconstruction surgery performed?
Superior capsule reconstruction surgery is performed under general anesthesia in a single session but in two stages. In the first stage, a skin incision of approximately 15 cm is made on the side of the patient’s thigh. The membrane of the muscle on the outer thigh of the leg is removed extensively. The tissue removed here is not the muscle itself, but the membrane on the outer side. Therefore, this tissue does not cause any impairment in muscle function after removal. The removed muscle membrane fills the same area as filling tissue within months.
In the 2nd stage of the surgery, the closed surgical procedure of the shoulder is started. Small incisions of about 1cm are made around the shoulder and the joint is entered with the help of a camera tip. After the condition of the joint and the tear is evaluated with the help of the camera, the upper part of the joint and the outer part of the head bone are prepared with the help of special tools. Special small diameter screws are placed in these areas. There are specially designed reinforced threads attached to the back of these screws. These threads are passed through the previously removed and prepared muscle membrane.
With a special method called the “Elevator Technique”, the muscle membrane is sent into the joint in a closed manner. After the strings are knotted under the camera view, the muscle membrane is placed and fixed between the joint bone and the head bone. This muscle membrane covers the head bone and acts as a kind of rotator cuff and prevents abnormal movements and rubbing of the bones against each other by keeping the head bone in the middle of the joint during joint movements. This reduces the patient’s pain and improves shoulder function.
What is the recovery period after superior capsular reconstruction surgery of the shoulder?
After superior capsule reconstruction surgery, patients are kept in the hospital for observation on the day of surgery and can be discharged the day after surgery if no complications develop.
Patients should use a padded shoulder strap for 6 weeks after surgery. During this period, the patient’s stitches are removed on the 15th day after surgery and the wound is allowed to be soaked, that is, to bathe freely.
In the 4th week, movements with the help of the other arm are allowed, and from the 6th week onwards, free movements are allowed. At the end of the sixth week, a physical therapy and rehabilitation program is started. The patient is allowed to start light sports activities at the end of the 3rd month and strenuous activities at the end of the 6th month.
What advantage does superior capsule reconstruction surgery provide to the patient?
Superior capsule reconstruction surgery is a salvage surgery for the shoulder joint, as can be understood from what has been explained above. In other words, this surgical procedure falls within the scope of joint-sparing surgery. The muscle membrane taken from the leg and transferred to the shoulder prevents friction between the bones in the shoulder and stops joint wear. Since joint wear does not progress, the patient does not need a shoulder prosthesis. In addition, since the head bone of the joint is more balanced in the middle of the joint during shoulder movements after surgery, shoulder movements are opened and strengthened. There is a significant decrease in the patient’s pain, especially at night.
What are the possible risks of superior capsule reconstruction surgery?
The general complications that can develop after superior capsule reconstruction surgery are similar to those seen in other general joint surgeries. However, the overall complication rate with this procedure is low. One of the complications specific to this method is the rupture of the muscle membrane transferred to the shoulder due to wear and tear. However, this risk has been minimized by applying advanced closed shoulder surgery techniques. The second common problem is fluid accumulation in the area where the muscle membrane is removed in the leg. This problem can also be treated in a short time with simple interventions.
Conclusion
Superior capsule reconstruction surgery is a joint-sparing surgical method based on the principle of closed muscle transplantation from the leg to the shoulder, designed for neglected-irreparable rotator cuff tears, with a low complication rate, high success rate, and advanced closed surgical techniques, the effectiveness of which has been proven in different studies.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Resurfacing Surgery

Hip pain, difficulty in movement and walking is a joint problem that negatively affects people’s lives. When congenital or acquired disorders and diseases of the hip joint are not treated properly, calcification develops in the joint. Hip joint calcification is a permanent condition and the functions of the person can only be improved with hip prosthesis surgery.
The aim of hip conserving surgery is to preserve the hip joint structure and to provide treatment with closed-arthroscopic or minimally open interventional surgical methods to eliminate some common hip problems detected early. Thus, in most patients, the development of joint calcification leading to hip replacement can be delayed or prevented. Hip preservation surgery is usually performed in young adults when there is no damage to the joint, but there is no age limit.
- Conditions in which hip conserving surgery is frequently performed;
- Developmental hip dislocation
- Hip impingement syndrome
- Labrum tears
- Cartilage damage
- Perthes disease
- Slipped femoral epiphysis
- Avascular necrosis of the hip head
- Post-traumatic hip problems
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Arthroscopy

Hip joint structure
The hip is the joint that joins the thigh bone (femur) to the pelvis (pelvis). The head of the thigh bone (femoral head) is round like a ball. The femoral head is placed in the socket (acetabulum) formed by the pelvis and forms the hip joint. The femoral head and the socket that form the hip joint are covered with a smooth-surfaced, slippery cartilage layer. This cartilage tissue allows the two bones to slide and move easily over each other.
A thick cartilaginous ring-shaped structure around the acetabulum, the hip joint socket, is called the labrum. While the labrum increases the depth of the socket in the hip, it also provides the stability of the hip joint by wrapping the femoral head like a gasket. Numerous ligaments and muscle tissues in the hip also support the stability of the joint.
What is hip arthroscopy?
Hip arthroscopy is a technique of closed surgery that allows the orthopedic doctor to evaluate the bone, ligament and cartilage structure of the joint and to intervene surgically. Hip arthroscopy is a joint-sparing surgery that allows early detection and intervention of problems in the joint and thus prevents rapid calcification of the hip. Hip arthroscopy is a different and more difficult technique than other joint arthroscopies. For this reason, it requires specialized equipment, and for successful surgical treatment, the specialist performing the surgery must have advanced training and experience in this field.
During arthroscopic surgery of the hip, a camera is inserted through a small hole into the hip joint and the image of the inside of the joint is transferred to the screen. With the help of special surgical instruments inserted into the joint through other small holes, the orthopedic doctor performs the procedure by watching it on the screen.
During arthroscopic surgery, the intra-articular structures are seen very closely and magnified. Thus, diseased tissues can be detected and treated much better. Arthroscopic surgery of the hip allows direct access into the joint without damaging or injuring the surrounding tissues and intervening only in the diseased tissues. In arthroscopic surgery, soft tissues such as muscles and capsules that provide joint movements, which are difficult to heal and painful, are not touched at all. This is especially important in the hip. Thus, postoperative joint movements are painless and comfortable. This allows for early and accelerated rehabilitation. It allows an earlier return to active life and sports. Since smaller incisions are made compared to open surgery, the risk of infection is also lower. Hip arthroscopy is a day surgery that does not require hospitalization.
In which cases is hip arthroscopy performed?
- In the diagnosis and treatment of problems that have been proven to originate from the hip joint but whose clinical and radiologic cause cannot be elucidated
- Removal of cartilage fragments that have fallen into the hip joint, tissues formed in the joint, bone-cement fragments in the joint space in hip prostheses
- In the early stage of hip osteoarthritis
- Hip impingement syndrome
- Acetabular labrum tears
- Partial cartilage damage
- Iliopsoas tendon disorders and bursitis
- Iliotibial band release
- Gluteus minimus tendon repair
- Resistant synovitis cases
- Hip joint infection
Who cannot undergo hip arthroscopy?
In order to perform hip arthroscopy successfully, the joint space must be clearly visible on the X-ray image of the hip. If a joint space cannot be detected, the arthritis has progressed too far. In this case, it is not possible to relieve the patient of pain by removing free lime and cartilage fragments. Hip arthroscopy is also not possible in very overweight and obese patients.
How is hip arthroscopy performed?
The hip is the deepest joint in the body. Its ball-and-socket shape also makes it difficult to enter the joint.
At the same time, the femoral head is located quite deep in the acetabular socket, so it is more difficult to reach it with an arthroscope than in the knee or shoulder joint. This problem has been solved by the development of new surgical instruments. Therefore, unlike other joint arthroscopies, arthroscopic operations of the hip cannot be performed without advanced operating room conditions, “traction table” and “scopy”.
First of all, the leg to be operated on is placed on the traction table and the hip joint is opened by 1 cm by applying controlled traction. A camera system is inserted through a 1cm incision made in the hip joint, accompanied by a device called scopi, which gives an instant X-ray image on the screen. Surgical instruments are inserted into the joint through one or two other holes and the operation is performed.
During hip arthroscopy, the intra-articular structures are first evaluated by direct visualization. Extremely small structures that cannot be detected by X-ray, tomography or even MRI-magnetic resonance imaging are clearly visualized by projecting them onto a television screen. The surgeon arthroscopically evaluates the structures inside the hip, identifies the problem causing the pain and then begins the surgical treatment.
Depending on the disorder detected during hip arthroscopy and its degree, there are various surgical methods that the orthopedic surgeon can apply in treatment. For example, if there is a frayed tear in the labrum surrounding the edge of the acetabulum, the seat of the hip joint, the damaged part is removed, leaving only the intact, uninjured labrum tissue. If the tear in the labrum has not caused abrasion of the labrum and has a smooth edge, repair can be performed without cutting out a piece of the labrum. In cases with hip impingement syndrome, abnormal bone structures are filed down and reshaped. If the cause of hip pain is cartilage deposits that have fallen into the joint, they are removed and the inside of the hip joint is cleaned. Minor damage to the hip joint cartilage can be cleaned and necessary procedures can be performed. In the presence of recurrent resistant synovitis or intra-articular infection of the synovial membrane, adhesions, thicknesses detected in the joint are cleaned, the joint is washed and a biopsy can be taken.
Recovery period after hip arthroscopy
Patients usually stay in hospital for only one or two days after hip arthroscopy surgery. Depending on the surgical procedure, patients may need to walk with crutches or a cane with a bracelet for a while. It is important that the exercises prescribed by the physiotherapist according to the patient’s condition are performed regularly at home.
Complications that may occur after hip arthroscopy include: complications related to anesthesia, infection, bleeding and swelling, thrombophlebitis, small instrument breakage in the joint, nerve damage, pain or numbness. These complication rates are lower when arthroscopic surgery methods are compared with open surgery methods.
Thanks to the smaller incisions made in minimal surgical methods such as hip arthroscopy, it is possible to detect and treat the problem causing pain in the joint early, with less blood loss and less tissue damage. After hip joint surgery, which is a joint-sparing surgery, patients experience less pain and can move more easily during the recovery period. Most patients return to their daily lives after a short period of time.
Conclusion
Developments in hip arthroscopy have provided great success in eliminating the problem with closed surgery in the early period before it reaches advanced calcification in this joint. Conditions such as hip impingement syndrome and labrum tears can be treated with hip arthroscopy. Hip arthroscopy is technically more difficult than other arthroscopies. When hip arthroscopy is performed by experienced orthopedic specialists trained in hip arthroscopy, clinical results and patient satisfaction are better.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Hip Impingement Disease
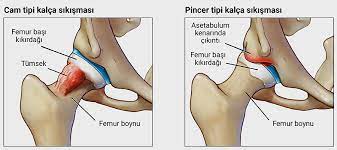
Hip joint structure
The hip joint is a joint that joins the thigh bone (femur) to the pelvis (pelvis). The head of the thigh bone (femoral head) is round like a ball. The femoral head sits in the socket (acetabulum) formed by the pelvis and forms the hip joint. The head and neck of the femur, which is the thigh bone, are inside the hip joint capsule. The femoral head and the socket of the hip joint, which touch each other, are covered with a layer of cartilage with a smooth surface. This cartilaginous tissue allows the two bones to slide smoothly over each other.
Around the joint socket in the hip is a thick cartilaginous ring called the labrum. The labrum supports the stability of the hip joint both by increasing the depth of the acetabular socket and by wrapping the femoral head like a gasket. The joint capsule and many strong ligaments surrounding the hip joint also support and protect the joint.
What is hip impingement disease?
Hip impingement occurs when the ball part of the femoral head, the femoral head of the hip, contacts the socket (acetabulum) prematurely or incompatibly during movement. This causes pain in the hip, usually in the groin area or on the outer side. Initially, the pain is more pronounced during long walks or sporting activities, but over time it can also be felt in everyday life. Especially when sitting or squatting for a long time, the pain increases, causing complaints such as stiffness and difficulty in movement. This inappropriate contact and compression, which recurs over time, causes damage to the articular cartilage and leads to calcification of the joint. When hip osteoarthritis occurs, patients need hip replacement surgery to get rid of this persistent pain, limitation of movement and difficulty in walking.
How does hip impingement occur?
It is a disease caused by compression of the cartilage and labrum tissue in between due to excessive contact between the femoral head-neck junction and the acetabular socket during hip joint movement. Hip impingement disease can be seen in three types;
- Glass type: It is caused by a hump-like protrusion in the bone where the femoral head and neck meet in the hip joint.
- Pincer type: It is seen when the acetabular socket of the hip joint is deeper and the coverage area over the femoral head is increased. In this type; a fringe-like protrusion is formed from the roof of the acetabulum on the outer lateral edge.
- Cases with Cam and Pincer types together.
In the Pincer type of hip impingement, the femur hits the protrusion on the roof of the acetabular socket during movement, resulting in damage to the cartilage. In the Cam type, the bump at the femoral head-neck junction rubs against the labrum, causing damage and tearing of the labrum. In both cases, labrum tear and cartilage damage as a result of repetitive friction and compression results in calcification of the hip joint in the future. These protrusions and hump-shaped deformities in the hip joint begin to form during adolescence, but the cause is not yet known.
What are the patient complaints in hip impingement disease?
The first complaint of patients is sudden pain in the groin area that occurs with certain movements or after exertion. Hip pain may occur after prolonged sitting or walking. The pain is usually felt in the groin and on the outer side of the hip, but it can also radiate from the front of the thigh to the knee. In some patients, the pain may be accompanied by a sticking or clicking sensation in the groin. After the initial painful period, there may also be a period of complete painlessness. At first, the pain increases after sports or heavy work, but if hip impingement is left untreated during this period, the damage to the joint increases.
The pain-free period decreases and patients begin to complain of constant groin, hip and leg pain. This results in calcification of the hip joint. In hip arthritis, joint movements are restricted, difficulty in walking and limping occur. The pain may occur not only during movements but also at rest and at night. Patients with this condition can only be helped by hip replacement surgery.
How is hip impingement diagnosed?
Knowledge and experience with hip impingement disease has increased considerably in the last ten years. In the past, the appearance of glass and pincers on hip X-rays did not attract attention. It can still be overlooked by specialists who do not deal with this subject.
Unfortunately, this situation results in calcification in the joint due to the fact that patients cannot be treated in the early period. In fact, since patients with hip impingement disease are treated with diagnoses such as herniated disc, inguinal hernia, knee meniscus problem, the time between diagnosis and treatment can be prolonged.
An orthopedic doctor experienced in hip problems usually suspects hip impingement disease after listening to the patient’s history and performing an examination. Glass and pincer-type deformities can be detected on hip X-rays. Magnetic resonance imaging (MRI) can be used to evaluate the cartilage and labrum and to make a differential diagnosis for diseases such as avascular necrosis of the femoral head. Hip joint ultrasound can be used to dynamically evaluate hip impingement. At the same time, tears and paralabral cysts, especially in the outer side of the labrum, can be detected by ultrasound and, if necessary, diagnostic injections can be performed. Sometimes, in the early stages of hip impingement disease, no significant findings may be detected on MRI. In this case, detailed examination and X-ray evaluation provide the most valuable data in the diagnosis of hip impingement disease.
Treatment of hip impingement disease
The first step in the treatment of hip impingement disease is to take some precautions to reduce hip impingement. These include not squatting on the floor, not sitting in a low seat, not turning the hip inwards or outwards or avoiding excessive bending towards the body, avoiding strenuous sports activities and losing weight. During the painful period, rest, various painkillers and some medications to reduce inflammation can be used. Afterwards, a physical therapy and exercise program is recommended. In mild cases, platelet-rich plasma injection known as TZP or PRP can be applied to the hip joint and labrum under ultrasound guidance. Closed surgical treatment with hip arthroscopy is performed in cases that do not respond to the measures and treatments taken, or in cases where significant tears or cartilage damage to the labrum are detected.
What is hip arthroscopy?
Although the hip arthroscopy method has surgical technical difficulties and requires special training of the orthopedic doctor, it has revolutionized the diagnosis and treatment of this disease. Hip arthroscopy surgery, which is performed closed with thin instruments inserted through small incisions, is not a method that damages healthy tissues, such as the large incisions used in the old open surgery methods and the removal of the femoral head from the socket by cutting a part of the bone. Therefore, hip arthroscopy is a much more comfortable surgery for the patient and has a shorter recovery period.
Today, the most common conditions for which hip arthroscopy is performed are hip impingement disease, labrum tear or a combination of both. In hip arthroscopy surgery, the impinged tissues are cleaned, bony protrusions are filed down and damaged tissues are repaired. Hip arthroscopy is a joint-sparing surgical method that reduces the risk of hip joint problems progressing to calcification and prosthesis surgery.
Recovery period after hip arthroscopy
Patients can usually go home the same day after surgery. Depending on the postoperative procedure and the orthopedic doctor’s recommendation, patients may need to use crutches for a while. Patients should also regularly do the recommended exercises at home. Patients with muscle weakness or difficulty in movement are admitted to a physical therapy and rehabilitation program. Most patients return to their daily lives after a short period of time. Return to active sports may take 2-4 months depending on the patient’s condition. The time between diagnosis and surgical treatment is an important determinant of the success of arthroscopic surgery in hip impingement disease.
Complications in hip arthroscopy
Although rare, some risks may be seen in hip arthroscopy. These include general complications related to anesthesia, infection in the joint, bleeding and swelling, thrombophlebitis, vascular and nerve damage, intra-articular small instrument tip breakage, pain or numbness. Compared to open hip surgery, hip arthroscopy has a lower risk of these complications.
Conclusion
Small structural differences in the hip joint that go unnoticed at a young age can lead to hip impingement disease, especially due to repetitive heavy work or repetitive strain from strenuous sporting activities. It is important to take preventive measures in the early period and to perform the necessary surgical procedure with hip arthroscopy. Otherwise, repetitive impingement and wear may cause damage to the hip cartilage tissue, resulting in joint calcification.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Height Lengthening Surgery

Lengthening surgery is a surgical operation performed by orthopedic specialists to lengthen the bones in the arms and legs and increase functionality. Apart from defects caused by leg length inequalities, poorly fused bone fractures as a result of unsuccessful treatment, congenital defects and developmental disorders, it can also be performed for aesthetic purposes.
Height growth occurs naturally over the years during growth and development. However, genetic factors, hormonal causes or chronic diseases can cause short stature. Although short stature or a disproportionate limb is not considered a disease, it can cause social, psychological and functional disadvantages that can have radical effects on the person’s life. Today, these problems can be prevented thanks to surgical methods.
- Who can undergo height lengthening surgery?
- Depending on the bone structure, it can be done from 4-5 years of age
- Treatment of dwarfism starts at an early age
- In general, the age range of 20-45 years is the most suitable period
For whom is height increase applied
“Lengthening surgeries can be performed from the age of 4-5 depending on the bone structure. Especially dwarfism treatment is started at an early age. Since the formation of new bone tissue and the healing process will become more difficult as the age progresses, the age range of 20-45 years is the most appropriate process. It is possible to increase the height by 10-15 cm with lengthening operation, but problems such as deterioration of the leg-body proportion that may occur with excessive increase in height should be taken into consideration. “
Techniques Used in Height Growth
Instead of externally applied external fixators, internal fixators that are placed inside the body and can be controlled from the outside are now more commonly used. There are also techniques that combine both methods.
Internal methods with specially developed nails do not require external stabilization and therefore offer more mobility and functionality during the lengthening process.
External Method
The external method uses orthopedic lengthening devices that are outside the body. External fixators such as TSF (Taylor Spatial Frame), Ilizarov device are available.
Internal Method
Orthopedic lengthening devices that are placed inside the bone and controlled from the outside are called internal devices; such as Precice®. Since there is no part outside the body in this method, it does not cause restriction of movement.
What is Precice 2 and how does it work?
Precise 2 is an orthopedic lengthening nail in the form of an interlocking metal rod. It is inserted into the bone canal through a small incision. After the surgery, the patient is given a special remote control. When this remote control is placed across the leg, the magnets in it cause the magnetic motor in Precise® to gradually lengthen. Thus, as the nail lengthens, so does the bone.
Precise® nails can be of different lengths and diameters, but the patient’s bone structure must be appropriate.
The bone diameter must be wide enough for the nail to fit into the bone canal.
In addition to the bone diameter, the bone length is also expected to be sufficient for the nail to be applied.
The shortest Precise® nail length is approximately 160-170 mm for the tibia and femur.
For this reason, a decision is made by making measurements with X-rays.
Precise® is accurate and controllable. It can be programmed to aid rapid healing.
3. Combined Method
It is a combination of internal and external technique. An intra-osseous nail is used in combination with an external fixative.
The disadvantage of this technique is the higher risk of infection due to the use of both implants.
It also requires three operations, first to insert the nail and apply the external stabilizer, second to remove the external stabilizer and lock the nail, and finally to remove the nail.
How is Height Lengthening Performed?
Every surgical intervention decision, including for aesthetic purposes, is an important step. Therefore, the patient should be informed about the surgical techniques to be applied, the general procedure, pre- and postoperative processes.
The surgery takes approximately 1.5-3 hours. Lengthening is achieved by the body’s capacity to form new bone tissue on its own. Along with the bone tissue, the surrounding soft tissues, ligaments, blood vessels and nerves adapt to this formation. Therefore, it is not necessary to harvest bone tissue from another part of the body or to lengthen the soft tissue with separate procedures.
In general, the process consists of surgically cutting the bone to be lengthened and gradually separating the two halves of the bone with different methods. Once the desired length is reached, the bone knits itself together until it can support the body weight again, forming bone tissue and lengthening is achieved.
First, the bone to be lengthened is cut, this procedure is called osteotomy. The leg is fixed with external or internal fixation, i.e. fixation methods. External fixation is usually done with ring-shaped apparatus fixed from the outside of the leg, while internal fixation method involves nail-like materials placed inside the bone.
The subsequent treatment process takes place in two phases;
Distraction Phase:
The bone area (osteotomy area), which is divided into two by the cutting process, is gradually and continuously separated from each other along the axis (distraction osteogenesis). With external control of the material used in the method, a total extension of 1 mm per day is achieved at intervals. In the space between the bone ends, new bone is formed from the body’s own bone tissue. At the beginning of this phase, patients usually start walking with the help of crutches.
Consolidation Phase:
The second phase is the healing and consolidation phase called consolidation. When the desired length is achieved, the bone tissue hardens in the cavity formed. Along with the bone tissue, the surrounding soft tissue also grows to the same degree. At this stage, the patient gradually begins to put more weight on the treated limb and walk without crutches.
Scientific Perspective
In the late stage of bone elongation, interleukins are released and act with growth factors released from platelets in the local hematoma to attract, proliferate and differentiate mesenchymal stem cells into osteoblasts and other differentiated mesenchymal cells. These in turn produce matrix, collagen fibers and growth factors.
Once a firm fixation is achieved, distraction triggers intramembranous bone formation. As the distraction phase progresses, the distraction cavity develops distinct zones with unmineralized bone in the middle, remodeling and mineralizing the bone peripherally. During consolidation, the high concentration of anabolic growth factors in regeneration decreases over time as mature cortical and cancellous bone forms.
Systemic diseases, congenital bone deficiencies, medications and substance abuse can often negatively affect the quality and quantity of regenerating bone.
Complications of Height Lengthening Surgery
As with any surgical operation, there are also possible complications of lengthening surgeries.
Infection can occur in the pin and wire areas of the apparatus used, in the incision areas or in the bone.
Early detection and precautions with patient follow-up and self-care can prevent this risk.
Edema formation may be observed in the area where surgery is performed. However, this is usually temporary. There may be scars at the application sites. Most scars usually disappear over time and do not cause any problems. During the operation, nerves and blood vessels are avoided as much as possible while the apparatus is inserted into the bone, but there is a risk of damage. Nevertheless, this is a very rare complication. A possible nerve injury may result in temporary or permanent loss of sensation or movement. A new surgical intervention will help recovery. Injured blood vessels can cause blood loss, depending on how severe the injury is. Damage to a large blood vessel is very rare and requires surgery to repair.
A blood clot in a vein in the leg is called a deep vein thrombosis (DVT). These clots can appear in the first few days after surgery. If the clot breaks off and travels to the lungs, it can cause serious problems with breathing. DVT occurs in less than 1% of patients. Movement after lengthening surgery can reduce the risk of DVT. Regional pain syndrome occurs when nerves become over-reactive after surgery. Common symptoms include pain, swelling, stiffness and sensitivity to touch. Treatment is usually with pain medication and physiotherapy.
Recovery after surgery
The lengthening process, which is performed by separating the cut ends of the bone with the control of the inserted apparatus, is started 1 week-10 days after the operation. This allows the maturation of blood vessels and soft tissue between both ends of the bone in the osteotomy site and the healing of the operation wounds. At this stage, the patient is allowed to walk using a walker.
New bone formation and progress are monitored with controls and X-rays.
In average 7-8 cm lengthening, approximately 4 months may be required for the newly formed bone to fully heal and consolidate. At this stage, the patient should be weaned from the walker and start walking using only a crutch or nothing at all. The patient can now return to an active practical life.
In this process, physiotherapy applications and follow-up are important for the bone and surrounding tissue to adapt to the new formation and to improve mobility.
It is possible to say that approximately 1 month recovery period is required for every 2 cm lengthening.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Contact
- Karanfil avenue . Alkaranfil street No: 4 Ofis No: 1 Beşiktaş / İstanbul
- +90 850 220 17 21
- info@checkupway.com

