WHAT IS CANCER?

Cancer is the abnormal growth of cells. Cancer cells multiply rapidly despite space restrictions, nutrients shared by other cells or signals from the body to stop reproducing.
Cancer cells are often shaped differently from healthy cells, do not function properly and can spread to many parts of the body. Tumours are abnormal tissue growth, clumps of cells that can grow and divide uncontrollably.
The first cancer to develop in a tissue or organ is called primary cancer. A malignant tumour is usually named after the organ or cell type affected. A malignant tumour that has not spread to other parts of the body is called localised cancer.
A tumour can invade the surrounding tissue more deeply and grow its own blood vessels. This process is also known as angiogenesis. If cancerous cells grow and form another tumour at a new site, this is called secondary cancer or metastasis. A metastasis retains the name of the original cancer. For example, bowel cancer that has spread to the liver is called metastatic bowel cancer, even though the person is experiencing symptoms caused by problems in the liver.
Cancer tumours can be divided into three groups: benign, malignant and precancerous (premalignant).
Benign tumours are not cancerous and are rarely life-threatening. Benign tumours tend to grow very slowly, do not spread to other parts of the body and are usually made up of cells that are quite similar to normal or healthy cells. Benign tumours can cause problems if they grow too large and put pressure on other organs (e.g. a brain tumour inside the skull).
Malignant tumours grow faster than benign tumours and have the ability to spread and destroy neighbouring tissue. Malignant tumour cells can break away from the main (primary) tumour and spread to other parts of the body in a process known as metastasis. After invading healthy tissue in the new site, it continues to divide and grow. These secondary sites are known as metastases and the condition is called metastatic cancer.
Precancerous (or premalignant) refers to a condition involving abnormal cells that may (or are likely to) develop into cancer.
WHAT IS ONCOLOGY?

Oncology is the study of cancer and tumours. The word ‘onko’ means mass or tumour and ‘logy’ means study in any field. Oncologists are physicians who specialise in the diagnosis and treatment of cancer. There are three main types of oncologists;
Medical oncologists who treat cancer with chemotherapy and other drugs,
Surgical oncologists who treat cancer by surgery,
Radiation oncologists who treat cancer with radiation,
Cancer treatment is a multidisciplinary team work.
As a matter of fact, medical oncologists mentioned above work as part of a multidisciplinary team that may include specialities such as a pathologist, molecular pathologist, psycho-oncologist, radiologist, interventional radiologist, primary care physician, geneticist, haematologist, palliative care specialist, oncology nurse.
An oncologist’s scope of practice is largely determined by the stage of malignancy (cancer). For example, treatment of early-stage cancer may involve a surgical procedure or radiotherapy, while treatment of advanced cancer may require chemotherapy.
WHAT ARE THE TYPES OF CANCER?
Cancer can be classified according to the cell type in which it starts. Some types of cancer that start in certain cell types are:
It is a type of cancer that originates from epithelial cells (the lining of cells that help protect or cover organs). Carcinomas can invade surrounding tissues and organs and metastasise to lymph nodes and other parts of the body. The most common types of cancer in this group are breast cancer, prostate cancer, lung cancer and colon cancer.
It is a type of malignant tumour of bone or soft tissue (fat, muscle, blood vessels, nerves and other connective tissues that support and surround organs). The most common forms of sarcoma are leiomyosarcoma, liposarcoma and osteosarcoma.
Lymphoma and Myeloma are cancers that start in the cells of the immune system. Lymphoma is a cancer of the lymphatic system, which circulates throughout the body and can therefore occur anywhere. Myeloma (or multiple myeloma) starts in plasma cells, a type of white blood cell that produces antibodies to help fight infection. This type of cancer can affect the cell's ability to produce antibodies effectively.
Leukaemia is cancer of the white blood cells and bone marrow, the tissue that makes up blood cells. There are several subtypes; the common ones are lymphocytic leukaemia and chronic lymphocytic leukaemia.
Brain and spinal cord cancers
Cancers of the brain and spinal cord are known as cancers of the central nervous system. Some are benign, while others can grow and spread.
Other Types of Tumours
Germ cell tumours are a type of tumour that starts in the cells that give rise to sperm or eggs. These tumours can occur almost anywhere in the body and can be benign or malignant.
Neuroendocrine tumours consist of cells that secrete hormones into the blood in response to a signal from the nervous system. These tumours, which can produce more hormones than normal, can cause many different symptoms. Neuroendocrine tumours can be benign or malignant.
Carcinoid tumours are a type of neuroendocrine tumour. They are slow-growing tumours that are usually found in the gastrointestinal tract (mostly in the rectum and small intestine). Carcinoid tumours can spread to the liver or other parts of the body, releasing substances such as serotonin or prostaglandins and causing carcinoid syndrome.
WHAT ARE THE RISK FACTORS FOR CANCER?

Cancers can be caused by many factors. In fact, most cancers develop as a result of exposure to many causal factors. Risk factors in cancer are as follows:
Age:
Many types of cancer become more common with age. The longer people live, the more they are exposed to carcinogens and the more genetic changes or mutations may occur in their cells.
Substances that cause cancer (carcinogens)
Carcinogens are substances that change the behaviour of a cell and increase the likelihood of developing cancer
Genetics:
Some people are born with an inherited high risk of cancer (‘genetic predisposition’). Although this does not mean that the development of cancer will definitely occur, it makes the disease more likely. For example, women who carry the BRCA 1 and BRCA 2 breast cancer genes have a higher predisposition to develop this type of cancer than women with a normal risk of breast cancer. However, less than 5% of all breast cancer is known to develop due to genes. So, although women with one of these genes are individually more likely to develop breast cancer, most cases are not caused by a high-risk inherited gene fault
Immune system:
People with weak immune systems are at risk of developing some types of cancer. People who have had organ transplants and who use drugs to suppress their immune system to stop organ rejection, as well as people whose immune system is weakened as a result of diseases such as HIV, may be at risk of cancer.
Alcohol consumption:
Excessive alcohol consumption can increase the risk for six types of cancer, including bowel (colorectal), breast, mouth, pharynx and larynx (mouth and throat), oesophagus, liver and stomach.
Being overweight or obese:
Obesity can increase the risk of developing 12 different types of cancer, including bladder cancer and pancreatic cancers.
Improper diet and nutrition:
Experts suggest that the consumption of red meats, processed meats, salty foods and diets that do not include fruits and vegetables are particularly effective on colorectal, nasopharyngeal and stomach cancer.
Lack of physical activity: Not only does regular physical activity help reduce excess body fat and associated cancer risks, but being physically active can also help reduce the risks of developing colon, breast and endometrial cancer
Smoking:
Cigarette smoke contains at least 80 different cancer-causing substances (carcinogens). When smoke is inhaled, the chemicals enter the lungs, pass into the bloodstream and are carried throughout the body. Smoking or chewing tobacco therefore not only causes lung and mouth cancer, but is also associated with many other cancers.
Ionising radiation:
Radon, x-rays, gamma rays and other forms of high-energy radiation can increase the risk of cancer. Prolonged and unprotected exposure to ultraviolet radiation from the sun, sunlight and tanning beds can also lead to melanoma and skin malignancies. People with fair skin, many moles on the body and a family history of melanoma or non-melanoma skin cancer are at risk from ionising radiation.
Hazards in some workplaces:
Some people are at risk of exposure to a cancer-causing substance through their work. For example, workers in the chemical paint industry have been found to have a higher than normal incidence of bladder cancer.
Infections:
Infectious agents are responsible for approximately 2.2 million cancer deaths per year. For example, about 70 per cent of cervical cancers are caused by human papillomavirus (HPV) infections, while liver cancer and non-Hodgkin’s lymphoma can be caused by hepatitis B and C virus, and lymphomas are also linked to Epstein-Barr. Bacterial infections have not been considered as cancer-causing agents in the past; however, recent studies have shown that people with helicobacter pylori infection in their stomachs develop inflammation of the stomach lining, which increases the risk of stomach cancer.
HOW DOES CANCER SPREAD?
Cancer is different from benign tumours because it can spread to different parts of the body from where it started. The cancer cells then start to grow in that area. A malignant tumour that spreads its cells to nearby tissues is known as invasive cancer. When cancer spreads from one part of the body to a different part, this is called secondary cancer or ‘metastasis’. For cancer to spread, it needs to increase its own blood supply. This is called angiogenesis. Without this blood supply, cells at the edge of the tumour will die from lack of oxygen.
Cancer cells produce substances that allow them to move around the body much more easily than normal cells.
Cancer cells also do not stick together as well as normal cells.
Cancer can spread in the following ways:
– Locally, in and near the tissue around the primary cancer
– Through the lymphatic system
– Through the blood circulation
WHAT ARE THE SYMPTOMS OF CANCER?
The symptoms of cancer vary greatly depending on the type of disease. For example, a malignant tumour can invade structures near the site of cancer growth, affect their function or press on nerves (for example, ovarian cancer can press on the colon, causing constipation; lung cancer can press on a nerve as it passes through the chest, causing hoarseness). Cancer can occur in many tissues and organs and can present with many different symptoms. Cancer often causes metabolic changes that result in general symptoms such as fatigue, weight loss and a general feeling of discomfort.
Being aware of the signs and symptoms of cancer is crucial for early diagnosis and effective treatment. However, it is also essential to pay attention to cancer screening tests in order to diagnose cancer at an early stage and to apply the right treatment. Even if the person does not have any complaints, he/she should protect himself/herself with cancer screening tests at certain ages. The most common symptoms of cancer can be listed as follows:
– Unexplained weight loss
– Lumps, bumps or enlarged lymph nodes
– Night sweats
– Bleeding (abnormal vaginal bleeding, blood in faeces or rectal bleeding, blood in urine)
– Changes in bowel movements (change in defecation or urination habits)
– Persistent and persistent cough
– Shortness of breath
– Pain in any part of the body,
– Persistent, severe fatigue
– Skin changes
– Feeling of bloating in the abdomen
– Difficulty swallowing
Some of these signs and symptoms may be specific to certain types of cancer, while others may occur in several types of cancer.
Unexplained weight loss
The first symptom of many cancers, especially stomach, pancreatic, oesophageal and lung cancers, is unexplained weight loss. This is equivalent to a 130 kg woman losing 6 or 7 kg or a 200 kg man losing about 10 kg. It is important for people who lose weight unexpectedly to be seen by a doctor. Although weight loss is more likely in advanced cancers, it can also occur in early-stage cancers.
Cachexia syndrome, which includes muscle loss as well as weight loss, is not only a symptom of cancer, but is considered a direct cause of death in about 20 per cent of people with cancer.
Swellings, lumps and bumps on the body
Bumps and lumps in various parts of the body can be a symptom of many types of cancer. Breast lumps can be among the symptoms of cancer, less common symptoms of breast cancer include redness, thickening or orange peel appearance in the breast. Testicular lumps can be a sign of testicular cancer. Just as women are advised to perform monthly breast self-examinations, men should perform monthly testicular examinations.
Enlarged lymph nodes can be the first sign of cancer, especially lymphomas, and can occur in many parts of the body. On the other hand, it should not be forgotten that the lumps that are noticed may be a sign of the first stage of cancer, as well as an indicator of the last stage.
Night sweats
Night sweats are a common symptom of cancer, especially leukaemias and lymphomas. Night sweats caused by cancer are not just ‘hot flushes’. In the case of cancer-induced night sweats, people may be soaking wet that they have to get out of bed and change their pyjamas. Night sweats are more common during sleep.
Haemorrhages
Unusual bleeding can occur early or late in many cancers. Blood in the sputum may indicate lung cancer, blood in the faeces may indicate colon cancer, blood in the urine may indicate bladder cancer and untimely vaginal bleeding may indicate cancer of the uterus or cervix. The colour of the blood can sometimes be important in determining where the blood comes from. Bleeding from the lower colon (left colon) and rectum is usually bright red. Those from the upper colon (right colon) and small intestine are usually dark red, brown or black. Blood from higher up, such as from the oesophagus or stomach, often resembles coffee grounds. Other causes of rectal bleeding include haemorrhoids, anal fissures and colitis. On the other hand, some types of colitis are a risk factor for colon cancer.
Persistent and persistent cough
A persistent and persistent cough can be one of the first signs of lung cancer. A persistent cough may also be a sign of cancer that has spread to the lungs, such as breast cancer, colon cancer, kidney cancer or prostate cancer.
Shortness of breath
Shortness of breath is one of the leading early symptoms of lung cancer. Although lung cancer can be associated with a chronic cough, the most common symptoms of lung cancer have changed over time. Previously, the most common types of the disease tended to grow near the large airways in the lungs, which could lead to a frequent (bloody) cough. Today, the most common form of lung cancer, adenocarcinoma of the lung, tends to grow in the outer regions of the lungs. These tumours can grow quite large before they are detected and often cause shortness of breath.
Chest, Abdominal, Pelvic, Back or Headache
Pain in any part of the body can be a possible sign of cancer.
Headache
Headaches are the most common symptom of brain cancer or tumours that have spread (metastasised) to the brain; however, the majority of headaches are not due to cancer.
The classic headache associated with a brain tumour is particularly severe in the morning and progresses over time. These headaches may worsen with activities such as coughing or pressing for a bowel movement and may only occur on one side of the head. People with headaches due to a brain tumour often have other symptoms such as nausea and vomiting, weakness on one side of the body or new onset seizures. However, brain tumours can cause headaches that are indistinguishable from tension-type headaches, which may be the only sign that a tumour is present.
Cancer that has spread to the brain (brain metastases) is seven times more common than primary brain tumours and causes similar symptoms.
Cancers most likely to spread to the brain include breast cancer, lung cancer, bladder cancer and melanoma. It is not uncommon for people with brain metastases, especially those with small cell lung cancer, to have symptoms related to a tumour in the brain before symptoms related to the primary cancer appear.
Back pain
The most common cause of back pain is tension in the back, but persistent back pain with no obvious cause can also be a sign of cancer. Cancer-related back pain is often (but not always) worse at night, the pain does not go away when you lie down, and it can be worse with a deep breath. Back pain can be caused by tumours in the chest, abdomen or pelvis or metastases from other cancers to the spine.
Shoulder pain
Pain in the shoulders or shoulder blade can often be due to a muscle strain, but in rare cases it can also be an important early sign of cancer. Pain from lung cancer, breast cancer and lymphomas, as well as metastases from other cancers, can cause pain in the shoulders or pain in the shoulder blade.
Chest pain
Unexplained heart disease or chest pain can also be a sign of cancer. Although the lung has no nerve endings, many people diagnosed with lung cancer have pain that feels like ‘lung pain’.
Pain in the abdomen or pelvic pain
As with pain in other parts of the body, although abdominal pain and pelvic pain are mostly associated with conditions other than cancer, these two types of pain in particular (uterine cancer, ovarian cancer, ovarian cancer, cervical cancer, tubal cancer, ovarian cancer) should not be neglected as they are among the symptoms of cancer and should be checked by a doctor.
Feeling of fatigue
Unlike ordinary fatigue, fatigue caused by cancer is often much more persistent. Some people describe this fatigue as “full body fatigue” or exhaustion. The hallmark of this type of fatigue is that it significantly reduces quality of life.
There are many ways in which cancer can cause fatigue. In general, the growth of a tumour can be challenging for the body. Other symptoms of cancer, such as shortness of breath, anaemia, pain or a reduced level of oxygen in the blood (hypoxia), can also cause fatigue.
Skin changes
Skin changes can be seen in internal organ tumours as well as skin tumours. Some types of cancer can cause jaundice, darkening of the skin or redness of the skin. Although skin cancers such as basal cell carcinoma and squamous cell carcinoma are more common, melanoma is responsible for most deaths from skin cancer. It is worth noting that melanomas are usually first noticed by someone else. A suspicious skin spot on the body should not be neglected, and a health institution should be consulted.
Bloating (Abdominal Distension)
Abdominal bloating can be the first sign of many cancers, including ovarian cancer, pancreatic cancer and colon cancer. Ovarian cancer symptoms are often referred to as the “silent killer” because they often appear late in the disease. Bloating has been found to be a common symptom of ovarian cancer; however, women often attribute this symptom to weight gain or other causes. Similarly, constipation, pain during intercourse and frequent urination can also be symptoms of ovarian cancer. If any of these symptoms are noticed, a doctor should be consulted. It should not be forgotten that early diagnosis of ovarian cancer increases the success of treatment.
Blood in the urine
Blood in the urine may be a symptom of bladder cancer.
Difficulty swallowing
Difficulty swallowing, also known as dysphagia, can be a symptom of cancer. Difficulty swallowing is usually the first symptom of oesophageal cancer due to narrowing of the oesophagus. On the other hand, since the oesophagus passes through the region between the lungs, tumours such as lung cancer and lymphomas in this region can often cause this symptom.
WHAT ARE THE RARE SYMPTOMS OF CANCER?
Some of the rare symptoms of cancer are as follows:
Blood clots
There are many risk factors for blood clots in the legs, known as deep vein thrombosis (DVT). In recent years, it has been noted that one of these factors may be a previously undiagnosed cancer. 20 It is important to know the symptoms of DVTs not only because of this, but also because they often break off and travel to the lungs, a condition known as pulmonary embolism.
Urine changes
Changes in urination can be an early sign of cancer.
Heartburn or indigestion
Chronic heartburn due to gastroesophageal reflux disease (GERD) may be one of the causes of oesophageal cancer.
Shingles
Shingles, a condition caused by reactivation of the chickenpox virus, can be a symptom of cancer in rare cases.
Depression
New-onset depression can also be an early symptom of cancer.
Minimally traumatised fractures
When cancer spreads to bones it can weaken them, so that fractures occur with minimal trauma. A fracture that occurs in a bone weakened by cancer is called a pathological fracture.
Easy bruising
Bruises that are not caused by injury can also be assessed by the doctor. Cancer cells infiltrating the bone marrow can reduce the number of platelets in the blood. A decrease in platelets can also cause easy bruising. Some leukaemias, lymph node tumours or bone marrow cancers can cause bruising. In addition to easy bruising of the skin, gum bleeding, nosebleeds or bleeding from anywhere else may occur in these diseases. If you experience nosebleeds for no apparent reason, a lot of bleeding from the gums after brushing, very intense and prolonged bleeding from small cuts or abrasions, you should consult a doctor immediately.
White spots in the mouth
White spots on the gums or tongue (leukoplakia) can be an early sign of oral cancers.
Other causes
Some cancers cause unique symptoms depending on the compounds they produce and secrete. For example, some lung cancers produce a hormone-like substance that raises the level of calcium in the blood.
HOW IS CANCER DIAGNOSED?
The tools used to diagnose cancer are extensive and include laboratory tests, imaging studies and other invasive or non-invasive procedures
Physical examinations
It is used to evaluate lumps, masses, lesions or changes in skin colour that may indicate cancer.
Complete blood counts (CBC)
During treatment, abnormalities in blood chemistry suggestive of leukaemia may be detected while monitoring the development of anaemia, infection or other complications.
Tumour marker tests
Tumour marker tests are blood tests used to measure substances in the blood that tend to rise if cancer is present. These include the prostate-specific antigen test (PSA) to detect prostate cancer, the BRCA1 and BRCA2 tests used for both breast and ovarian cancer, and the CA-125 test used to detect a tumour associated with a range of cancers
Flow cytometry
Flow cytometry evaluates cells suspended in liquid and is useful in diagnosing leukaemia or lymphoma from a blood or bone marrow sample.
Biopsy
A biopsy is the removal of a sample of tissue or fluid from the body for evaluation under a microscope. It can be obtained by fine needle aspiration (FNA), core needle biopsy, cone biopsy or surgery.
Imaging tests
Imaging tests are used to diagnose cancer. These tests can include X-ray, computed tomography (CT) and magnetic resonance imaging (MRI). Nuclear medicine imaging using radioactive tracers can diagnose certain types of cancer, while changes in metabolism can be detected consistent with positron emission tomography.
Genomic testing
Genomic testing can help identify the chromosomal characteristics of a tumour and help the oncologist understand what triggers the disease and choose the most appropriate drug treatments.
WHAT IS CANCER STAGING?

The classification of cancer according to the anatomical extent of the disease, i.e. stage, is essential for patient care, research and cancer control. The UICC TNM staging system is the common language adopted by oncology healthcare professionals to communicate about the extent of cancer for each individual patient. Once the stage of cancer is known and understood, this often provides a basis for deciding appropriate treatment and individual prognosis. It can also be used to inform and evaluate treatment guidelines and forms vital information for policy makers developing or implementing cancer control, prevention plans and research.
TNM classification focuses on the anatomical size of the tumour and is determined by evaluating the following categories:
T defines the size of the main (primary) tumour
N describes whether the cancer has spread to nearby lymph nodes
M describes whether the cancer has metastasised (spread from the primary tumour to another part of the body)
WHAT IS METASTASIS?
Metastasis is the spread of cancer to a different part of the body from where it started. In other words, cancer cells can settle and multiply in a different part of the body and form new tumours. Cancer cells metastasise to other areas through the lymphatic system and blood circulation. Cancer cells from the original or primary tumour can travel to other areas such as the lungs, bones, liver, brain and other areas. These metastatic tumours are ‘secondary cancers’ because they originate from the primary tumour. Metastasis is important as it helps determine staging and treatment.
WHAT IS CANCER TREATMENT?

Doctors treat cancer according to the type of cancer, its stage at diagnosis and the person’s general health.
Approaches to cancer treatment are as follows:
Chemotherapy uses drugs that target rapidly dividing cells.
The aim of these drugs is to destroy cancerous cells. The drugs can also help to shrink tumours. Some side effects of chemotherapy can be severe.
Hormone therapy involves taking medicines that change the way certain hormones work or interfere with the body’s ability to produce them.
Hormonal therapy is used to treat breast cancer, prostate cancer and cancers of the reproductive system by changing the amount of hormones in the body.
Immunotherapy, one of the new generation treatment approaches in cancer disease, aims to enable the body to defeat cancer on its own by activating the immune system.
Immunotherapy, which has far fewer side effects than chemotherapy and targeted smart therapies, creates a memory in immune cells, resulting in better, long-term and permanent responses.
Radiotherapy uses high doses of radiation to destroy cancerous cells. The doctor may also recommend radiotherapy before a surgical procedure to shrink the tumour or reduce tumour-related symptoms.
Stem cell transplantation may be especially useful for people with blood-related cancers such as leukaemia or lymphoma.
In cancer treatment, surgery is part of the treatment plan. For example, the surgeon may remove lymph nodes to reduce or prevent the spread of the disease.
Targeted therapies work to prevent cancerous cells from multiplying. They can also strengthen the immune system. Two examples of these treatments are small molecule drugs and monoclonal antibodies.
These treatment methods are used alone or in combination.
The first treatment is usually known as first-line treatment.
The treatment given after the first-line treatment is called adjuvant treatment. As a matter of fact, chemotherapy applied after the surgical procedure is adjuvant treatment. The treatment given before the first-line treatment is called neoadjuvant treatment.
FREQUENTLY ASKED QUESTIONS ABOUT CANCER
What is palliative treatment in cancer?
The aim of palliative care is to make the person feel as well as possible and to improve their quality of life, regardless of the stage of cancer. Palliative care can address the physical, mental, psychological and social needs of the cancer patient. Palliative treatment can continue at the same time as curative treatment. This means that patients receiving palliative care may still have active treatment to reduce or stop the growth of cancer. The palliative care team will work with cancer specialists to manage side effects from treatment and help maintain the patient’s quality of life. Cancer treatments such as surgery, chemotherapy, immunotherapy, targeted therapy and radiotherapy may also be used as part of palliative care. In this case, the aim is to relieve symptoms, not to control the cancer.
What are the goals of cancer treatment?
Cancer treatments have different goals;
Definitive cure (Cure):
The aim of treatment is to cure the cancer completely, allowing you to live a normal life. Depending on your particular situation, this may or may not be possible.
Primary treatment:
The aim of primary treatment is to completely remove the cancer from the body or kill the cancer cells. Any cancer treatment can be used as primary treatment, but the most common primary cancer treatment for most common cancers is surgery. If the person’s cancer is particularly sensitive to radiotherapy or chemotherapy, one of these treatments may be taken as your primary treatment.
Adjuvant treatment:
The goal of adjuvant therapy is to kill cancer cells that may remain after primary treatment to reduce the chance of the cancer recurring. Any cancer treatment can be used as adjuvant therapy. Common adjuvant treatments include chemotherapy, radiation therapy and hormone therapy.
Palliative treatment:
Palliative treatments can help relieve the side effects of treatment or the signs and symptoms caused by cancer. Surgery, radiotherapy, chemotherapy and hormone therapy can be used to relieve signs and symptoms. Medicines can relieve symptoms such as pain and shortness of breath.
What should be done to prevent cancer?

Cancer is one of the most common causes of death in our country and in the world. Exposure to chemical substances, smoking and alcohol consumption, stress and unhealthy diet cause an increase in cancer cases. Can the risk of cancer be reduced by avoiding these external factors? Experts say that lifestyle changes reduce the risk of cancer. Especially by changing eating habits, avoiding habits such as smoking and alcohol, and an active life, the rate of cancer can be reduced. The two most important issues in cancer prevention are choosing healthy foods and avoiding carcinogens such as smoking. Recent studies show that a diet rich in vegetables and fruits, a life without smoking, regular physical activity and maintaining a healthy body weight can reduce the development of cancer by up to 40 per cent. This means preventing 3-4 million new cancer cases in the world every year. Foods contain vitamins, minerals and fibres that are essential for a good and healthy life, as well as bioactive molecules known as antioxidants, which have protective effects. These protect the body against many serious diseases, including cancer.
Statistics show that the most common cancers diagnosed are lung, breast and large intestine cancers, and the most common causes of loss of life are lung, liver and stomach cancers. Cancer screening tests should be given importance in order to diagnose cancer at an early stage and to apply a correct treatment. Even if the person does not have any complaints, he/she should protect himself/herself with cancer screening tests at certain ages.
It is recommended that the following recommendations be taken into consideration to prevent cancer:
- People should try to maintain their ideal weight.
- One-way nutrition should be avoided. All food groups including meat, milk, cereals, fruits, vegetables and fats should be consumed in appropriate amounts during the day.
- Attention should be paid to eat 5 portions of fruit and 2 portions of vegetables a day.
- Pulp intake is very important in cancer prevention. For this reason, rye, wholemeal or whole wheat bread should be preferred instead of white bread. Fruits that can be eaten with their peels should be consumed without peeling.
- Excess sugar consumption should be avoided in order to maintain ideal weight.
- Baking or boiling should be preferred as cooking method. Frying should be avoided and the food should be cooked without over-roasting.
- It is important not to smoke and not to be in smoking environments.
- Inactivity should be avoided and care should be taken to increase daily physical activities. Doing sports at least 2 days a week is an important condition for a healthy life.
- 2-2.5 litres of water should be consumed daily.
- Tea and coffee consumption should be reduced. Half-fat milk can be used instead of milk powder when drinking coffee. Instead of drinks with high sugar content such as acidic drinks and ready-made fruit juices, low-sugar compotes, pleasantries, freshly squeezed fruit juices can be drunk.
- Excessive alcohol intake should be avoided.
- It is important to consume fish 2 or 3 times a week to benefit from the positive effects of Omega-3 fatty acids.
- The frequency of consumption of foods with high antioxidant content such as broccoli, cauliflower and cabbage should be increased.
- Care should be taken to prepare all kinds of food well washed and clean and clean water should be used.
- Frying oils should not be used repeatedly.
- Foods cooked directly on fire should be consumed at most one day a week.
- Daily salt consumption should be below 5 grams.
- Consumption of foods with high salt content such as pickles and pickles should be limited.
- Salami, sausage and smoked food groups should be avoided as much as possible.
- It is important to consume 2 glasses of milk or yoghurt during the day.
- Direct sunlight should be avoided, especially in summer.
What should cancer patients pay attention to?
Cancer patients should generally pay attention to the following points.
- Natural and healthy foods, fresh vegetables and fruits should be consumed daily in main and intermediate meals in accordance with the season.
- Improper nutrition during chemotherapy leads to excess weight as well as stomach complaints. Sugary and floury foods are the most important reason for this. Brown sugar should be preferred and rye bread made of whole wheat flour should be consumed instead of white bread. Solid or internal fat and margarine should not be used.
- A small amount of sunflower or olive oil should be preferred.
- It is important to drink plenty of water.
- If the patients are taking medication for blood pressure, cholesterol, diabetes or other chronic diseases before chemotherapy, they should never stop taking them.
- The medication of patients using blood thinners will also be regulated by the oncology specialist.
- Orthopaedic mattresses and pillows should be preferred and 8 hours of sleep should be allowed.
- Dishes should be washed in the machine, not by hand.
- Cancer patients should avoid these!
- Excess milk (more than 1-2 glasses per day) is not recommended as it will cause sudden blood sugar drop and rise. Instead, 250 gr – 500 gr yoghurt or buttermilk can be cottage cheese.
- The amount of red meat should be reduced. Protein should be taken from other protein sources such as white meat, cheese, legumes.
- Excessive fatty and heavy meals should be avoided.
- Foods high in sugar should not be preferred.
- Grapefruit from citrus fruits should not be used in patients receiving chemotherapy because it may interact with drugs, and oranges and tangerines should be preferred.
- High doses of vitamins should not be used and a doctor should be consulted before taking vitamins.
- Mixtures with unknown ingredients should never be consumed.
- Patients with breast tumours should consult their doctor before using soya and flaxseed.
- Cancer patients should prefer sports that do not tire the body excessively and that they can enjoy.
- It should consume plenty of water against skin dryness.
Patients who are uncomfortable with the taste of water can drink herbal teas.
- Telephone should not be a chat tool for cancer patients. Short calls should be made and headphones should be used.
- When using a laptop computer, care should be taken to ensure that the computer is on the table.
- The television should be switched off from the button as well as the remote control. In this way, radiation emission is prevented.
- Cancer patients can have MRI and tomography. There is no harm for patients to pass through the X-ray machine.
Can cancer cause weight gain?
Although weight loss is a more common sign of cancer, some people with cancer may gain weight. Studies show that more than half of women with breast cancer gain weight during treatment and that these extra pounds are linked to worse outcomes. Excess weight can be a side effect of medicines such as steroids or hormones. Also, some chemo drugs can cause extra fluid retention, known as oedema. This can also lead to weight gain. In addition, many patients with cancer find that their energy levels drop, which can lead to inactivity and weight gain.
Does cancer affect blood pressure?
Some cancer drugs, such as anti-VEGF drugs, can cause an increase in blood pressure. These treatments help to block blood flow to tumours, but can also affect other blood vessels in the body, which can increase blood pressure. High blood pressure can also be a sign of certain cancers, such as adrenal cancer. Chemotherapy and certain targeted drugs used to treat cancer can also cause low blood pressure.
What is the link between smoking and cancer?
Some of the deaths caused by cancer are due to smoking and other tobacco products. Smoking 1-10 cigarettes a day increases the risk of lung cancer by 20 per cent compared to non-smokers, while smoking two packs increases the risk by 80 per cent. On the other hand, even if one does not smoke, being in a smoking environment (passive smoking) increases the risk of lung cancer by approximately 1.5 times. The risk of developing lung cancer in someone who has smoked a packet of cigarettes a day for about 20 years is halved within 10 years after quitting smoking. Quitting smoking is the most important prevention to reduce the risk of cancer and other cardiovascular and lung diseases. For this purpose, when you contact your doctor, you will need during smoking cessation psychological and medication (nicotine patches, gum) support. Smoking plays a very important role in the development of cancers of the lung, throat, oesophagus, bladder, pancreas, kidney, cervix and breast. In addition to nicotine in tobacco, many carcinogenic substances such as nickel, cadmium, tar, monoxide, arsenic and radon cause cancer by mutating the p53 tumour suppressor gene. Passive smokers are also at risk. The most important cause of paediatric cancers is parental smoking. In fact, smoking during pregnancy is the most important cause of paediatric leukaemia.
What is the link between cancer and obesity?
Decreased physical activity and obesity lead to an increase in cancer types. Scientific studies show that obesity is a risk factor in breast, uterine, bowel, oesophagus and kidney cancers. This increased risk is thought to be linked to an increase in estrogen due to obesity. Therefore, preventing obesity and increasing physical activity is considered to be an important factor in the prevention of cancer.
Can cancer cause blood clots?
People with cancer have a higher risk of developing deep vein thrombosis (DVT: a blood clot that forms in a deep vein). Many chemotherapy drugs can also increase the risk of DVT.
Does environmental pollution increase the incidence of cancer?
An important cause of cancer is increasing environmental pollution. Mankind digs up the earth and unearths many minerals, but does not show the same sensitivity in neutralising the wastes of these minerals, which should not be present in the earth. “Batteries” that are used every day and thrown away are the simplest examples of this. The contribution of environmental pollution to cancer formation reaches about 10 per cent when ozone depletion and occupational factors are included. The decrease in stratospheric ozone has increased the harmful effects of ultraviolet rays and the effect of ultraviolet on skin cancer is certain.
What is the importance of psychological support in cancer?
The feelings of shock, denial, anger, sadness, fear and guilt that sometimes accompany the feelings of shock, denial, anger, sadness and fear experienced by a patient who learns that she has “cancer” when she goes to the doctor because of a small lump in the breast, bleeding in the urine, a cough that does not go away or a mole that has changed its shape can cause both the patient and her relatives to experience psychological problems. These emotions can create a crisis situation by affecting the whole life of the person, including work and social life. In the fight against cancer, treating and supporting the soul as well as the body is of great importance for the treatment to be successful. Psychological support also improves the patient’s quality of life. The supportive therapies to be determined by the specialised doctors dealing with cancer psychology for each patient will help patients and their relatives to overcome this difficult process more easily. The improvement in the psychological state of patients and the positive perspective they gain also increase their quality of life and the chances of success in their treatment. It is possible to adapt to the disease process that emerges suddenly from a healthy life, to feel physically and mentally well, and to increase the power of struggle with these support therapies. In addition, it is very important to provide psychiatric support to increase the ability to cope with physical and mental complaints such as anxiety, restlessness, depression, insomnia, weakness, nausea and pain, to include family members who have experienced a similar crisis in the support system of the patient in a healthy way, to provide psychiatric support to restore the order of social life, sharing responsibilities, work and economic life that has been interrupted.
Does salt consumption cause cancer?
Although salt itself does not cause cancer, it disrupts the structure of the stomach surface and prepares the environment for the effect of carcinogenic substances. Again, substances called nitrosamine in pickles where salt is used in abundance are important in the formation of cancer.
Why can cancer cause back pain?
Most cases of back pain are not caused by cancer, but back pain can be an indicator. Back pain can be a sign of primary bone cancer, metastases from the breast, colon, testicles or lungs. is a symptom of many types of cancer, including cancer of the spine. Often the tumours press on the spine, affecting the surrounding nerves and causing pain in the back.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
Gynaecological cancer types, which are called female cancers, are listed as follows:

What is gynaecological oncology?

Gynaecological oncology is the branch of science that examines cancers originating from the female reproductive organs.
What is gynecologic oncology concerned with?
Ovaries, uterus, tubes, vagina, vulva that limits the entrance to the vagina are among the female reproductive organs. Gynaecological oncology plays a role in the prevention, diagnosis and treatment of cancers in these organs. Gynaecological oncology is a department that houses the best doctors. Gynaecological oncology surgery is also a branch of gynaecological oncology. Gynaecological oncology is also known as gynaecological oncology, gynaecological oncology, gynaecological cancer surgery, gynaecological oncology by many people.
What are the symptoms of female cancers?
Female cancers give different symptoms depending on the type and stage of the disease. Symptoms of female cancer can be listed as follows in general terms:
- Bleeding or discharge in women onset of menopause
- Menstrual irregularity
- Adet dışında kanamalar
- Pain after sexual intercourse, abdominal pain
- Abdominal swelling
- Wounds in the vaginal area, itching
- Eating and drinking problems
Factors predisposing to cancer
Many chemical products such as industrialisation, increased environmental and air pollution, nutrition with ready-to-eat foods and smoking prepare the ground for the development of cancer cells by disrupting the structure of inhibitory genes that prevent cancer and tumour formation in the human organism. It is unlikely that these negative factors can be prevented or reduced. Therefore, the reality of cancer must be accepted and measures must be taken.
Advances in health informatics are making cancer treatment easier
Despite the rapid increase in the number of cancer cases, early diagnosis of cancer is possible thanks to important steps taken in the field of health technology. In addition, the increase in medical knowledge and surgical experience makes treatment more effective. In the last 10 years, clinical and molecular studies on reproductive system cancers have clarified many unknowns and the factors that cause cancer have been better understood. The use of treatments such as direct cancer cell-directed therapy, vaccines and immunotherapy also contribute to survival rates.
The medical oncology department deals with chemotherapy applications, which means the treatment of cancer with drugs. In medical oncology centres in our country, chemotherapies, targeted smart drugs and molecules, hormonotherapy, immunotherapies and biological therapies recommended by the oncology doctor are applied in cancer treatment.
Paediatric and female cancers
The increase in the incidence of cancer, the increase in the age of marriage and the postponement of conception to advanced ages due to women’s work life bring cancer and the desire for children together in an average of 10 per cent of women. In women who do not have children, if cancer is caught at an early stage, reproductive ability can be preserved by removing only the cancerous area with hormonal or surgical treatment depending on the type of disease. After having a child, surgical treatment can be completed if treatment is required.
Cervical cancer and reproductive preservation surgery have been performed for more than 20 years in the world and the results are satisfactory in terms of pregnancy after treatment. In early stage uterine cancer, only the cancerous area is removed and the uterus and vagina are combined.
Twenty per cent of uterine cancers occur under the age of 45 and 5 per cent under the age of 40. Therefore, the number of patients with uterine cancer and desire for children is quite high. In this case, if the disease is in the early stage, that is, if it has not spread outside the inner wall of the uterus and the cell type is not very bad, it can be treated with medication and after the disease is regressed, conception can be achieved. In this case, up to 70 per cent success can be achieved with progesterone treatment.
In recent years, fertility preservation in ovarian cancers has become increasingly common. Especially in germ cell ovarian cancers and borderline type ovarian cancers seen at an early age, it is possible to become pregnant by removing only the cancerous tissue or the cancerous ovary and preserving the uterus and the opposite ovary.
Success rates in treatment increase with advanced surgical techniques
Rapidly developing surgical techniques and the widespread use of laparoscopic surgeries in the world and in Turkey provide early recovery and reduce the risks of open surgery. All these contribute significantly to the early diagnosis and effective treatment of cancer.
Laparoscopic and robotic surgery are increasingly effective treatment methods for uterine cancer, cervical cancer and ovarian cancer caught at an early stage. Thanks to these methods, the patient’s hospital stay, recovery, return to work and social life are shortened and the patient does not have cosmetically significant skin damage.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS ENDOMETRIOSIS?
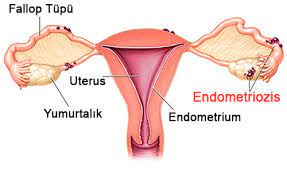
Endometriosis is defined as the presence of the endometrium layer, which normally forms the inner part of the uterus, outside the uterus. This disease is usually seen in the lower parts of the abdomen, which we call the pelvis. However, it can be seen less frequently all over the body. Endometriosis, which is estimated to be seen in approximately 5-10 per cent of women of reproductive age, is among the most important causes of infertility.
WHAT ARE THE SYMPTOMS OF ENDOMETRIOSIS?
Endometriosis symptoms can be listed as follows:
- The most important findings are pain during menstruation
- Constant severe pain in the lower abdomen
- Severe pain during sexual intercourse
- Difficulty and pain when going to the defecation, sometimes diarrhoea
- Frequent urination and blood in the urine
- Side pain, back pain
WHAT CAUSES ENDOMETRIOSIS?
The exact cause of endometriosis is not clearly known. Although there are several theories, none of these theories alone can explain all cases of endometriosis. It is more common especially in thin, tall, red-haired, coloured-eyed women. Some of the theories trying to explain endometriosis are as follows:
- When menstruation starts in women, the superficial part of the endometrium, the inner layer of the uterus, is expelled, while the same layer can be poured into the abdominal cavity through the tubes. In women with a healthy immune system, these blood and endometrial tissues spilled into the abdominal cavity are cleared, while in some women they cannot be cleared and settle in the tubes, ovaries, intestines, bladder or other organs in the abdominal cavity. It causes migration of defence cells called inflammation in these areas. In the later stages of the disease, bleeding, tissue healing and adhesions in the abdomen may occur. Endometriosis foci formed in the ovaries bleed into the ovaries with the effect of hormones during each menstrual period, causing lesions known as endometrioma. The blood accumulated in the ovary turns brown in time and these cysts are popularly called chocolate cysts because they resemble chocolate.
- . Another theory is that the cells in the lining of the uterus reach other organs of the body through the blood vessels. Although rare, foci of endometriosis that cause bleeding in the patient’s eye every menstrual period or cause blood to accumulate in the chest cavity every menstrual period have been reported in the literature. These foci can be explained by this theory.
Some conditions that prevent endometriosis are also known. These include pregnancy, multiple births and breastfeeding. Again, endometriosis is less common in overweight women with high body mass index and especially high waist-to-hip ratio.
HOW IS ENDOMETRIOSIS DIAGNOSED?
The definitive diagnosis of endometriosis is made when the endometrial tissue, which should normally be found only in the inner layer of the uterus, is seen in other parts of the body, these tissues are surgically removed and microscopically observed by pathology specialists.
Detailed history and symptoms of the patient are very important for preliminary diagnosis. Findings obtained from the patient’s history, such as menstrual pains that start later, pain in the lower abdomen, pain during sexual intercourse, inability to have children spontaneously, pain during large toilet, bloody urine or bloody faeces are important for the detection of the disease.
On examination, endometriotic nodules located in the vagina, if any, can be seen. Chocolate cysts can be palpated. The diagnosis of chocolate cysts can be made more clearly in gynaecological ultrasound performed together with the examination. Endometriotic nodules on the rectum, the last part of the large intestine, can be seen. A preliminary diagnosis can be made in 70 percent of severe endometriosis cases by gynaecological examination.
Sometimes additional investigations may be required. In patients with bloody urine, endometriotic lesions in the bladder or urinary tract can be seen with the help of a thin camera with a procedure called cystoureteroscopy. In patients with bloody stools, endometriotic nodules can also be seen with colonoscopy. In addition, magnetic resonance imaging (MR) is a valuable method in the diagnosis and surgical planning of deep infiltrative endometriosis.
However, it is worth mentioning again that the definitive diagnosis of endometriosis is made by microscopic examination of the lesions removed by laparoscopy.
HOW IS ENDOMETRIOSIS TREATED?
Endometriosis is a treatable problem. Treatment should be individualised according to the patient’s complaints, whether she wants to have children or not and the examination findings. A wide range of treatments can be applied, from waiting-observation therapy, drug therapy, assisted reproductive techniques to surgery.
While women with endometriosis whose pain is at the forefront may benefit from medical treatment, in advanced cases, surgical treatment may be considered in women who want to have children when assisted reproductive techniques fail.
If the person applies with the complaint of inability to conceive for a certain period of time, assisted reproductive techniques such as vaccination and in vitro fertilisation are used in the first stage. Some of the patients who undergo assisted reproductive methods such as in vitro fertilisation can become pregnant. If there is no response from these treatments, surgical removal of the disease can be performed. In the surgical method; removal of chocolate cysts with laparoscopic surgery, opening of adhesions, restoring the tubes to their normal anatomy or removal of nodules in cases of deep infiltrative endometriosis with severe pain despite treatment. Chocolate cysts should be monitored more carefully, especially in patients over the age of 40. Because there is a risk of ovarian cancer development on the basis of chocolate cysts. If a suspicious appearance is detected on ultrasound or MRI, removal of the ovary and tube may be considered. However, I would like to emphasise once again that there is no standard approach in these patients and treatment should be individualised for each patient.
FREQUENTLY ASKED QUESTIONS ABOUT ENDOMETRIOSIS
What are the risk factors for endometriosis?
Some of the risk factors determined for endometriosis disease in addition to cases such as starting menstruation at an early age, having menstruation more frequently than 21 days, never having given birth, having a large amount of menstrual bleeding, being tall, red hair, blue-green eye colour, being freckled are as follows:
- Infertility
- Congenital structural defects of the female reproductive organs
- Alcohol, caffeine
- Diet with fat and meat
- Low body mass index
- Endometriosis in a first-degree relative
- Endometriosis, which does not cause any complaints, is less common in blacks but more common in Asians compared to the white race.
Does endometriosis prevent conception?
Endometriosis is seen in 5-10 per cent of all women of reproductive age in our country. However, this rate can reach up to 25-30 per cent in women who have problems with conception. Endometriosis can prevent conception for different reasons. Endometriosis can prevent the egg from reaching into the tubes by forming adhesions in the reproductive organs. Sometimes it can prevent pregnancy by blocking the end of the tubes, that is, by causing ‘tubal obstruction’. Endometriosis may also cause chocolate cysts called endometrioma. These cysts can settle in the ovaries and prevent a healthy ovulation, as well as reduce the chance of pregnancy by reducing the egg reserve. Cytokines and humoral factors secreted from endometriosis foci may adversely affect embryo development and attachment. After treatment, pregnancy increases by 40 per cent after two years of waiting. However, if the person is still unable to conceive normally, in vitro fertilisation can be tried.
What is deep endometriosis?
“Deep infiltrative endometriosis”, which is a special type of endometriosis disease that is common in women of reproductive age, sometimes manifests itself with severe pain and sometimes it can progress silently without any symptoms. Patients who do not show symptoms usually consult a doctor with the complaint of inability to conceive.
“Deep infiltrative endometriosis”, which is defined as the spread of endometriosis deep into the uterine ligaments between the vagina and rectum, intestines, bladder, urinary bladder, urinary ducts and peritoneum, is a disease that requires a multidisciplinary approach that concerns not only the field of gynaecology but also general surgery, urology, gastroenterology.
These tissues, which may not show any symptoms until advanced stages, can block the ducts in the intestinal region when they reach very large sizes. In this case called “deep infiltrative endometriosis”, it is important that the surgery is performed by experienced hands and experienced people. Because during the operation, the area between the uterus and the intestine and the ureters, which are the urinary tubes, must be freed very well. In surgery, it is very important to remove the part of the intestine that is often involved and to bring the remaining parts together. In order to diagnose deep endometriosis, which seriously affects the social life of the patients, and to prevent endometriosis from causing serious adhesions between the tissues, it is important that the diagnosis and treatment are performed by experienced hands and in centres with the necessary equipment.
Is endometriosis a disease with herbal treatment?
Endometriosis cannot be solved with herbal treatment. Products sold on the internet under the name of “herbs for endometriosis” may cause more harm than good. Treatment for endometriosis should be planned with a specialist gynaecologist and obstetrician.
When is endometriosis diagnosed most often?
Endometriosis is diagnosed between the ages of 25-35 on average. There is a delay period of approximately 7 years between the onset of the disease and the diagnosis.
Is endometriosis seen after menopause?
Endometriosis is a hormone-dependent disease. Since the estrogen and progesterone hormones produced from the ovaries cease in menopause, endometriosis is expected to regress. The incidence of endometriosis in the postmenopausal period is less than 5 per cent, and these women usually have a history of hormone replacement therapy used to relieve menopausal symptoms.
Is endometriosis related to being overweight?
In addition to the risk factors that cause endometriosis, there are also factors that provide protection from this disease. Pregnancy, multiple births and breastfeeding are among the main protective factors, while endometriosis is less common in obese women with high body mass index and especially high waist-to-hip ratio.
Is menstrual pain a sign of endometriosis?
Yes, severe menstrual pain may be a sign of endometriosis. However, menstrual pains do not start from the first menstruation, but at any later period. Menstrual pain from the first menstruation is called primary dysmenorrhoea and the causes are usually different. Unfortunately, many women may take menstrual pains as natural and feel that they have to live with these pains. Most women may think that these pains are normal instead of going to a doctor. However, this problem decreases the quality of life of women and may adversely affect reproduction in the later stages.
What is a chocolate cyst?
A chocolate cyst is a type of cyst that grows in the ovaries, tubes and uterus of women and bleeds into itself during each menstrual period. Chocolate cysts are so named because the menstrual blood that accumulates in them becomes a little more fluid, like chocolate, and turns brown in colour after a while. The real name of these cysts is endometrioma. The diagnosis is mostly made by ultrasound. The ca125 level in the blood is usually checked, but it cannot help us much in the differentiation with ovarian tumour.
Chocolate cyst treatment varies according to the individual. In young, childless women, the growth of chocolate cysts can be suppressed with birth control pills. If women who want to have children cannot conceive spontaneously, assisted reproductive techniques such as vaccination and in vitro fertilisation may be necessary. In women who cannot conceive despite these treatments, surgery may be required in women with large cysts and therefore increased risk of torsion or rupture. The gold standard treatment in these patients is complete removal of the cyst wall by laparoscopic surgery. If it cannot be completely removed, the possibility of recurrence increases. Since the risk of cancer development on the basis of endometrioma increases, especially over the age of 40, more detailed evaluation and imaging methods such as MRI may be required when necessary. In the presence of a suspicious lesion, it may be necessary to remove that ovary and tube.
Is there a connection between endometriosis and infertility?
One of the reasons for women who cannot get pregnant may be endometriosis. In some of these women, scar tissue caused by endometriosis causes obstruction in the woman’s tubes. However, the reasons why endometriosis affects fertility in most women are not yet clearly known.
Endometriosis can briefly cause the following:
- It reduces the number of eggs in the ovaries, which we call ovarian reserve.
- It impairs ovulation function.
- It can cause obstruction in the tubes and prevent the union of sperm and egg.
- It produces natural toxins that kill sperm.
- It prevents the embryo from attaching to the uterus.
- It has a harmful effect on embryo development.
Can women with endometriosis get pregnant with in vitro fertilisation?
In women with endometriosis, IVF treatment can provide pregnancy rates of up to 60 per cent in a single attempt in proportion to their age. Of course, it is necessary to repeat IVF treatment in women who cannot conceive in the first attempt. With repeated attempts, the chance of pregnancy can be achieved to a great extent.
Is the immune system effective on endometriosis?
The exact cause of endometriosis is still unknown. The most widely accepted theory is that the tissues in the uterus pass through the tubes of the woman during menstrual bleeding and settle in the abdominal cavity and continue their development here. It is thought that the immune system also differs from normal to allow this.
Is endometriosis found in the rectum?
Endometriosis is a very common health problem. This tissue can be found in organs inside the abdomen (ovary, uterine canal, peritoneum, intestines, rectum, urinary bladder) or outside the abdomen (vagina, umbilicus, eye, pleura). Depending on the severity of the symptoms and the rate at which the endometriotic nodules reach the internal canal of the rectum, it may be necessary to remove the rectum, which is the last part of the large intestine where the nodule is located in some patients, and to reconnect the remaining parts, and in some patients, it may be necessary to scrape the nodule from the rectum with scissors.
What is important in chocolate cyst and endometriosis surgery?
Gynaecologists and Obstetricians pay attention to the following points in these operations:
- Not to damage the ovarian reserve: In these operations, the ovarian tissue outside the cyst wall should not be damaged. Because if the ovarian tissue is damaged, the eggs located here may be damaged and the patient may face early menopause and infertility problems in the future. Not damaging the ovaries, tubes and uterine tissue are the most important points in chocolate cyst surgery.
- Opening of adhesions: Chocolate cyst may cause dense adhesions compared to other ovarian cysts. Opening and correction of these adhesions during surgery can reduce the pain complaint and increase the success rate for pregnancy treatment.
- Removal of deep-seated endometriosis nodules: Endometriosis and chocolate cysts may also be associated with severe groin and abdominal pain. Preoperative detection of endometriosis nodules, especially deep infiltrative endometriosis, which cause severe pain, is of great importance. In the presence of these nodules, removal of the chocolate cyst alone does not completely relieve the pain. Deep infiltrative endometriosis nodules must be removed together with the ovarian cyst. This region is very important in terms of surgery. Because it is in close proximity to the rectum, which is the part of the large intestine behind the uterus and ovaries, and the tubular structures called ureters, which provide the passage of urine from both kidneys to the bladder. Protection of these tissues during surgery is of great importance. For this reason, these surgeries are performed by experienced physicians.
How many cm of chocolate cyst requires surgery?
There is no specific size limit for chocolate cyst surgery. The patient’s age, infertility, rupture and torsion risks should be discussed with the patient and a decision should be made together. Rupture is the rupture of the endometrioma parts of the ovary and spillage of the endometrioma content into the abdominal cavity. Torsion, on the other hand, is the rotation of the ovary and tube including the endometrioma around itself, disruption of blood flow and gangrene. In this case, the ovary and the tube are returned to their original state. Unfortunately, in some patients the ovary cannot be saved.
Will the chocolate cyst go away on its own?
Chocolate cysts do not go away on their own. The treatment is surgical. Although some medications prevent the growth of cysts, they cannot eliminate them. If the cyst bursts, its contents may spill into the abdominal cavity, but the risk of recurrence is quite high because the wall of the cyst is not removed.
How does a chocolate cyst cause pain?
People with chocolate cysts say that they have menstrual pain. They also state that their pain starts just before menstruation and continues throughout the menstrual period. Patients may express that they have pain especially in their groin, legs and lower back. Chocolate cyst can also cause pain during sexual intercourse. Sometimes pain can also be felt in the intestines and bladder.
How to recognise a rupture of a chocolate cyst?
Patients with ruptured endometriomas report a stabbing pain in the groin, which then spreads throughout the abdomen. A ruptured chocolate cyst can be detected by ultrasound. Sometimes nausea, vomiting and weakness may be observed along with the pain.
What is the CA 125 value in chocolate cyst?
The Ca125 value is actually a blood test that we use in patients with a mass in their ovaries to distinguish whether the mass is malignant or cancerous. Ca125 levels can be elevated in many conditions other than cancer. One of these conditions is chocolate cysts. Especially in ruptured, i.e. burst chocolate cysts, Ca125 values can reach quite high values and can mimic advanced ovarian cancers with the content of the chocolate cyst poured into the abdomen.
Does chocolate cyst cause discharge?
Chocolate cysts do not cause discharge because they are seen in the ovaries located in the abdomen and are not directly connected to the vagina.
Can chocolate cysts occur in single women?
Chocolate cysts can occur in single women.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS UTERINE CANCER?
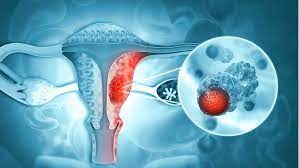
Uterine cancer is one of the most common types of cancer in women. The uterus is made up of cells called endometrium, which thicken regularly and shed menstrually when the time comes. These cells sometimes undergo changes and can divide and multiply abnormally. This is called uterine cancer or endometrial cancer.
WHAT CAUSES UTERINE (ENDOMETRIAL) CANCER? WHAT ARE THE RISK FACTORS?
What causes uterine cancer? The exact answer to the question is not known. However, changes in estrogen and progesterone levels in the body can cause uterine cancer. The endometrium can be affected by changes in estrogen and progesterone levels. This interaction may predispose to uterine cancer. Although the causes of uterine cancer are not known exactly, risk factors are known.
The risk factors that cause uterine cancer are as follows:
- Age: The risk of uterine cancer increases with age. However, uterine cancer can also be seen at a young age.
- Starting menstruation at an early age can cause uterine cancer. Exposure to estrogen hormone for years increases the risk of uterine cancer.
- Late menopause. Uterine cancer usually occurs after menopause. Late menopause can increase the risk of uterine cancer by causing more exposure to the hormone estrogen.
- Obesity is one of the factors that increase the risk of uterine cancer. Since excessive fat tissue produces estrogen, the risk of uterine cancer is higher in obese women.
- Diabetes can increase the risk of uterine cancer. The risk of uterine cancer in women with type 2 diabetes is almost 2 times higher than those without diabetes.
- Not having a pregnancy. During pregnancy, the hormone balance shifts towards progesterone. Never getting pregnant can cause uterine cancer.
- Polycystic ovary syndrome. In polycystic ovary syndrome, estrogen levels are high and progesterone levels are low. This increases the risk of uterine cancer.
- Some hormone suppressing drugs used in the treatment of breast cancer can also cause uterine cancer.
- Those with a family history of bowel cancer are in the more risky group in terms of uterine cancer.
- Radiation therapy for other cancers may predispose to uterine cancer.
- Hormone replacement therapy after menopause can cause uterine cancer.
WHO CAN GET UTERINE CANCER?
Uterine cancer is generally menopausal cancers. It is more common over 55 years of age. However, it can also be seen at a young age.
WHAT ARE THE SYMPTOMS OF UTERINE CANCER (ENDOMETRIAL CANCER)?
The first symptoms of uterine cancer are vaginal bleeding. Especially during menopause, vaginal bleeding should be considered as uterine cancer until proven otherwise. In menstruating women, irregular intermittent bleeding and excessive bleeding may be the first symptoms of uterine cancer.
Apart from vaginal bleeding and discharge, different symptoms may also be experienced when uterine cancer progresses.
- Pelvic pain
- Abdominal pain
- Bloating
- Frequent urination
- Pain during urination
- Bleeding in the postmenopausal period
These complaints may also occur due to different problems. However, it is important for those who experience one or more of the symptoms of uterine cancer to consult a gynaecology and obstetrics doctor for early diagnosis.
WHAT ARE THE STAGES OF UTERINE CANCER?
It is important to know the stage of cancer in order to plan the treatment of uterine cancer correctly. The stage of uterine cancer is determined by the extent of the tumour area, the spread of uterine cancer to the lymph nodes and whether the uterine cancer has metastasised. Uterine cancer is generally handled in 4 stages.
- Stage 1 of uterine cancer: Cancer is only in the uterus. There is no spread to surrounding tissues or distant parts of the body. Stage 1 can be handled under 2 separate headings according to how far the cancer cells have spread to the uterine muscle tissues (myometrium).
- Uterine Cancer Stage 2: Cancer is seen in the uterus and cervix. In other words, cancer has spread from the body of the uterus and progressed to the supporting connective tissues of the cervix. There is no metastasis in the lymph nodes and distant parts of the body
- Stage 3 uterine cancer: The cancer has spread outside the uterus. However, the spread has not reached the rectum or bladder. Stage 3 according to the spread to the fallopian tubes, ovaries, lymph near the uterus. Uterine cancer can be divided into sub-headings.
- Stage 4 uterine cancer: It is the last stage of uterine cancer. Cancer has spread to the rectum, bladder or more distant organs in the body. It is analysed under 2 sub-headings. Uterine cancer stage 4A: The cancer has spread to the mucosa of the rectum or bladder. Uterine cancer stage 4B: The cancer has spread to the lymph in the groin area, bones or distant organs such as the lungs.
When determining the stages of uterine cancer, the appearance of the cancer cells under a microscope is also important. If the cancerous cells look like healthy tissue and have different cell groups, this is called a “differentiated” or “low-grade tumour”. If the cancerous tissue looks very different from healthy tissue, it is called “poorly differentiated” or “high-grade tumour”. The grade of the tumour can give an idea of how fast the uterine cancer will spread.
HOW IS UTERINE (ENDOMETRIUM) CANCER DIAGNOSED?
“How to understand uterine cancer?” is one of the most curious topics. Women who experience one or more of the symptoms of uterine cancer should go to the gynaecology and obstetrics doctor without wasting time. After the pelvic examination, some tests may be required to clarify the diagnosis.
- Vaginal ultrasound: Ultrasound imaging method is used to see the tumours in the uterus and its structure. The thickness of the uterine wall or other abnormalities can be determined with the ultrasound probe placed at the entrance of the uterus.
- Hysteroscopy: An imaging method called hysteroscopy can be used to diagnose uterine cancer. A thin flexible tube with a fibre optic camera is inserted into the uterus. This allows the inside of the uterus and the endometrium to be examined.
- Pathological evaluation. In order to make a definitive diagnosis of uterine cancer, a tissue sample taken from the uterus by curettage must be pathologically evaluated. The biopsy can be performed under hysteroscopy and anaesthesia.
- Computed Tomography (CT) and Magnetic Resonance (MR) : CT or MR imaging methods can be used to determine the size of the abnormality or tumour in the uterus. Contrast material can be used in CT or MRI imaging to get a clearer image. If the treatment plan will include hormone management, MRI may be useful to obtain detailed images. MRI images can also be used to see how far the cancer has grown into the uterine wall and to determine whether fertility can be preserved.
HOW IS UTERINE (ENDOMETRIUM) CANCER TREATED?
In the treatment of uterine cancer; many factors such as the type of cancer, stage, possible side effects of the treatment to be applied, the general health status of the patient, age, the effects of the treatment to be applied on fertility are taken into consideration.
Although surgical methods come to the forefront in the treatment of uterine cancer, chemotherapy, radiotherapy, hormone therapy, targeted therapy and immunotherapy can be applied. In the treatment of uterine cancer, sometimes only one or more than one of these methods can be applied in combination.
- Uterine cancer surgery
The most common method in the treatment of uterine cancer is surgery. Along with hysterectomy surgery, pathological examination of the uterus during surgery called frozen is the main treatment method. Depending on the result of frozen, it may also be necessary to remove the lymph around the vessel.
- Chemotherapy treatment of uterine cancer
In the treatment of uterine cancer, chemotherapy can be applied before or after surgery. Chemotherapy can be administered after surgery against the risk of recurrence of uterine cancer, and preoperative chemotherapy can be administered before surgery to shrink the tumour and remove it completely. It can also be used alone or in combination with radiotherapy.
- Radiotherapy treatment of uterine cancer
Radiation therapy is usually given after surgery to destroy any remaining cancer cells. In some cases, radiotherapy can also be used before surgery to remove the entire tumour. Radiotherapy may be preferred in patients whose general health condition is not suitable for surgery.
- Hormone therapy for uterine cancer
Hormone and hormone blocking drugs can be used to change hormone levels. Hormone therapy can slow the growth of uterine cancer cells. Hormone therapy can be used in case of recurrence of uterine cancer and in metastatic uterine cancers. Hormone therapy is usually combined with chemotherapy.
WHAT SHOULD BE CONSIDERED TO PREVENT UTERINE CANCER?
As in breast cancer and cervical cancer, there is no screening method. The most effective prevention method in uterine (endometrium) cancer is early diagnosis. Therefore
Every woman should have a regular gynaecological examination.
Birth control pills can be taken. Using oral contraceptives for one year can reduce the risk of uterine cancer. However, it should not be forgotten that these oral contraceptives have side effects. The decision should be made after discussing the risks and benefits with the doctor.
Weight control should be ensured. Obesity may increase the risk of uterine cancer.
Different factors contribute to different types of cancer. Although there is no proven way to completely prevent uterine cancer, you can reduce your risk. Talk to your healthcare team for more information about your personal cancer risk.
A form of birth control, a progestin-releasing intrauterine device (IUD), can be used.
FREQUENTLY ASKED QUESTIONS ABOUT UTERINE CANCER
There are frequently curious questions among uterine cancer patient comments. Frequently asked questions about uterine cancer can be listed as follows:
How is Uterine Cancer Surgery Performed?
Uterine cancer surgery may differ according to the patient and the spread of cancer. Uterine cancer surgery is usually performed by the method known as hysterectomy. Hysterectomy, popularly known as uterine removal surgery, can be performed by open method, laparoscopic (closed method) or robotic.
After the diagnosis of uterine cancer, surgical planning is made according to the stage of cancer and the patient’s body performance. Generally, surgery is performed in the first three stages of uterine cancer, while surgical method is not preferred in the last stage.
Uterine cancer surgery can be performed by combining several surgeries. Depending on the stage of uterine cancer, the surgeon may perform a simple hysterectomy (removal of the uterus and cervix) or radical hysterectomy (removal of the uterus, cervix, upper part of the vagina and nearby tissues). Depending on the age and menopausal status of the patients, oophorectomy is performed to remove the ovaries. If uterine cancer has spread to lymph tissues, these tissues can also be removed during surgery.
What is the Success Rate of Uterine Cancer Treatment?
Endometrium cancer is a disease that can be completely cured when diagnosed early. When caught in the early stages, patients have a 5-year life chance of 95%.
How is Uterine Cancer Screening Performed?
There is no screening test to detect endometrial cancer.
Is there a blood test for uterine cancer?
There is no known blood test for the diagnosis of uterine cancer
Does uterine cancer kill? Is uterine cancer fatal? Uterine Cancer survival times
Cancer is a lethal disease. The most important concept that determines life expectancy is the stage of the disease.
Is there a vaccine for uterine cancer?
There is no vaccine for uterine cancer.
Is uterine cancer contagious?
Uterine cancer is not contagious.
Does uterine cancer cause pain?
Uterine cancer can progress without causing any pain, but some patients may experience pain.
Can uterine cancer be transmitted to men?
Uterine cancer is not transmitted to men.
Does uterine cancer cause leg pain?
If the tumour has spread to the nerve area, it may cause leg pain.
How many hours does uterine cancer surgery take?
The duration of the operation varies depending on the extent of the disease, i.e. the stage and the skill of the surgeon.
How is Uterine Cancer Examination Performed?
After the diagnosis is made by biopsy, MRI can be performed to investigate the extent of the tumour.
Does uterine cancer recur?
Uterine cancer may recur.
What should be considered after uterine cancer surgery?
One of the most important issues to be considered after uterine cancer surgery is not to interrupt routine controls. In addition, attention should be paid to a healthy diet.
Where does uterine cancer metastasise?
Uterine cancer primarily spreads to surrounding tissues. It spreads to the lymph nodes and surrounding tissues in the pelvic region.
Can a person with uterine cancer have sexual intercourse?
There is no obstacle for uterine cancer patients to have sexual intercourse.
Is uterine cancer genetic?
Uterine cancer can be genetic. Especially those with a history of cancer in 1st degree relatives are in the risky group.
Can virgins get uterine cancer?
If there is a risk factor or family history, they can. However, uterine cancer is rare under the age of 40.
Is there a herbal treatment for uterine cancer?
There is no known herbal treatment for uterine cancer.
What should patients who have uterine cancer surgery pay attention to?
After uterine cancer surgery, it is important for patients to pay attention to their lifestyle and nutrition.
Can uterine cancer be detected on ultrasound?
Ultrasound imaging can provide suspicious data for uterine cancer. However, a biopsy should be performed for definitive diagnosis.
Can uterine cancer be detected in blood tests?
There is no known blood test for uterine cancer.
What is the age range of uterine cancer?
Uterine cancer is more common in the postmenopausal period.
Does uterine cancer cause low back pain?
Although rare, uterine cancer can cause low back pain.
Does spiral uterus cancer?
Spiral does not cause uterine cancer. Especially hormonal spirals can be protective.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS CERVICAL CANCER?

Cervical cancer is the most common gynaecological cancer in developing and underdeveloped countries. Every year, 500,000 new cases of cervical cancer are diagnosed worldwide. Cervical cancer, which usually occurs around the age of 50, has started to be seen in young women in recent years.
The HPV (“Human Papilloma Viruses”) virus, which is responsible for almost all cervical cancers, does not show many symptoms and is highly contagious. Most women defeat the HPV virus, which they have encountered at some point in their lives, with the help of their own body defence system. Some HPV viruses are stronger than this defence system and can cause cervical cancer. Taking precautions to protect against the HPV virus that causes the disease and having regular health checks and screenings helps to detect the disease before the disease occurs or in the early stages of the disease and helps success in treatment.
WHAT IS THE CERVIX?
The cervix, the lower part of the uterus, connects the uterus and vagina. The cervix, also known as the cervix, plays an important role in allowing fluids to pass between the uterus and vagina. It also allows the baby to pass through the vagina and leave the womb during labour.
WHAT ARE THE CAUSES OF CERVICAL CANCER?
Like many cancers, the exact cause of cervical cancer is unknown. Only some factors can facilitate the development of cervical cancer and accelerate the disease process. In general, the risk factors of cervical cancer are as follows;
- Being polygamous
- Sexual intercourse before the age of 20
- Smoking
- Weak immune system
- Frequent viral and bacterial infections in the genital organs
- Giving birth more
- Low socio-economic status
- Vitamin C and vitamin A deficiency
WHAT ARE THE TYPES OF CERVICAL CANCER?
Adenocarcinoma
There are different types of cervical cancer. There are many types of cervical cancer, including invasive cancers such as adenocarcinoma and squamous epithelial cell carcinoma. Among cervical cancers, adenocarcinoma, which is more difficult to detect and rarer, is a relatively aggressive type of cancer. Adenocarcinomas usually form in the inner canal of the cervix rather than on the outer surface of the cervix. Smear tests use cell samples from the outer surface. Therefore, by the time adenocarcinoma is diagnosed, the cancer is usually in an advanced stage. More adenocarcinomas occur with HPV types 16, 18, 45 and 31, which cause cancer.
WHAT ARE THE SYMPTOMS OF CERVICAL CANCER?
Symptoms of cervical cancer may not show themselves in the early period. Even in a gynaecological examination, the problem in the cervix may not be seen. After the high-risk HPV screening tests, which are cervical cancer screening tests, are positive or abnormalities are detected in the vaginal swab called smear test, changes can be detected with the instruments that enlarge the cervix called “colposcope”, and the definitive diagnosis can be made with a biopsy taken from the suspicious area.
Symptoms of cervical cancer occur mostly in the advanced stages of the disease.
Symptoms such as bloody discharge, bleeding after sexual intercourse and irregular menstrual bleeding are among the symptoms of cervical cancer. In advanced cases, the tumour can be detected even during examination. As cervical cancer progresses, urinary problems, difficulties in defecation and leg pain can be seen.
One of the symptoms of cervical cancer, bleeding that occurs unexpectedly immediately after sexual intercourse or the next day is called “postcoital bleeding”. Postcoital bleeding is an important finding and may be an early sign of cervical cancer.
Genital warts caused by HPV are not considered a sign of cervical cancer. Because while some types of HPV cause genital warts, some types cause changes in the cells of the cervix in women. However, a detailed examination and HPV typing should be performed due to the possibility of possible high-risk HPV types with the detection of genital warts. A cervical swab is taken to determine whether the person has HPV infection. According to the results of the examination, it can be determined whether HPV infection is present or not, and if so, its type.
Symptoms of cervical cancer, especially if it has progressed to advanced stages, can be summarised in this way;
- Urine and faecal leakage from the vagina
- Back pain
- Leg pain
- Loss of appetite
- Pelvic pain
- Swollen feet
- Weight loss
- Fatigue, weakness
- Bone pain and fractures
WHAT ARE THE RISK FACTORS FOR CERVICAL CANCER?
Among the causes of cervical cancer are giving birth, having sexual intercourse at an early age, having many partners and smoking. HPV infection has been observed in 98 per cent of cervical cancer patients. There are more than a hundred types of HPV, which is usually transmitted through sexual intercourse. Especially types 16 and 18 cause cervical cancer, while types 6 and 11 cause warts in the genital organs.
Polygamy, starting sexual intercourse before the age of 20, smoking, weak immune system, frequent viral and bacterial infections in the genital organs, multiple births, low socioeconomic status, vitamin C and vitamin A deficiency are among the risk factors for cervical cancer.
WHAT ARE THE PREVENTION METHODS AGAINST CERVICAL CANCER?
Cervical cancer prevention methods can be listed as follows:
- Have regular medical check-ups
- Get vaccinated against HPV
- Avoid smoking and tobacco products
- Strengthen the immune system
- Take precautions against sexually transmitted diseases
- Eat a healthy diet
- Take precautions against obesity
STAGES OF CERVICAL CANCER
The process leading to cervical cancer progresses as CIN 1, CIN 2, CIN 3 and then cervical cancer. Spontaneous regression of the disease can be seen in 70-90% in the first stage, 40-45% in the second stage and 30-35% in the third stage. In patients who do not receive any treatment, the disease turns into advanced cancer within years. In the early stages, there is no need to remove the uterus and complete recovery can be achieved by partially removing the cervix with simple surgical procedures called LEEP and conisation. These patients can get pregnant and have a baby after treatment.
The stages of cervical cancer can be listed as follows;
Stage 0: The abnormal cells are in the innermost layer of the cervix. It is also called carcinoma insutu.
Stage I: Cancer cells are found only in the cervix. The tumour size can vary between 3 mm and 4 cm.
Stage II A: The cancer has spread beyond the cervix to the upper two-thirds of the vagina but not to the tissues around the uterus.
Stage II B: The cancer has spread beyond the cervix to the upper two-thirds of the vagina and the tissues around the uterus.
Stage III A: The cancer has spread to the lower part of the vagina but not to the pelvic wall.
Stage III B: The cancer has spread to the pelvic wall or has invaded the ureters, the tubes connecting the kidneys to the bladder, blocking the passage of urine and causing enlargement of the kidneys.
Stage IV: The cancer has spread beyond the cervix to the bladder, rectum or other parts of the body.
CERVICAL CANCER VACCINE
HPV transmitted through sexual intercourse can cause cervical cancer. To protect against HPV, it is recommended that girls and boys between the ages of 9 and 26 and adults should be vaccinated against cervical cancer. Although 3 vaccines (9-valent, 4-valent and 2-valent vaccines) have received FDA approval and are being used in the USA, the 9-valent vaccine has not yet arrived in our country. The 2-valent vaccine contains virus-like particles of HPV types 16 and 18, which most commonly cause cervical tumours, and provides immunity against these types, while the 4-valent vaccine protects against warts by containing virus-like particles of HPV types 6 and 11, which cause warts in addition to these types. The latest vaccine, the 9-valent vaccine, contains virus-like particles of other high-risk HPV types 31, 33, 45, 52 and 58 in addition to HPV types 6, 11, 16, 18 in the 4-valent vaccine and provides a higher level of protection because it provides immunity against more HPV types that cause cervical cancer. These vaccines also provide some immunity against other HPV types in a cross-reaction.
Two doses of vaccine are sufficient for children between the ages of nine and 15. There should be a 6-12 month interval between the first and second dose of vaccines. In the 15-26 age range, 3 doses of vaccine are recommended at 0, 1 and 6 months. After the age of 26, vaccination is not recommended due to the high probability of encountering HPV until that age, but it can be done in appropriate cases by discussing this issue with the physician. HPV vaccine is administered intramuscularly. It can be administered from the shoulder or hip.
Getting the cervical cancer vaccine before you ever encounter HPV can prevent most cases of cervical cancer. In addition to cervical cancer, it is also protective against cancers of the vagina and vulva. 4 and 9 type vaccines can prevent genital warts and anal cancers in men and women. Since some HPV types are also associated with cancers that develop in the mouth and throat, it also provides protection against these cancers. The Centers for Disease Control and Prevention (CDC) recommends routine HPV vaccination for boys and girls after the age of 9. The ideal vaccination time for the cervical cancer vaccine is before sexual experience begins, that is, before contact with the HPV virus. When HPV is infected, the vaccine may not be as effective as getting it at the recommended time.
HOW IS CERVICAL CANCER DIAGNOSED?
Cervical cancer can be diagnosed by gynaecological examination in the advanced stage, and by colposcopic examination and biopsies performed as a result of detection of positivity in the high-risk HPV DNA test or abnormality in the smear test, which are screening tests in the early stage. In cervical cancer, which has a success rate of 80-85% when caught and treated at an early stage, biopsy is also very important in the diagnosis of the disease and for a correct treatment plan.
The first step in cervical cancer is to diagnose the cancer and determine the stage of the cancer. For this reason, a biopsy is taken from the cervix and cancer staging is performed. Staging of cervical cancer is defined according to the spread of the cancer in the body. Staging is based on pelvic and rectal examination in addition to radiological studies and possible other diagnostic tests. Apart from smears and biopsies, these tests are used to diagnose cervical cancer;
WHAT IS A SMEAR TEST?
The smear test is an extremely simple and painless cancer screening method. It is very important for women to have a smear test to prevent cervical cancer. Smear test is performed in two ways. In the classical method; the discharge taken is applied on a glass and sent to the laboratory after being detected with a special spray. In the second way; the material taken is poured into a special liquid in a bottle. In this way, it is sent to the laboratory where it is microscopically examined through certain stages.
All women over 21 years of age who have started an active sexual life should have a smear test. If active sexual life started before this age, it is recommended to have a smear test within the first three years from the age of initiation. In patients with a normal smear test, if there are no other risk factors, a test every 3 years is sufficient. Tests should not be interrupted even during menopause. After the age of 65, smear tests can be discontinued with the knowledge of the doctor if the patient has at least three normal smear test results by that time. In addition, if the smear test shows a suspicious situation, the test can be performed more frequently or further tests can be performed.
Colposcopy: It is the examination of the epithelium lining the cervix by looking at the cervix with a special binocular-like instrument. Cervical cancer does not start in one day. The deterioration of the cells increases gradually over time. It is possible to see and follow these changes with colposcopy examination. If the colposcopy examination is evaluated together with the smear, the error rate decreases significantly.
These tests are also used in the diagnosis and staging of cervical cancer;
Rectovaginal examination; In this test, the rectum and vaginal area are examined at the same time. It is a simple pelvic examination that can be performed under examination room conditions. It is understood whether the cancer has spread outside the cervix.
CT scan; CT scan, also called computed tomography, starts with the intravenous injection of a radiopaque substance. This substance provides better visualisation of internal organs in x-rays.
MRI (Magnetic Resonance Imaging) scan; This test uses magnetic radio waves and a computer to image internal organs and tissues.
PET (Positron Emission Tomography) scan; Radioactive glucose is injected into the vein, and the areas of the body where glucose is used at a high rate are determined in PET. Cancer cells are more active than normal cells and use more glucose. Cancer cells appear brighter in this test.
In addition, a chest X-ray and blood count may be requested to determine the spread of cancer to the breast or lungs.
HOW IS CERVICAL CANCER TREATED?
Genital warts caused by HPV virus infection can be treated by burning, freezing, surgery or local creams. The disappearance of the wart as a result of this treatment does not mean that it will not appear again. In some people, the wart does not recur after treatment; in some people, wart formation can be observed at frequent intervals. Treatment should be repeated for each new wart formation. The risk of recurrence of genital warts depends on how strong the immune system is. In HPV virus infections, it is known that the person can spontaneously eliminate the virus from the body without treatment.
In the treatment of cervical cancer, surgical intervention, radiotherapy and chemotherapy are used alone or in combination with each other. If the pre-cancerous lesion (CIN 2-3) has not passed into the depth of the tissue, the area of the cervix can be determined by colposcopy. By surgically removing the area, the area that may become cancerous is eliminated and a high rate of recovery is achieved in the patient. With a simple surgical procedure, the patient can be discharged on the same day. If the cancer has become invasive, that is, if it has gone deep into the tissue, there are two treatment options. In this case, a “radical hysterectomy” is performed, which is an extensive and difficult operation that will take a long time. At the same time, since the cancer cells have invaded the lymph nodes in the pelvic region, they are also removed.
The alternative is chemo-radiotherapy; cancer cells in that area are sensitised to the radiation with chemotherapy drug, then radiotherapy is applied to the patient and follow-up is continued. If it is in the late stage, chemotherapy is given, but the cure rate in these patients is considerably reduced.
WHAT IS HPV, HOW IS IT TRANSMITTED?
HPV is a sexually transmitted virus and can cause cervical cancer. HPV (Human papilloma virus), which is seen in more than 95% of women diagnosed with cervical cancer, is a virus that infects the genital area and spreads through contact. It causes warts in the sexual area, especially more frequently in women, and cancer in the cervix, external genital area and reproductive tract. The HPV virus is quite insidious and can continue to spread for months without showing any symptoms. Symptoms of the virus are called “silent infection” when they are observed several months or years after infection.
The HPV virus can cause genital warts in men and women, cervical cancer in women, and penile cancer in men. HPV, an infection that should be taken seriously, can be controlled by the immune system of some people. It should not be forgotten that a virus that cannot be neutralised by the immune system can maintain its existence for years without any symptoms. A person can carry the infection for years without any complaints. This does not prevent the spread of the disease, and the virus can continue to be transmitted during intercourse.
HPV virus types are divided into risk groups according to the possibility of causing cervical cancer. The types that cause more warts are in the low risk group for cervical cancer. Therefore, it is not the case that every genital wart will turn into cervical cancer.
GENITAL HERPES TREATMENT
Warts caused by HPV virus infection can be treated by burning, freezing, surgery or local creams. The disappearance of the genital wart as a result of this treatment does not mean that it will not occur again. While genital warts do not recur in some people after treatment; in some people, genital wart formation can be observed again at frequent intervals. Treatment should be repeated for each new genital wart formation. In HPV virus infections, it is known that the person can spontaneously eliminate the virus from his/her body without treatment.
Cervical cancer after treatment
Depending on the stage of the cancer and the type of treatment, cervical cancer may not disappear or may reappear after treatment. A new cancer may also develop elsewhere in the body. This is why routine check-ups and smear tests are important even after treatment has finished. Your doctor may ask you to have more frequent smear tests in the first few years after treatment. This is done to make sure that all cancer cells have disappeared. Other tests and procedures may also be needed. Your doctor will work with you to plan the check-ups you need even after treatment is finished.
FREQUENTLY ASKED QUESTIONS ABOUT CERVICAL CANCER
Is Cervical Cancer Contagious?
The biggest factor causing cervical cancer is HPV. This virus was detected in 99.7% of patients. Although cervical cancer is not contagious, HPV is the most common sexually transmitted virus. There is a high rate of contagiousness of 60% after sexual contact with people with warts in the genital area.
HPV can be transmitted sexually at a very high rate; at very low rates, it can be transmitted by hand contact, toilet and personal hygiene materials. Multiple partners have a high risk of HPV contagiousness.
What are the First Symptoms of Cervical Cancer?
Among the first symptoms of cervical cancer, symptoms such as bloody discharge, bleeding after sexual intercourse and irregular menstrual bleeding can be seen.
Where Does Uterine Cancer Pain Hit?
Cervical cancer may present with symptoms such as back pain, leg pain, pelvic pain, bone pain. In addition, pain and compression sensation in the lower abdomen, pain during sexual intercourse, weight loss can also be seen.
Can Cervical Cancer Be Felt by Hand?
During manual examination, the doctor places two fingers inside the vagina and the other hand on the lower abdomen. In this way, the organs and any palpable mass can be felt.
At what stage does uterine cancer show symptoms?
Symptoms of cervical cancer appear in the advanced stages of the disease. In advanced stages, the tumour can be seen during examination. As cervical cancer progresses, urinary problems, difficulties in defecation and leg pain can be seen.
At what age does cervical cancer start?
Cervical cancer, which usually occurs around the age of 50 during menopause, has recently been seen in young women. Although breast cancer ranks first in the ranking of common cancers in women, cervical cancer can surpass breast cancer due to its life-threatening characteristics.
What is evident in a smear test? Can Cervical Cancer Be Detected?
Smear test is performed to detect changes in the vagina before they turn into cancer. In this way, the woman can easily get treatment before she reaches the cancer stage. Women may need to have a smear test in the routine determined by gynaecologists.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT ARE OVARIAN CYSTS?
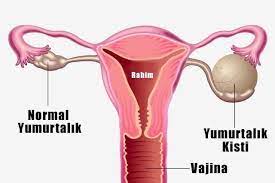
The incidence of ovarian cysts varies according to age groups. Different cysts are encountered during adolescence, reproductive age or menopause. Ovarian cysts seen according to age groups can be classified as follows:
Functional cysts: Cysts in the period between the ages of 13-18, called the adolescent period, are mostly functional cysts, usually do not require surgery and disappear over time. Since the hormone balance of the body has not yet settled in this period, the body can form temporary cysts. Functional cysts should generally be followed up. Because even if it is unlikely, ovarian torsion or cyst rupture may occur due to the weight created by the cyst. Apart from this follow-up, there is no need for any drug treatment. Functional cysts can also be seen during fertility.
Germ cell tumours: These are ovarian tumours that can be seen in adolescence and the first years of reproductive age. While surgery is sufficient in some types determined at diagnosis, chemotherapy treatment may be required in addition to surgery in some types. They are solid cystic masses that mostly manifest themselves as solid organs. It can be easily determined whether it is a functional cyst or a solid cystic mass by ultrasound control.
Corpus luteum cysts: These are cysts seen during menstrual period. It occurs with ovulation (ovulation). It disappears almost completely, sometimes it may cause bleeding.
Dermoid cysts: It is common during pregnancy. They are cysts containing ectodermal tissues such as skin, hair, fat, bone, teeth in the external structure of the body. Dermoid cysts can create weight in the patient very quickly and become cysts that require urgent surgery with torsion, i.e. ovarian rotation. In the past, all of the ovaries were removed in case of torsion, but nowadays the ovarian torsion can be restored and the cystic mass causing it can be removed. Most of the time, ovarian functions are restored with this method. If there are no serious delays, it is a problem that can be solved without removing the ovaries.
Chocolate (endometriotic) cysts: Endometriotic cysts, popularly known as chocolate cysts, are so named because their structure resembles melted chocolate. They are the most common special cysts during the reproductive period. Chocolate cysts are actually the formation of endometriosis in the ovary. Chocolate cysts are seen in one out of every 10 women in the fertile period. In these cysts, surgery is much more selective. Because chocolate cysts are mostly seen in women in the fertile period. In other words, patients have plans to become a mother. For this reason, surgery is not recommended immediately in chocolate cysts. However, surgery is required if the patient complains of pain. If the cyst is very large, such as 9-10 cm in size, surgery should be preferred if it no longer causes pelvic pressure. However, for example, if the size is 5 cm, there is no suspicious irregularity on ultrasound, and it is a homogeneous chocolate cyst, it is followed up. Because these cysts can recur unless a very successful surgery is performed. And ovarian reserve may decrease during surgery. For this reason, depending on the appearance on ultrasound, surgery should be avoided and followed up as much as possible, especially if the patient has a desire to have children. However, if CA-125, a tumour marker taken from the blood, shows an increase in the blood, surgery is required in these patients. The risk of cancer is low in chocolate cysts in reproductive age. As the age increases, the risk of chocolate cysts becoming tumoural increases.
WHAT ARE THE SYMPTOMS OF OVARIAN CYSTS?
The most important symptom especially in young age group cysts is groin pain and menstrual irregularity. In chocolate cysts, complaints of inability to have children especially during the fertility period, very painful periods that occur later, pain during intercourse in sexually active women can be seen. Sometimes painful defecation may occur when the intestines are involved. Difficulty in urination may be observed. Different complaints about the organs in the pelvic region called the pelvic region may occur. However, the most common symptom is the inability to conceive. In addition, long-lasting groin pains are also very common. In menopausal tumour cysts, abdominal swelling, frequent urination due to pressure on the organs in the region, constipation complaints, the onset of vaginal bleeding in menopause, sometimes called “postmenopausal”, and complaints such as abdominal pain are symptoms encountered during menopause, especially in large-sized tumours. In addition to these, there may be cysts that do not cause any symptoms and are detected incidentally during routine controls.
HOW ARE OVARIAN CYSTS DIAGNOSED?
The first diagnostic tool is physical examination. In physical examination, the abdomen is examined manually. Painful areas are detected. Afterwards, the most important imaging tool is ultrasonography. Ultrasonography evaluates the size, appearance and structure. In necessary patients, blood tests called tumour markers are performed or supported by MRI. MRI is not requested in every cyst. It is requested in suspicious cases. In case of suspicion of cancer, MRI (MRI) can be applied to see whether it has spread to different areas. In addition, tumour tests in the blood play an important role in the diagnosis. In ovaries, especially in serous cancers and chocolate cysts, CA-125, CA-19-9 in mucinous ovarian tumours, Alpha Feto protein (AFP), Beta-HCG in germ cell tumours seen at an early age, LDH blood test in some specific tumours may also be useful.
Although the risk of cancer in the young age group is low, it is necessary to first determine whether there is cancer in the presence of any complex cyst. Therefore, surgery is generally recommended for all non-functional cysts in the young age group. Functional cysts are kept under follow-up. If the patient is in menopause or close to menopause, that is, cysts seen after the 40s are cysts that are slightly closer to the possibility of cancer. Especially in menopausal patients, factors such as whether the structure of the cyst is regular on the ultrasound image are evaluated. Generally, if a cyst is detected during menopause and it is not thought to be a functional cyst, surgery is recommended.
WHAT IS THE TREATMENT OF OVARIAN CYSTS?
In the presence of a cyst, a combined evaluation is made with ultrasound findings, patient complaints, laboratory tests and other imaging methods if necessary, and a decision is made on the follow-up protocol or surgical intervention. There are ultrasound findings that determine whether the cyst is benign or malignant. These are; the size of the cyst, the structure of the surrounding tissue called the cyst wall, the presence of disorganised tissues such as papillary protrusions and nodular structures. For example, if there are solid areas, i.e. complicated cysts, these should be especially suspected. In these cases, surgery should generally be preferred and pathological examination should be performed during surgery. If it is found to be benign, only the cyst is removed and no other intervention is performed.
However, if it is found to be malignant in pathological examination, then conservative surgery or cancer surgery should be performed depending on the patient’s age and whether the patient plans to have children or not.
If the cyst does not require surgery and is only to be followed up, it is checked at 3 or 6 month intervals. If surgery is to be performed, closed methods such as laparoscopy or robotic or open surgery are applied depending on the size of the mass, its location, whether it is in both ovaries, and the patient’s desire to have children.
If the patient is very uncertain whether the finding is a tumour or not, the closed laparoscopic method can be applied first to see the structure of the mass. However, if it is a large mass, if the presence of a tumour is considered first and if it is widespread, that is, if there is a mass in both ovaries, then open surgery is preferred.
In the treatment of functional cysts, a follow-up protocol is applied. Cysts of patients with no clinical problems, pain or other complaints can be followed up for a long time. In these patients, the patient is only informed about the risk of ovarian rotation, that is, the risk of torsion, and intervention is performed when there is an emergency. Functional cysts or cysts that are not considered cancerous often disappear spontaneously. If they do not disappear but start to increase in size, then they are removed from follow-up and surgical treatment is started.
FREQUENTLY ASKED QUESTIONS
- Does an ovarian cyst prevent conception?
Depending on the type, ovarian cysts can be an obstacle to conception. In general, ovarian cysts that have not progressed too far (uncomplicated) are removed after a successful surgical intervention and the obstacle to conception disappears.
- What should patients with cysts under follow-up do in case of an emergency?
If the patient knows that she has a cyst, she is informed by her doctor whether the cyst is on the right or left side. However, the pain in the region can be reflected on both sides. For this reason, in case of any pain in the abdominal region, for example, especially in cases of severe pain that comes and goes intermittently, the physician who follows the cyst should be contacted first, but if it cannot be reached, it is absolutely necessary to apply to the emergency room. If a different doctor is consulted, test results and ultrasound images should be reported to the doctor. In addition, oral nutrition should be stopped when pain starts. If pain is accompanied by nausea, vomiting or abdominal swelling, it suggests peritoneal irritation. In other words, it means that the cyst has come into contact with the abdomen. Again, these are symptoms that require urgent medical attention.
- Does an ovarian cyst cause bleeding?
Bazı yumurtalık kistleri oluşum yerlerine ve boyutlarına göre kanama ile kendini gösterebilmektedir.
- Yumurtalıklarda kist olup olmadığı nasıl anlaşılır?
Some ovarian cysts may manifest themselves with bleeding depending on their location and size.
- Does an ovarian cyst cause pain?
Yes, one of the most common features of ovarian cysts is pain.
- What causes an ovarian cyst?
Ovarian cysts can develop for many reasons. The most common cause is hormonal imbalances in the body. Ovarian cysts can also develop as a result of various ovarian infections, radiation exposure, tumors and some cellular disorders.
- What are the symptoms of chocolate cyst?
In chocolate cysts, complaints of inability to have children, especially during the fertility period, very painful periods that occur later, pain in intercourse in sexually active women can be seen. Sometimes painful defecation may occur when the intestines are involved. Difficulty in urination may be observed. Different complaints about the organs in the pelvic region called pelvic region may occur. However, the most common symptom is the inability to conceive. In addition, long-lasting groin pains are also common.
- What causes a chocolate cyst?
There are no direct causes of chocolate cysts, but there are factors that increase the risk. These are mainly genetic and environmental factors. It can also develop due to many different reasons such as weak immune system, flow of menstrual blood into the abdominal cavity and tissue differentiation.
- Does a chocolate cyst cause bleeding?
There is usually no bleeding in the presence of a chocolate cyst.
- Where does a chocolate cyst cause pain?
It may cause groin pain during menstrual periods or pain in the vaginal area during sexual intercourse in sexually active women.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
What is robotic surgery in gynaecological diseases?

In parallel with the advancement of technology, there are very important developments in surgical methods and surgical techniques all over the world. The main purpose of these developments is to perform surgeries more safely, to reduce complication rates and to minimise undesirable results related to surgery. The most important progress in this field is that surgeries that used to be performed as open surgery can now be performed with minimally invasive methods, that is, closed. The latest point of technology in closed surgeries is robotic surgery systems. Robotic surgery, to put it simply, is a closed surgery performed by means of robotic arms controlled by the surgeon. Compared to traditional laparoscopic surgeries, the robotic system has many advantages.
In which cases is robotic surgery applied in gynaecological diseases?
There is no situation in which robotic surgery should not be used in gynaecological diseases. Robotic surgery can be performed in all cases where laparoscopic surgery is appropriate. Robotic surgery can be applied in the surgery of uterus, cervix and ovarian cancers, removal of fibroids, hysterectomy, endometriosis surgery, ovarian cysts, urinary incontinence and uterine prolapse.
However, technically, there are some situations where the advantage of closed surgery over open surgery is reduced. In these cases, open surgery may be preferred instead of robotic surgery.
How is robotic surgery applied in gynaecological diseases?
Patient preparation in robotic surgery is very similar to the traditional laparoscopic method. After the patient is taken to the operating table and anaesthesia is given, the patient is placed in the gynaecological examination position with footrests. Then, a special needle is inserted into the abdomen through a tiny incision about 3 cm above the navel and the abdomen is inflated with carbon dioxide gas. When a pressure of approximately 15 mmHg is reached, the trocar (metal tube or sheath through which surgical instruments can enter and exit) is inserted into the abdomen through a 7 mm incision made 3 cm above the navel. The camera of the robotic system is advanced into the abdomen through the first inserted trocar and the first image of the organs in the abdomen is obtained. After this stage, the operating table is turned upside down at an angle of approximately 35 degrees. In order to prevent the patient from sliding down the table, the feet are fixed on the footrests and shoulder supports are placed on the shoulders. Depending on the type of surgery to be performed, as many trocars as the total number of robotic arms to be operated with are placed under the image of the first entered camera.
However, technically, there are some situations where the advantage of closed surgery over open surgery is reduced. In these cases, open surgery may be preferred instead of robotic surgery.
Myomectomy : The robotic system provides a great advantage in the surgical treatment of fibroids, which is a problem that can be seen in a significant number of women of reproductive age. The most important step in fibroid surgery with the closed method is to close the incisions in the uterus in a solid and multi-layered manner after removing the fibroids. Failure to close the incisions in the uterus properly after fibroid removal increases the risk of uterine rupture in subsequent pregnancies. In myomectomies performed with robotic system, since robotic arms can mimic wrist movements in all axes, suturing the incisions is much easier and more reliable.
Hysterectomy : All hysterectomy procedures suitable for closed surgery can be performed with the robotic system. Thanks to the three-dimensional and high quality image, the possibility of unwanted situations that may occur during hysterectomy surgery is reduced. After the uterine ligaments are cut robotically, the top of the vagina is cut all around and the uterus freed from all its connections is taken out of the vagina. The incision site in the vagina is also closed robotically or vaginally.
Endometriosis : Endometriosis is a condition that involves the uterus, tubes, ovaries and even the large intestine and causes serious adhesions, loss of function and pain in these organs. Endometriosis surgery requires experience and especially advanced endometriosis surgery is a long-lasting surgery. Robotic surgery provides significant advantages in this situation, which requires high concentration for long periods of time and the opening of adhesions in important organs without damaging the organs.
What are the advantages of robotic surgery in gynaecological diseases?
The advantages of Da Vinci robotic surgery to the patient can be listed as follows:
- Since the operation is performed with tiny incisions, the amount of bleeding in the patient is less
- Since the incision size is smaller than open surgery, the patient feels less pain
- Shorter wound healing time
- The patient’s hospitalisation time is shortened
- Complication rate is lower than open surgery
- The patient returns to daily and social life in a shorter time
- Since the recovery period is shorter, it allows oncological treatment to be started sooner after surgery
FREQUENTLY ASKED QUESTIONS ABOUT ROBOTIC SURGERY IN GYNECOLOGICAL DISEASES
How does robotic surgery differ from open and closed methods in gynaecological diseases? Why is robotic surgery preferred in gynaecological diseases?
Robotic surgery has certain advantages over both open surgery and traditional closed methods (laparoscopy).
Advantages compared to open surgery:
- Blood loss during surgery is much less
- Complication rates are lower
- Shorter recovery time, shorter hospital stay
- Postoperative pain is less
- It returns to normal life more quickly after the operation.
- The surgical scar is much smaller
Advantages over conventional laparoscopic surgery:
- The surgeon performs the operation in a much more comfortable position by sitting on the console. This allows the surgeon to continue the operation without getting tired and losing concentration even in long cancer surgeries. In conventional laparoscopic surgeries, the surgeon is much more physically challenged and experiences fatigue, physical pain and loss of concentration during prolonged operations.
- With the robotic system, the surgeon sees the operation field in 3D and in high quality. In the classical laparoscopic method, since the surgery is performed by looking at a 2-dimensional screen, the sense of depth disappears and in some cases this may cause problems.
- In the robotic system, the robotic arms in the patient are designed to simulate the surgeon’s finger and wrist movements with high sharpness. Thus, surgical instruments with 360-degree movement capability can be used with very high precision during surgery. This is not possible in classical laparoscopy.
- In the robotic system, the surgeon himself can control all the instruments and the camera in the patient, that is, the area where he works, as he wishes. In classical laparoscopy, the surgeon can control only two instruments at the same time. Another person manages the camera and the assistant instrument. Therefore, the success of the operation depends on the surgeon as well as the assistant.
- The controls in the robotic system completely prevent the surgeon’s hand tremors, providing a vibration-free and smooth instrument use.
How is the recovery process after robotic surgery?
In robotic surgery, 7 mm diameter instruments are used and robotic surgeries are performed through an average of 4 7 mm incisions. Therefore, the recovery period after robotic surgeries is extremely short.
Are there any risks associated with robotic surgery for gynaecological diseases?
Compared to the conventional laparoscopic method in gynaecological diseases, there are no risks specific to robotic surgery. Technically, although there may be malfunctions that may occur in the robotic system, they are extremely rare and in such cases, surgery can be continued with the traditional laparoscopic method. In other words, the risks that are likely to occur as standard in a surgery are also valid for robotic surgery.
Can robotic surgery in gynaecological diseases be applied in every patient?
Robotic surgery can be applied in all cases suitable for traditional laparoscopic surgery. Since some conditions may constitute an obstacle for closed surgery, robotic surgery is not suitable in these cases. These conditions are
- The patient has a medical condition that constitutes an obstacle for closed surgery (intracranial masses where intracranial pressure increase may be dangerous, serious lung and heart disease, etc.)
- Examples can be given if the disease planned for surgery is not suitable for closed surgery (such as ovarian cancer with intra-abdominal diffuse disease, mass or tumour occupying a large area in the abdomen)
How many days is the hospital stay after robotic surgery?
The hospital stay in robotic surgery is significantly shorter compared to open surgery. Considering that complicated cancer surgeries can also be performed with robotic surgery today, the duration of the patient’s hospital stay varies depending on the disease, the general condition of the patient and the procedure performed robotically. The hospital stay is usually 1 night for fibroids and hysterectomy surgeries and 2 nights for uterine cancer surgeries.
Does pain occur after the operation?
Pain after robotic surgery is much less than open surgery. The pain felt is usually felt for a short time at the trocar entry points. It can be controlled with non-strength painkillers.
Is it necessary to stay in intensive care after surgery?
The need for intensive care after robotic surgery varies according to the general condition of the patient, the severity of the disease and the procedure performed. Generally, there is no need for intensive care after robotic surgery unless otherwise.
What are the rates of use of robotic surgery in gynaecological diseases?
Robotic surgery is increasingly being used in the surgical treatment of gynaecological diseases, especially in North America. Approximately 30-40% of all closed uterine operations are performed by robotic method. As a result of robotic surgery systems that are rapidly becoming widespread in Europe, laparoscopic hysterectomy surgery has been decreasing over the years and robotic hysterectomy surgery has been increasing.
What should patients pay attention to after robotic surgery?
There is no special issue that patients should pay attention to after robotic surgery. Patients can take their bath a few days after the surgery. No special care is required for the stitches and patients do not need to have their stitches removed as absorbable materials are usually used.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
What is leep conisation?
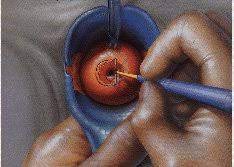
Leep conisation is a surgical procedure performed for both diagnosis and treatment in cases where CIN 2, CIN 3 (HSIL) is detected in patients undergoing colposcopy / biopsy during routine gynaecological follow-ups to detect cervical cancer precursor cells. Leep conisation procedure can be used to confirm the diagnosis and simultaneously used for treatment. Questions such as “What is Leep conisation?”, “What is Leep operation?”, “What is Leep procedure?”, “What is Leep treatment?”, “What is Leep surgery?”, “What does Leep mean?”, “What is Leep conisation?”, “What is Leep procedure?” are raised by patients. Conisation procedure can be applied in 2 ways as hot conisation (LEEP) and cold conisation. Hot conisation (LEEP) procedure is mostly preferred in the world and in our country.
In the hot conisation (LEEP) procedure, under anaesthesia, a special tool is used to cut and remove the cervix. In the cold conisation procedure, the cut is made with a scalpel. Cold conisation operation is mostly preferred for people diagnosed with early stage cervical cancer.
In which diseases is leep conisation applied?
Is the Leep conisation procedure only applied in the treatment of cervical cancer or precursor cells? The question is raised by patients. Leep conisation is a procedure that is generally applied to the cervix from gynaecological pain. It can be used for cervical cancer, or if there is an abnormal condition in the cervix, it can be used to reduce the cervix according to the patient’s complaint or to remove the diseased area to repair the cervix. However, leep conisation procedure is generally used in cervical cancer.
Why is leep conisation performed?
- Leep conisation surgery is usually performed for both diagnosis and treatment of cell changes in the cervix caused by HPV infection. It stands out as a surgical procedure especially for CIN 2 and CIN 3 diagnoses.
- In patients who have a biopsy with suspicion of cervical cancer, leep conisation surgery can be performed to clarify the diagnosis if there is doubt in terms of diagnosis.
- There is no need for leep conisation surgery in patients who undergo cervical biopsy and are diagnosed with cervical cancer. However, leep conisation may be considered in patients diagnosed with early stage cervical cancer. Cold leep conisation is generally preferred in patients
- As leep can be used in early stage cervical cancer, leep conisation operation can also be performed in cases where abnormal cells such as CIN are seen.
- In patients with advanced cervical cancer, it is sufficient to perform a biopsy procedure. LEEP technique is not used if the incision is diagnosed by biopsy.
- Whether LEEP procedure should be performed or not is decided according to the result of colposcopic biopsy. After the area determined by the LEEP procedure is removed, it is then sent to pathology.
How is leep conisation surgery performed?
- If abnormal cells are found in the cervical biopsy and it is decided to perform leep conisation, this procedure is performed under general anaesthesia.
- Leep conisation procedure is performed on the gynaecological examination table.
- Since the patient will receive anaesthesia, it is healthier to perform the procedure in the operating theatre environment.
- Leep conisation is a surgical procedure. After the patient is placed on the gynaecological table, the gynaecologist and obstetrician makes the cervix visible with a vaginal speculum used to examine the vaginal walls and vagina.
- The cervix is stained with a special solution and the surgical borders are determined.
- The affected part of the cervix is surgically removed. Since it is removed in the shape of a cone, the procedure is called Leep conisation.
- The surgically removed section is sent to the pathology laboratory to check for abnormal cell changes.
Frequently asked questions about Leep conisation
What is the price of Leep conisation surgery?
Questions such as “How much is the Leep conisation price?”, “How much is the Leep conisation fee?” are brought up by patients. Leep conisation fee may vary according to the price policy of the doctor and the hospital where the surgery will be performed, and the material to be used during Leep conisation surgery. Leep conisation surgery is a procedure performed safely by experienced gynaecologists and obstetricians. Before getting the answer to the question of how much is the price of Leep conisation surgery, it is necessary to choose the doctor, make a preliminary examination before the procedure and determine the road map for the best solution of the problem.
Will there be menstrual irregularities after Leep?
Questions such as “How will menstruation occur after Leep conisation?”, “When and how will the first menstruation occur after Leep conisation?”, “Will there be menstrual irregularities after Leep conisation?” are among the most curious topics. There is no change in the normal menstrual rhythm after leep conisation surgery. However, in the first menstrual cycle after leep conisation, the amount and duration of bleeding may be slightly higher. In case of excessive bleeding, it is necessary to consult a doctor.
Is there a suitable time to have leep conisation surgery?
- Leep conisation surgery can be performed at any time, but it is recommended to be performed immediately after the menstrual cycle to make both the doctor and the patient more comfortable. Performing it as soon as possible after the end of menstruation provides some advantages to the patient.
- After the leep conisation surgery, a bleeding-free period of 20-25 days ensures better tissue healing. Bleeding-free recovery period after the surgery can accelerate the healing process of the tissues. If leep surgery is performed close to the menstrual period, the amount of bleeding will increase more and healing will be later. This will impair the patient’s quality of life.
- Performing leep conisation surgery during menstrual bleeding may also pose a risk in terms of infection.
How long is the recovery period after Leep conisation surgery?
Recovery after Leep surgery takes approximately 4-6 weeks.
What does the Leep conisation pathology result show?
- The pathology evaluation performed after the Leep conisation procedure is compared with the biopsy results. It is checked whether the pathology of the area removed in the Leep conisation procedure is parallel to the biopsy results.
- The depth of the lesion and whether the surgical margin is normal are checked. It is checked whether there are cancer cells in the depth of the tissue.
- It is checked whether the surgical margin is clear in terms of the continuity of the lesion. If the surgical margin is clear, adequate surgery is performed.
- Leep conisation pathology result shows whether the diagnosis is in the right place and whether the treatment is adequate.
- Pathology is also decisive in determining the road map in the later stages of treatment.
What should be considered after leep conisation surgery?
- The patient can stand up on the same day after the leep surgery. Since the surgery is performed under general anaesthesia, the patient can return to social life after a 1-2 hour rest period.
- Intra-abdominal pressure should not be increased for 1-2 days after leep conisation surgery. It is especially important to avoid straining in the toilet.
- There is a recovery period of approximately 4-6 weeks after Leep surgery. There should be no sexual intercourse during this period.
- It is important to pay attention to hygienic conditions to avoid infection.
- There may be spot-like bleeding after Leep conisation surgery and this does not indicate a problem. However, it is necessary to consult a doctor in case of falling pieces or excessive bleeding.
- There is no restriction on bathing after Leep surgery.
How many days does bleeding last after Leep conisation surgery?
Questions such as “How long does bleeding last after Leep conisation surgery?”, “Does bleeding occur after Leep conisation?”, “How long does bleeding last after Leep?” are among the topics wondered by patients.
There may be no bleeding after Leep conisation surgery. If there is bleeding after the operation, this bleeding is usually in the form of stains. Spot-like bleeding should be considered normal. This type of bleeding may last for 15 days.
After the leep conisation procedure, there may be a discharge process due to tissue shedding. The important thing here is that the discharge is not infected. Hygienic conditions should be observed.
When is sexual intercourse after Leep?
There should be no sexual intercourse in 4-6 weeks, which is the healing process after Leep conisation surgery. Before starting sexual intercourse, the doctor should check and then decide.
Can pregnancy occur after Leep conisation surgery?
Questions such as “Will there be pregnancy after Leep?”, “Will there be pregnancy after Leep?”, “Pregnancy after Leep conisation” are among the most curious topics. Leep conisation surgery is not performed on a pregnant woman. After leep conisation surgery, there is no problem in terms of pregnancy. Although there is no condition that prevents pregnancy, there is a risk of premature birth in those who have leep conisation surgery. Although this risk is low after the leep procedure, the risk of premature birth may occur due to shortening of the cervix.
Is there a recurrence after leep conisation?
Patients raise the question of whether Leep conisation surgery can be performed a second time. Leep conisation can be performed more than once if necessary.
HPV infection can affect the cervix and cause abnormal cells to form. In such cases, leep conisation surgery can be performed a second time or even a third time if necessary. People with HPV infection and smokers are usually the group requiring a second intervention. Smoking is the most important risk factor for recurrence of HPV infection. In recent scientific studies, it has been stated that the possibility of complete removal of HPV infection from the body is very low. In cases where the immune system is weak, HPV infection reappears. Smoking is one of the most important factors that weaken the immune system. If smoking is present in the social life of the person, it is possible to encounter the abnormal cells caused by HPV infection again.
After leep conisation surgery, the first control is performed after 6 months.
Is leep conisation painful?
Leep conisation operation is not a painful procedure. Since the operation is performed under anaesthesia, the person will not feel pain. After the procedure, the patient may experience mild pain. However, the pain can be controlled with simple painkillers. There is no pain affecting the social life of the patient. There are usually no stitches in leep conisation operation. However, stitches can be used in cold leep conisation operation. This is completely surgeon’s preference.
What are the complications after leep conisation operation?
The most important complication after leep operation is bleeding. Excessive bleeding should be taken into consideration rather than stain-like bleeding. In the long term, there may be cervical incompetence in pregnancy.
Is there any smelly discharge after Leep conisation?
Odorous discharge after leep conisation surgery suggests the possibility of infection. However, even if it is not odorous after surgery, discharge may occur due to tissue shedding. In case of odorous discharge, it is necessary to consult a doctor.
How long does the leep conisation procedure take?
Leep conisation surgery is a surgical procedure that takes 15-20 minutes.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
Paediatric oncology

Cancer is the second most common cause of death in children and approximately 3 thousand children are diagnosed with cancer every year in our country. One out of every two children diagnosed with childhood cancers dies due to lack of treatment or delay in diagnosis. Thanks to early diagnosis and correct treatment practices, it is possible for the majority of children with cancer to fully recover.
The most important way to achieve success in childhood cancers is to treat these patients in full-fledged centres with infrastructure and service quality. Memorial Pediatric Oncology Centres serve to provide high-level diagnosis and treatment opportunities for children with cancer. For the diagnosis and treatment of all childhood cancers, pediatric oncologists, pediatric surgeons, orthopedics, neurosurgery, ophthalmology, ear-nose-throat departments, especially doctors specialised in tumours and tumour surgery are in cooperation.
MULTIDISCIPLINARY APPROACH IN THE TREATMENT OF ALL CHILDHOOD CANCERS
The most common types of cancer in children are leukaemia, brain tumours, lymphoma, kidney and adrenal gland tumours, soft tissue and bone tumours, some organ tumours and retinoblastoma (eye tumours). While public awareness of leukaemias is higher, awareness of solid tumours and lymphomas, which account for 75% of all childhood tumours, is lower. Childhood cancers can be more difficult to treat and early diagnosis is vital. In Pediatric Oncology Centres in our country, this challenging process is carried out very successfully with a team approach thanks to the cooperation of many specialities.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
What is Oncological Surgery (Cancer Surgery)?

Oncological (cancer) surgery is the removal of cancerous tumours or tissues from the body and cleaning the area from cancer. Oncological surgery, which has a 100-year history, has been performed classically open since its inception, and today it is applied with different techniques aiming to create smaller incisions in the body for both cosmetic appearance and shortening the healing time. Minimally invasive surgery called ‘small incision’, laparoscopic surgery performed closed through one or several holes and new generation surgeries performed with robotic systems, which are the most advanced point reached by technology, prioritise comfort while restoring the patient’s health.
What are the Objectives of Oncological Surgery?
The aim of oncological (cancer) surgery, which offers patients privilege, comfort and rapid return to daily life with great developments in the last 20 years, is to completely remove the tumour from the body. Here; timing and a very good organisation with other branches is required. Surgery is one of the most critical stages of the treatment process. In order to achieve a successful result in the treatment process, the disease should not recur at the site of the tumour and there should be no distant organ metastases, in other words, the disease should be completely eliminated. The exact equivalent of this is curative treatment. This is the primary and indispensable goal in cancer surgery. Open, laparoscopic (closed) or robotic methods are preferred among personalised treatment options in cancer surgery. In a successful cancer surgery, it is aimed to clean the cancerous cells in the most accurate way, as well as to make the patient feel less pain, to preserve all functions and to recover in a short time.
In Which Cancer Types Is Surgical Oncology Effective? What are the Diseases Treated?
Surgical oncology or cancer surgery is applied in the fields of General Surgery, Endocrine Surgery, Thoracic Surgery, Gynaecological Oncology, Urology, Brain and Neurosurgery, Head and Neck Surgery, Orthopaedic Oncology, Breast and Oncoplastic Surgery.
General Surgery
Breast and thyroid cancers, liver tumours, gallbladder and biliary tract cancers, pancreas and main region tumours, stomach, colon and rectum cancers and oesophageal tumours are treated.
Thoracic Surgery
Palliative methods in lung and pleural cancers, tumours of the chest wall, tumours of the respiratory tract and mediastinum, advanced stage cancers of the lung and other organs, interventional procedures and stent applications in lung and respiratory tract tumours are performed.
Gynaecological Oncology
Also known as female cancers; uterine, cervical, ovarian, ovarian, tubal, vulva and ovarian cancers are operated.
Urology
Laparoscopic and robotic surgery of prostate cancer with nerve-sparing methods, bladder tumour surgery and closed surgical applications of new bladder reconstruction, kidney tumour surgery and kidney-sparing methods, surgery of adrenal gland cancers and testicular tumours are performed.
Brain Surgery
Surgical interventions are performed with microsurgical and endoscopic techniques in childhood brain and nerve tumours, pituitary tumours and tumours of the skull base. In the surgery of tumours located in the sensitive area of the brain, neuromonitoring technology is used against the risk of postoperative paralysis.
Head and Neck Surgery
Surgical treatment of tumours of the larynx, pharynx, paranasal sinus and nasal cavity, tonsil and salivary gland cancers, oral cavity, floor of the mouth, tongue, the upper part of the throat, the area connecting the rest to the throat, the lower part of the throat and the area below it, the auricle and the external auditory canal.
Orthopaedic Oncology Department
Tumours originating from the bone itself, bone metastases of other organ tumours, malignant tumours of the tissues forming the skeletal system, soft tissue tumours including muscle, adipose tissue, connective tissue, vessels and nerves, and all skeletal system tumour surgeries in childhood and adulthood are performed.
Breast and Oncoplastic Surgery
Special surgeries combining oncological and aesthetic surgery are applied in order to eliminate breast loss of breast cancer patients not only due to cancer diagnosis but also after breast surgeries. By combining the principles of oncological and plastic surgery, comfortable options are offered for patients who have previously experienced breast loss due to cancer.
In which cases can cancer surgery not be performed?
Surgical treatment of cancer is no longer a single treatment method and has become one of the most important parts of an organised treatment process. With the effect of technology on cancer surgery, cancer has become a disease that can be fought more actively for all surgeons in this field. Thanks to the surgeries that have come to the agenda for both doctor and patient comfort, the number of operations that cannot be performed has gradually decreased and intervention in organs with immunity has become relatively easier. In the surgery of pancreatic cancer, which is the best example of this, in addition to the artificial vascular surgeries performed to prevent the tumour from involving the nearby vessels, with very effective drug regimens in oncology, patients can be operated by first shrinking the tumour in cases of pancreatic cancer or metastasis to the liver, which are considered inoperable. Cancer surgery is a form of treatment that prolongs the quality and duration of life as it should be.
However, despite all these developments, not all cancers are operable. Surgery is an option for solid organ tumours and non-operative treatment methods are used for blood cancers. However, again, the tumour must have certain characteristics in order to be surgically removable. In cases where the tumour is too large to be removed by surgery, distant organ metastases affecting the general health status of the patient, surgery may not be an option for patient groups who cannot tolerate the complications of surgery due to advanced age. In such cases, non-surgical treatments may be preferred to reduce the tumour and make it operable, as well as supportive treatments for surgery as a preventive measure to eliminate the risk of cancer cells remaining after surgery. If gastric cancer is caught at an early stage, almost all patients can be cured of the disease by surgery. However, different treatment alternatives come to the fore for people with advanced pancreatic cancer and some chronic diseases. Therefore, in order to apply the right treatment method, it is important to choose the patient correctly and to determine the order of application of the treatment. Proper management of the treatment of patients diagnosed with cancer under the roof of a cancer centre will positively affect the results of the treatment.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS MOUTH CANCER?

Oral cancer is the growth of abnormal cells anywhere in the mouth or lips. While catching oral cancers as early as possible is extremely important for the success rate of treatment, surgery is at the forefront in the treatment of tumours in this region. Surgery should be performed as wide as possible, safely, leaving a surgical margin and the surgical area removed during the operation must be supported by pathology (frozen). In some cases, chemotherapy can be applied in addition to surgery. In the treatment of a cancer in the mouth, neck dissection (except hard palate) is absolutely necessary.
WHAT ARE THE RISK FACTORS FOR ORAL CANCER?
The risk of oral cancer increases in long-term and intensive users of tobacco and tobacco products. As a matter of fact, it has been found that approximately 75 per cent of people with oral cancer use tobacco. As the amount and duration of tobacco use increases, the risk of oral cancer also increases. Excessive alcohol consumption, too much exposure to the sun, being over the age of 40, and being obese also increase the risk of oral cancer. People with a history of head and neck cancers have an increased risk of developing oral cancer, especially if they continue to smoke and drink alcohol. In addition, HPV infection, ultraviolet rays, malnutrition, weakened immune system, having certain health problems such as graft-versus-host disease or fanconi anaemia and poor oral hygiene are among the factors that increase the risk of oral cancer.
Note: People with mouth cancer are more likely to develop cancer of the larynx, oesophagus or lung.
WHAT ARE THE TYPES OF MOUTH CANCER?
Oral cancer is categorised according to the cell type in which the cancer (carcinoma) starts to grow. Squamous cell carcinoma is the most common type of oral cancer, accounting for 9 out of 10 cases.
Less common types of oral cancer include
- Adenocarcinoma, which are cancers that develop inside the salivary glands
- Sarcoma growing from abnormalities in bone, cartilage, muscle or other tissues
- Oral malignant melanoma in which cancer begins in the cells that produce skin pigment or colour (melanocytes). These appear as very dark, mottled bumps that often bleed.
- Lymphoma, which develops from cells usually found in the lymph nodes. (They can also grow in the mouth.)
On the other hand, oral cancer is a type of cancer under the umbrella of ‘head and neck cancers’. Other types of head and neck cancers include
- Larynx cancer
- Nasopharyngeal cancer (the area behind the nose (pharynx) that forms the upper part of the throat)
- Oropharyngeal cancer
- Hypopharyngeal cancer
- Thyroid gland cancer
- Nasal and sinus tumours
- Oesophageal cancer
WHAT ARE THE SYMPTOMS OF MOUTH CANCER?
If any of the symptoms of oral cancer lasts more than 2 weeks, it is important to consult a doctor immediately. The symptoms of oral cancer can be listed as follows:
- Non-healing mouth / lip sores
- Lump or swelling in the mouth
- White or red patches in the mouth
- An area inside the mouth that discolours and stays that way
- Lumps or thickening of the cheeks
- Sore throat that has not healed for a long time
- Voice hoarseness
- Bad breath
- Chewing or swallowing problems
- Inability to move the jaw and tongue
- Numbness of the tongue or part of the mouth
- Pain around the teeth and in the jaw
- Unexplained weight loss
- Constantly feeling that something is stuck in the throat
HOW IS MOUTH CANCER DIAGNOSED?
Diagnosis of oral cancer begins with a physical examination. With or without symptoms, the dentist may notice an abnormal tissue change in the mouth, feel a lump or mass during a routine check-up.
Direct examination of the lesion or a small biopsy may lead to a diagnosis. Once diagnosed, the doctor will use various tests to determine whether the cancer has spread beyond the oral cavity and the extent of the cancer. Tests may include
- MRI scan of the head and neck
- CT scan of the breast to look for cancer in the lymph nodes
- Positron Emission Tomography (PET) scan to look for cancer in other parts of the body
- The doctor can also look at the larynx, oesophagus and lungs by sliding a tube with a small camera at the end down the throat.
HOW IS MOUTH CANCER TREATED?
Oral cancer treatment practices may vary depending on the general health condition of the patient, the location and stage of the cancer. Surgery, the most common treatment for oral cancer, involves removing the tumour and some surrounding healthy tissue. In cases where cancer cells have spread to the lymph nodes, the surgeon will remove them to prevent the cancer from spreading to other parts of the body. One of the most exciting new developments in oral cancer treatment is the widespread use of robotic surgery.
Radiotherapy is the primary treatment for some small tumours. Radiotherapy uses high-energy x-rays to kill cancer cells. In some cases, patients who have undergone surgery receive radiotherapy to remove cancer cells that may have remained in the body at microscopic level after surgery. Even when radiotherapy cannot cure the cancer, it can relieve symptoms such as bleeding and difficulty swallowing.
If needed, doctors may use chemotherapy to shrink tumours before a surgical procedure. If the tumour is too large to be operated on, chemotherapy and radiotherapy can relieve the symptoms caused by the cancer.
If the cancer is diagnosed at an earlier stage (Stages I and II), the chances of recovery are much better. This is because tumours at these stages are smaller than 4 centimetres at their widest point and have not spread to the lymph nodes. Cancer patients at these stages can be treated with surgery and radiotherapy. Stage III and IV tumours are more advanced. At these stages, tumours are treated with radiotherapy, chemotherapy or both, as well as more extensive surgical procedures. Targeted drug therapy can also be used alone or in combination with chemotherapy-radiotherapy.
Immunotherapy uses drugs that help the immune system fight the cancer.
Immunotherapy can be applied to people with advanced oral cancer that does not respond to standard treatments.
FREQUENTLY ASKED QUESTIONS ABOUT MOUTH CANCER
How can the risk of oral cancer be reduced?
Although there is no proven method to prevent oral cancer, the risk of developing oral cancer can be reduced by taking the following recommendations into consideration.
Tobacco use should be stopped or should not be started: Tobacco use increases the risk of oral cancer. Smoking and chewing tobacco exposes the cells in the mouth to dangerous chemicals that can cause cancer.
Alcohol users should consume in moderation: Excessive alcohol consumption can irritate the cells in the mouth, making them vulnerable to oral cancer. Therefore, excessive alcohol consumption should be avoided.
Excessive sun exposure should be avoided: Stay in the shade as much as possible and use sunscreen cream as a base layer to protect the lips from the sun’s harmful rays. A wide-brimmed hat that effectively shades the entire face, including the mouth, should be worn.
A well-rounded, healthy diet with a variety of fruit and vegetables can also reduce the risk of mouth cancer.
What is supportive care for oral cancer?
Supportive care helps to address the physical, practical, emotional and spiritual challenges of oral cancer.
There are many programmes and services available to help meet the needs and improve the quality of life of people living with cancer and their loved ones, especially following treatment.
Recovering from oral cancer and adjusting to life after treatment is a different process for each individual, depending on the location of the tumour, the stage of the cancer, the organs and tissues removed during surgery, the type of treatment and many other factors. Even when treatment is over, there may still be issues such as coping with long-term side effects. A person undergoing treatment for oral cancer may have the following concerns.
Self-esteem and body image
How a person feels about themselves is defined as self-confidence. Body image is how a person sees their own body.
Oral cancer and its treatments can affect a person’s self-esteem and body image. This is usually due to the following factors:
- Scars
- Skin changes
- Changes in face shape
- Having to use a prosthesis
- Difficulty speaking or eating
- Weight loss
Some of these changes may be temporary, while others may last for a long time or become permanent.
Some individuals may avoid socialising even if the effects of treatment are not visible outside the body. This is because they may be afraid that others will judge them and they may be afraid of experiencing a sad or angry emotional outburst.
Those affected by your appearance after oral cancer surgery need to give themselves time. Talking to someone who has had a similar experience, family support, socialising with friends can help the individual. There are also tools that can help with facial changes, such as camouflage make-up for scars or wearing scarves and hats.
Dry mouth
Many people will experience dry mouth during and after treatment for oral cancer. Radiotherapy or a surgical procedure that damages the salivary glands can cause dry mouth. Chemotherapy given in combination with radiotherapy can often exacerbate the complaint of dry mouth.
Intensity modulated radiotherapy (IMRT) can help reduce this complication in many patients.
Difficulty chewing and swallowing
Oral surgery, especially if it involves the removal of certain structures such as the tongue and jawbone, can cause difficulty chewing and swallowing. In some cases, it may be necessary to have reconstruction or dentures to replace a structure inside the mouth. Ways to improve swallowing include changing your head posture and doing range of movement exercises for the jaw and tongue. A feeding device called a glossectomy spoon allows a person with only part of their tongue to put soft food in the back of their mouth. This also helps with swallowing.
Speech problems
Surgery to remove large parts of the tongue, jaw bones or palate can cause speech problems. Reconstruction helps to reduce these complications, but it is often difficult to restore normal function. Mouth prostheses can compensate for tissue lost during surgery and help improve speech.
A speech therapist can assess speech problems and help manage them.
Flavour changes
Radiotherapy to the head, neck or mouth can damage the salivary glands and taste buds on the tongue, which can affect the way some foods taste. Chemotherapy drugs can also affect the taste cells in the mouth. Surgery to remove part or all of the tongue can cause a reduced or lost sense of taste.
Tooth problems
Radiotherapy can cause dental problems. Saliva helps to clean the teeth and gums, so when less saliva is secreted, there is a higher risk of developing caries and gum disease. Radiotherapy can also affect tooth enamel. This increases the risk of tooth decay.
A check-up with the dentist is recommended before the treatment begins. Good oral care is very important to prevent problems. Fluoride treatments can be used to prevent tooth decay. After the treatment, regular check-ups with the dentist should be organised.
Nutrition problems
Difficulty chewing and swallowing and loss of appetite can lead to malnutrition and weight loss. Steps can be taken to increase appetite and help people eat more and continue to eat well. Nutritional supplements may be recommended. A registered dietitian can often help people manage their nutrition and anorexia.
Decreased thyroid function (hypothyroidism)
Between 30 per cent and 40 per cent of people who receive radiotherapy for head and neck cancers, including oral cancer, will develop hypothyroidism. Some symptoms of hypothyroidism include extreme fatigue, dry skin and hair, hair loss, weight gain and intolerance to cold.
Those with hypothyroidism after oral cancer treatment may need to take daily medication.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS KIDNEY CANCER?
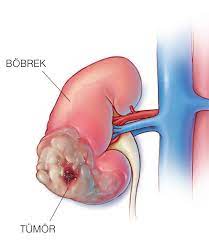
Kidney cancer is a disease in which kidney cells become malignant (cancerous) and grow out of control to form a tumour. In other words, kidney cancer is caused by abnormal growth of cells in the kidneys. Almost all kidney cancers first occur in the lining of the small tubes (tubules) in the kidney. This type of kidney cancer is called renal cell carcinoma.
Renal cell carcinomas (RCCs) account for about 90 per cent of kidney cancer cases. Other types of kidney cancer are:
- Transitional cell carcinoma or renal pelvis cancer, which starts on the lining of the renal pelvis
- Wilms’ tumour (nephroblastoma), the most common cancer in children aged 14 and under
- The rare renal sarcoma develops in the soft tissue of the kidney.
WHAT ARE BENIGN KIDNEY TUMOURS (NON-CANCEROUS LESIONS IN THE KIDNEY)?
Benign kidney tumours can be treated by destroying them using many of the same treatments used for kidney cancers, such as surgery or radiofrequency ablation. The choice of treatment depends on many factors, including the size of the tumour and whether it causes any symptoms, the number of tumours, whether the tumours are in both kidneys and the person’s general health.
Angiomyolipoma
Angiomyolipomas are the most common benign kidney tumour. They are more common in women. They can develop in people with tuberous sclerosis, a genetic condition.
These tumours are made up of different types of connective tissue (blood vessels, smooth muscle and fat). If they do not cause any symptoms, they can usually be monitored closely. If they start to cause problems (such as pain or bleeding…) they may need to be treated.
Oncocytoma
Oncocytomas are benign kidney tumours that are not common and can sometimes grow quite large. They are more common in men and do not spread to other organs.
WHAT ARE THE CAUSES OF KIDNEY CANCER?
Kidney cancers account for about 2.5 per cent of all cancers. Kidney cancer is twice as common in men as in women. The risk of kidney cancer increases with age. As a matter of fact, most cases of kidney cancer occur in people over the age of 50. Although the cause of kidney cancer is not known exactly, the factors listed below may increase the risk of developing kidney cancer.
Smoking: Smokers have almost twice the risk of developing kidney cancer than non-smokers. About 1 in 3 of all types of kidney cancer is thought to be related to smoking
Obesity Obesity can cause changes in certain hormones that can lead to kidney cancer.
High blood pressure: High blood pressure can increase the risk of kidney cancer.
Kidney failure: People with kidney failure have a higher risk of developing kidney cancer.
Family history of cancer: People with a parent, brother or sister (first-degree relative) with kidney cancer are at high risk.
Radiation exposure: The risk of developing kidney cancer may be increased in people who have previously undergone radiation therapy for therapeutic purposes or who have been exposed to radiation for other reasons over a long period of time.
Exposure to toxic substances at work: The risk of developing kidney cancer may be higher after regular exposure to chemicals such as certain metal degreasers, arsenic or cadmium used in mining, farming, welding and painting.
WHAT ARE THE SYMPTOMS OF KIDNEY CANCER?
In its early stages, kidney cancer usually does not cause any obvious or disturbing symptoms. Small-sized tumours in the early stages are usually detected by chance, especially in abdominal ultrasonography or tomography performed for another disease.
As the kidney tumour grows, the symptoms listed below may occur:
- In some cases, blood may appear in the urine. In other cases, traces of blood are detected in a urinalysis, a laboratory test usually performed as part of a regular medical examination
- A lump or mass in the kidney area
- Not very severe, persistent pain, especially in the lumbar region
Less common symptoms of kidney cancer may include
- Fatigue
- Loss of appetite
- Weight loss
- High fever
High blood pressure or an abnormally low red blood cell count (low RBC count) (anaemia) may also indicate a kidney tumour. These symptoms are less common.
On the other hand, if the tumour has spread to organs such as bones and lungs, symptoms such as cough, bloody sputum and bone pain may also be observed.
HOW IS KIDNEY CANCER DIAGNOSED?
Since kidney cancer is usually asymptomatic, i.e. it can be asymptomatic, the tumour is usually detected when the patient undergoes a medical test for another reason. In ultrasound and computed tomography examinations performed in any complaint of the patient, a kidney tumour that the patient is not aware of can be detected while the disease is still in the early stage. For example; when a patient presents to a doctor with a gallbladder complaint and is referred to an ultrasound by an internal medicine specialist, the probability of catching a developing kidney tumour during ultrasound is quite high.
Computed tomography (CT) and MRI scans are often the only tests doctors need to diagnose kidney cancer. Sometimes doctors will also perform what is known as a percutaneous biopsy if they need more information about a tumour before recommending a treatment. During this procedure, the doctor numbs the skin using local anaesthetic. He or she then uses a small needle to pull out some of the tissue.
Doctors may use CT scans or ultrasound (the use of sound waves to create images on a computer monitor) to locate the tumour and guide the insertion and withdrawal of the needle. A pathologist, a doctor who studies diseases in a laboratory, examines tissue samples under a microscope for signs of cancer.
Urine tests do not diagnose kidney cancer; however, the doctor may want to see if there is blood in the urine, which is a common sign of advanced kidney cancer. Blood tests, on the other hand, help doctors determine if the kidneys are working properly, but are not used to diagnose kidney cancer.
WHAT ARE THE STAGES OF KIDNEY CANCER?
Staging is the process of determining how extensive the cancer is and is an important part of diagnosis. Depending on the stage of the cancer, the most appropriate treatment options are determined. The stages of kidney cancer range from Stage I (the least severe stage) to Stage IV. When patients are confirmed to have kidney cancer, the doctor will discuss staging.
Stage I (least severe stage)
The tumour is 7 cm or smaller and is located only in the kidney. It has not spread to lymph nodes or distant organs.
Stage II
The tumour is larger than 7 cm and is located only in the kidney. It has not spread to lymph nodes or distant organs.
Stage III
In stage III, the tumour extends to surrounding tissues outside the kidney and may have spread to regional lymph nodes.
Stage IV
The tumour has spread to areas outside the Gerota fascia, the layer of connective tissue that compresses the kidneys and adrenal glands, and extends to the adrenal gland. The cancer has also spread to numerous lymph nodes or to distant areas of the body, such as the bones, liver or lungs.
WHAT IS THE TREATMENT FOR KIDNEY CANCER?
The options for treating kidney cancer can depend on a number of factors, including the type of kidney cancer the patient has, whether the cancer has spread, and treatment preferences, as well as the patient’s overall health. The standard method of treating kidney cancers is surgery. The aim of the surgical procedure is to remove the cancer, preserving normal kidney function whenever possible. Depending on the stage of the cancer, the size of the mass, the area of the kidney in which the mass is located and its number, the whole kidney or only the mass is removed by closed method. If the cancer has spread beyond the kidney, additional treatments may be recommended.
Removal of the affected kidney (nephrectomy)
A complete (radical) nephrectomy involves removal of the entire kidney, the healthy tissue margin and sometimes additional nearby tissues such as lymph nodes, adrenal gland or other structures.
The surgeon can perform nephrectomy through a single incision in the abdomen or side (open nephrectomy) or through a series of small incisions in the abdomen (laparoscopic or robotic-assisted laparoscopic nephrectomy).
Removal of the tumour from the kidney (partial nephrectomy)
This procedure, also called kidney-sparing or nephron-sparing surgery, is a common treatment for early-stage tumours. Kidney-sparing surgery aims to preserve kidney function as much as possible and reduce the risk of subsequent complications such as kidney disease and the need for dialysis.
Non-surgical treatments such as chemotherapy and radiation therapy have low effectiveness in the treatment of kidney cancer.
Immunotherapy works to strengthen your body’s own immune system. Immunotherapy is a treatment option for people with advanced kidney cancer. Cytokines (proteins that activate the immune system) can be given intravenously or orally and can shrink the cancer. Targeted therapies can also be used for advanced kidney cancers. Targeted therapies target specific molecules. Targeted therapy medicines are usually given as tablets or intravenously. Tyrosine kinase inhibitors (TKIs) have been tested in people with advanced kidney cancer and have been found to cause fewer side effects than chemotherapy drugs.
Note: Da Vinci Robotic Surgery provides great advantages to the patient in kidney tumour surgeries. In cases such as partial removal of the kidney or removal of the tumoured part of the kidney, the problem is solved by entering 4-5 holes from the abdomen, separating the tumoured tissue, without the need for large surgical incisions, without compromising oncological and surgical principles.
FREQUENTLY ASKED QUESTIONS ABOUT KIDNEY CANCER
What is embolisation for the treatment of kidney cancer?
The surgeon inserts a catheter and passes a synthetic material into the blood vessel. This material blocks the blood supply to the kidney, which deprives the tumour of oxygen and nutrients and causes it to shrink.
Can kidney cancer be prevented?
One hundred per cent prevention of the disease is not possible as the causes of kidney cancer are not fully known; however, maintaining a healthy lifestyle, a combination of a healthy diet and regular exercise will help prevent obesity, which is a major risk factor for kidney cancer.
Is kidney cancer fatal?
The prognosis for kidney cancer varies depending on the stage of the cancer. Although the average life expectancy of kidney cancer cases is determined according to the stages of cancer, this situation may differ from person to person.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS TONGUE CANCER?

Tongue cancer is a serious life-threatening type of oral cavity cancer. The tongue is the most common site of oral cavity cancers after the lips.
WHAT ARE THE SYMPTOMS OF TONGUE CANCER?
The symptoms of tongue cancer are similar to those of other types of oral cancers. Depending on the stage of development, the most common symptom of tongue cancer is a non-healing sore in the oral cavity. Some symptoms of oral cancer or tongue cancer can also be attributed to other medical conditions, so if the relevant symptoms persist for more than two weeks, it is necessary to have a thorough clinical examination, undergo laboratory tests and consult a doctor for a definitive conclusion.
The symptoms of tongue cancer are usually painless and not specific to the disease. Due to the non-specific and often painless symptoms, tongue cancer and other types of oral cancer are often not detected at an early stage. Symptoms of tongue cancer, which is more likely to be seen and felt than hypopharyngeal tongue cancer (oral tongue cancer), include
- A greyish-pinkish mass or sore on the lateral surfaces of the tongue
- Tongue pain
- Sore throat
- Difficulty swallowing or chewing
- Difficulty moving the tongue
Cancer in the root of the tongue is usually diagnosed at an advanced stage, when the tumour is larger and the cancer has spread to the lymph nodes in the neck.
Some of the symptoms caused by cancer in the root of the tongue are as follows:
- Sore throat
- Difficulty swallowing
- Feeling as if there is a lump in the throat
- Changes in voice
- Ear pain
It is important that people who complain of any of these symptoms are evaluated by an ear, nose and throat specialist. Because, as with most types of cancer, early diagnosis is very important for the success of tongue cancer treatment.
WHAT ARE THE RISK FACTORS FOR TONGUE CANCER?
The two most important risk factors for the development of tongue cancer are tobacco use and alcohol consumption. Men are twice as likely as women to develop tongue cancer. While tongue cancer is rarely seen in young people, it is more likely to occur in people aged 40 and over.
Risk factors for tongue cancer are summarised as follows:
- Smoking or using other forms of tobacco (chewing, etc.)
- Alcohol consumption
- HPV-16 and 18: Human Papillomavirus
- Asbestos exposure
- Factors related to malnutrition
- Genetic predisposition
- Poor oral hygiene and long-term irritation
HOW IS TONGUE CANCER DIAGNOSED?
A biopsy is the first step in the diagnosis of tongue cancer. During a biopsy, a small amount of tissue is removed from the part of the tongue where cancer is suspected. The tissue is sent to a pathologist who examines it under a microscope and helps to make a diagnosis. The examination of a tissue sample from the suspected cancer site by a pathologist is key to the diagnosis. After the diagnosis of tongue cancers, radiological examinations such as ultrasound, computed tomography and MRI are used to evaluate the size, stage, spread and relationship with other organs. In this way, the treatment method to be applied is decided.
The stage of cancer at the time of diagnosis determines the treatment options and has a strong influence on survival time. The earlier tongue cancer is diagnosed, the higher the chance of survival five years after diagnosis.
WHAT ARE THE TYPES OF TONGUE CANCER?
The most common type of tongue cancer is squamous cell carcinoma (SCC). Squamous cells are flat, skin-like cells that line the inside of the mouth, nose, larynx, thyroid and throat. Squamous cell carcinoma is the name for cancer that starts in these cells.
WHAT ARE THE STAGES OF TONGUE CANCER?
The stage of the cancer indicates how big the tumour is and whether it has spread. The classification indicating the stage of cancer in the body is the TNM classification. According to this classification
T; the size of the tumour at the site of origin,
N; for tumours in the head and neck region, the size and condition of the tumour that has metastasised (spread) to the neck lymph nodes,
M indicates the presence of metastases beyond the neck, in distant organs, often via blood.
In summary, the stage of the cancer depends on the following factors
- How much the cancer has grown in local tissues
- Whether it has spread to nearby lymph nodes
- Whether it has spread to another part of the body
WHAT ARE THE TREATMENT METHODS FOR TONGUE CANCER?
Treatment options for tongue cancer vary depending on the general health status of the patient, the type and stage of the tumour. Early diagnosis is very important for survival and comfort of life in tongue cancers.
Surgical procedure
For small tongue cancers, surgical removal of the tumour is usually the only treatment required. However, depending on the stage of the tumour and the results of radiological examination, neck dissection and surgical removal of the affected or potentially affected neck lymph nodes may be required.
Radiotherapy
Radiotherapy is often used in combination with chemotherapy or before/after surgery to stop cancer cells from multiplying.
Intensity Modulated Radiation Therapy (IMRT) uses an advanced computer system to calculate the correct dose of radiation needed to treat the tumour. This minimises excessive radiation exposure to the normal tissue surrounding the tumour, limiting the amount of side effects that may occur due to radiotherapy and ensuring the most effective radiotherapy.
Chemotherapy
Chemotherapy is used in combination with other treatment options such as surgery and/or radiation. The aim of chemotherapy is to help control the growth of the cancerous tumour. When combined with radiation, it is called chemoradiation. It is also called palliative treatment when given alone to control the symptoms of the disease.
Chemotherapy may also be given after surgery to reduce the risk of the cancer coming back.
After the surgical procedure, radiotherapy and chemotherapy, diet and speech, swallowing, physical and occupational rehabilitation therapies can be applied to improve the quality of life of tongue cancer patients.
WHAT CAN BE DONE TO PREVENT TONGUE CANCER?
Although there is no proven method to prevent tongue cancer, the risk of developing tongue cancer can be reduced by considering the following recommendations.
- Do not smoke or use tobacco products. Smokers and/or users of tobacco products should seek professional help if necessary to quit these habits.
- Alcohol consumption should be avoided
- It is necessary to see a doctor regularly for check-ups and cancer screening examinations.
- Pay attention to oral hygiene
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS LIVER CANCER?

Malignant tumours originating from the liver’s own cells are called primary liver cancer. Since it originates from the liver’s own cells, it is called hepatocellular (liver cell) carcinoma. It is one of the most common and life-threatening tumour types. In addition, there are liver tumours that do not originate from hepatocytes. These are cholangiocellular carcinoma (tumours originating from the biliary tract). However, there are angiosarcoma, that is, liver tumours originating from vascular structures. If the person’s liver is healthy, the risk of developing this type of cancer is very low. Especially those with liver disease, individuals with structural disorders of the liver (cirrhosis or cirrhosis grounds) are at risk of liver cancer. Liver cancer is one of the most common cancers in the world. It is a type of disease that should be diagnosed early because it causes life risk. Early diagnosis of this disease is very important. The main treatment is the removal of cancerous tissue. It is very difficult to remove only the tumoured part of the liver because the liver is sick and it is only sufficient for the person in terms of function. Liver transplantation stands out as an important treatment method for liver cancer patients.
WHAT ARE THE SYMPTOMS OF LIVER CANCER?
Liver cancer does not have a very specific finding in the early period. Therefore, when the diagnosis is made, the cancer is usually found to have reached a large size. Findings such as weight loss, loss of appetite, weakness, fatigue, jaundice, fluid collection in the abdomen are frequently observed. Sometimes there may be a feeling of pain and fullness in the upper right side of the abdomen. Since cancer is often preceded by a chronic liver disease (e.g. cirrhosis) and these diseases often have similar symptoms, the case may be confused. Although liver cancers are the 6th most common type of cancer in the world, they are more common in our country because of the high number of cirrhosis-related diseases. For this reason, patients with chronic hepatitis and early stage cirrhosis should be followed up radiologically in 6 months-1 year periods against the risk of tumour development with methods such as ultrasound and, if necessary, MRI and CT.
WHAT CAUSES LIVER CANCER?
Liver causes can be listed as follows:
- Hepatitis B virus infections,
- Hepatitis C and
- Hepatitis D virus infections,
- Aflatoxin (poison of aspergillus flavus),
- Cirrhosis,
- Genetic congenital metabolic diseases,
- Haemochromatosis,
- Wilson’s disease,
- Glycogen storage disease,
- Chemicals (nitrites, hydrocarbons, solvents) are among the causes of liver cancer.
The liver, which is the body’s factory, is a centre affecting all systems, a blood reservoir and a part of the defence system. The group with the highest risk for liver cancer is people with hepatitis. Since liver cancer does not give symptoms in the early period, the possibility of early diagnosis is low. 80 per cent of these cancers develop mostly in people with cirrhosis, so patients should be closely monitored. Compared to individuals who are not at risk, people with hepatitis B and C are 200 times more likely to develop liver cancer. Hepatitis B can be prevented by vaccination. Treatments developed for hepatitis C also give very positive results. Cirrhosis is a disease caused by damage to liver cells due to alcohol, hepatitis, immune system-related causes, etc. There is a risk of developing liver cancer in 5% of cirrhosis patients. Obesity is also among the important risks as it can trigger fatty liver and cirrhosis.
HOW IS LIVER CANCER DIAGNOSED?
In some cases, liver cancer may not give any symptoms until it reaches an advanced stage. As the cancer progresses, symptoms such as causeless weight loss, constant swelling of the abdomen, fluid accumulation, loss of appetite and constant weakness, jaundice may begin to appear. People with such complaints should consult a doctor as soon as possible. Today, it is possible to detect any kind of development in the liver by means of imaging methods. Especially patients at risk should be followed up with ultrasonography, which is the cheapest and most easily applicable method. Computed tomography (CT), magnetic resonance imaging (MRI) and angiography are other methods to be used. Sometimes several of these imaging methods can be used together to strengthen the diagnosis. Alpha feto protein (AFP), a tumour marker, can be detected in the blood. A high level of this test is significant in terms of cancer. However, it should not be forgotten that it can be normal even in patients with known cancer. A normal result does not mean that there is no tumour. In some cases, a needle biopsy of the liver may be performed for diagnosis. However, this is not a method that should be used frequently. Whether or not a biopsy should be performed should be decided by physicians experienced in these matters, i.e. gastroenterology specialists and/or surgeons who are interested in liver disease.
HOW IS LIVER CANCER TREATED?
The consequences of untreated liver cancer cause unfavourable pictures. The life expectancy in these cases is 6-9 months. The most effective method is surgical removal of the tumour. The ability to perform surgical treatment depends on the stage of the tumour and whether it has spread to the surrounding area or not, and if the patient has a liver disease, the degree of this disease. Surgery has no place in liver cancer that has spread outside the liver. The success of surgery is also related to the diameter of the tumour. Survival after surgery is much better in patients with a diameter <5cm compared to patients with a tumour >5cm. The expected 5-year survival after surgical removal under ideal conditions (<5cm, single, no invasion) is around 60%. In cases where surgery cannot be performed, methods such as radioembolisation, chemoembolisation, chemotherapy, alcohol injection, radiofrequency ablation can be applied by the Interventional Radiology Specialist. In appropriate cases, these can also be used together with surgery. What should be taken into consideration in surgery is that the remaining liver should be of sufficient quality and size to sustain the patient’s life in a healthy way. If surgical removal of the tumour in the liver is not appropriate, liver transplantation can be used. There are many reasons that lead to liver transplantation. Liver tumours are one of them. If the tumour meets the appropriate criteria, liver transplantation is the ideal treatment in terms of outcome. With liver transplantation, the diseased liver, which is potentially at risk of developing a tumour, is completely removed. A healthy liver is transplanted in its place. Patients who undergo transplantation have a lower risk of tumour regrowth.
FREQUENTLY ASKED QUESTIONS ABOUT LIVER CANCER
What are the first symptoms of liver cancer?
Liver cancer does not have a very specific finding in the early period. Therefore, when the diagnosis is made, the cancer is usually found to have reached a large size. Findings such as weight loss, loss of appetite, weakness, fatigue, jaundice, fluid collection in the abdomen are frequently observed.
Does liver cancer go away?
Untreated liver cancer causes unfavourable outcomes. The life expectancy in these cases is 6-9 months. The most effective method is surgical removal of the tumour. The ability to perform surgical treatment depends on the stage of the tumour and whether it has spread to the surrounding area, and if the patient has liver disease, the degree of this disease. Surgery has no place in liver cancer that has spread outside the liver. The success of surgery is also related to the diameter of the tumour. Survival after surgery is much better in patients with a diameter <5cm compared to patients with a tumour >5cm. The expected 5-year survival after surgical removal under ideal conditions (<5cm, single, no invasion) is around 60%. In cases where surgery cannot be performed, methods such as radioembolisation, chemoembolisation, chemotherapy, alcohol injection, radiofrequency ablation can be applied by the Interventional Radiology Specialist. In appropriate cases, these can also be used together with surgery. What should be taken into consideration in surgery is that the remaining liver should be of sufficient quality and size to sustain the patient’s life in a healthy way. If surgical removal of the tumour in the liver is not appropriate, liver transplantation can be used. There are many reasons that lead to liver transplantation. Liver tumours are one of them. If the tumour meets the appropriate criteria, liver transplantation is the most ideal treatment in terms of results. With liver transplantation, the diseased liver, which is potentially at risk of developing a tumour, is completely removed. A healthy liver is transplanted in its place. Patients who undergo transplantation have a lower risk of tumour recurrence.
How is liver cancer recognised?
Liver cancer does not have any specific findings in the early stages. Therefore, when the diagnosis is made, the cancer is usually found to have reached a large size. Findings such as weight loss, loss of appetite, weakness, fatigue, jaundice, fluid collection in the abdomen are frequently observed. Sometimes there may be a feeling of pain and fullness in the upper right side of the abdomen. Since a chronic liver disease (e.g. cirrhosis) is often present in the background of the cancer and these diseases often give similar symptoms, the case can be confused. Although liver cancers are the 6th most common type of cancer in the world, they are more common in our country because of the high number of cirrhosis-related diseases. For this reason, patients with chronic hepatitis and early stage cirrhosis should be followed up radiologically with methods such as ultrasound and, if necessary, MRI and CT at 6-month-1-year intervals against the risk of tumour development.
Where does liver cancer cause pain?
Findings such as weight loss, loss of appetite, weakness, fatigue, jaundice, fluid collection in the abdomen are frequently observed. Sometimes there may be a feeling of fullness in the upper right side of the abdomen.
Who can get liver cancer?
Liver tumours that develop in patients with hepatitis B and hepatitis C or cirrhosis may not show symptoms in the early period. Hepatitis B and hepatitis C are among the most common diseases in our country. The presence of hepatitis virus is also an important risk factor for the development of liver cancer.
At what age is liver cancer diagnosed?
The average age at diagnosis of liver cancer is 62 years. More than 90% of patients diagnosed with liver cancer are over the age of 45, while 3% are between the ages of 35-44 and less than 3% are younger than 35.
How many stages of liver cancer?
Liver cancer should first be staged for treatment planning. Liver cancers are generally divided into 4 stages:
Stage 1: In liver cancer, the tumour tissue is located in the liver and has not affected any other organ or structure.
Stage 2: In liver cancer, small tumoural formations are located within the liver tissue or a malignant tumour tissue is found to have reached the blood vessels.
Stage 3: In liver cancer, several large tumours have invaded the liver tissue or one large tumour has invaded a large blood vessel.
Stage 4: In liver cancer, liver cancer has now metastasised and spread to other parts of the body.
What is good for liver cancer?
The question is frequently asked by users. There is no place for support products or any food / beverage in the treatment of liver cancer. Any product that is said to be beneficial should never be used without asking a doctor.
What does a mass in the liver indicate?
A mass in the liver is also called a tumour. These masses are generally benign or malignant tumours arising from the organ’s own tissue. On the other hand, benign masses that spread to the liver as a result of a different disease can also be seen.
Is a mass in the liver dangerous?
Most of the liver masses are benign tumours. Although the majority of malignant tumours are metastases that spread to the liver from other organs, masses formed in the liver’s own tissue are also frequently seen.
Does a mass in the liver cause pain?
Liver cancer may not show any symptoms in the early period. As the diameter of the mass increases, a diffuse pain appears on the right side of the abdomen. In advanced stages, severe abdominal pain is accompanied by weight loss and abdominal swelling.
What is a benign mass in the liver?
The most common benign tumours of the liver are haemangiomas, adenomas and focal nodular hyperplasia. Haemangiomas are the most common benign tumours of the liver. They have no risk of carcinogenesis and have a low risk of rupturing and bleeding. For this reason, patients are usually followed up with serial imaging examinations.
How is the treatment of a mass in the liver?
The most effective method is surgical removal of the tumour. Surgical treatment depends on the stage of the tumour, whether it has spread to the surrounding area or not, and the degree of liver disease in the patient. Surgery has no place in a liver cancer that has spread outside the liver. The success of surgery is also related to the diameter of the tumour. If surgical removal of the tumour in the liver is not appropriate, liver transplantation can be used. There are many reasons for liver transplantation. Liver tumours are one of them.
How is it understood that the liver cyst is benign?
Liver cysts usually do not cause complaints and most of them are benign. Cysts that do not show symptoms are mostly small cysts. However, as the cyst grows, some complaints may occur in the abdomen.
How many cm of liver cyst is dangerous?
Survival after surgery is much better in patients with a diameter <5cm compared to those with a tumour >5cm. The expected 5-year survival after surgical removal under ideal conditions (<5cm, single, no invasion) is around 60%.
How long does liver mass surgery take?
Although it varies depending on the size of the mass and whether there is metastasis or not, it takes approximately 1-2 hours.
How is liver cancer prevented?
To prevent liver cancer, it is necessary to be protected from hepatitis viruses. Vaccination against hepatitis B virus should be provided before it is too late. Excessive alcohol consumption should also be avoided as it can cause cirrhosis and liver cancer in the long term. By reducing the risk of obesity and diabetes with a healthy diet, the risk of fatty liver disease, cirrhosis and liver cancer will also be reduced.
What is the importance of interventional radiological applications in liver cancer treatments?
The types of interventional radiological applications in cancer treatment and their effectiveness have been gradually increasing with the developing technology in recent years. The most important of these treatments are radiofrequency (RF) and microwave (MW) ablation treatments, which can be defined as burning the tumour with a needle inserted into the tumour under the guidance of imaging through the skin, chemoembolisation and radioembolisation (Yitrium 90-Y-90) treatments in which high doses of chemotherapeutic or radioactive isotope-loaded drugs are administered to reach the tumour through blood vessels with angiographic techniques and both block the vessels to cut the tumour’s nutrition and destroy it at the same time. These methods, which can provide complete treatment in early stage small tumours, can be used to slow or stop the spread of the tumour or to shrink the tumour in patients in advanced stages where other treatments cannot be applied.
How does the Yitrium 90 treatment for liver cancer differ from others?
This treatment method, also known as radioembolisation or selective internal radiotherapy (SIRT), is based on the principle of reaching a tumour in the liver through the arteries and injecting Yttrium 90 radioisotope loaded into microspheres to deliver a dose of radiation that is too high to be delivered externally, thereby eliminating the viability of the tumour. Yttrium 90 treatment is applied in two steps. In the first step, the patient’s hepatic arteries are determined in detail, and if there are any vessels connected with the gastrointestinal system, these are blocked. Then, a test drug that mimics the actual Y90 radioactive drug is administered into the liver and a preparatory angiography is completed to test the actual treatment. The patient does not need to be hospitalised for the preparatory angiography. If it is found that the liver vasculature is suitable for this treatment, the appropriate treatment dose is calculated by the nuclear medicine doctor and the actual treatment day is determined. Generally, approximately 7-10 days after the preparatory angiography, the treatment is administered into the liver by angiography in the second step procedure.
Who is suitable for Yttrium-90 treatment of liver cancer?
The patient group suitable for treatment consists of patients whose existing tumoural disease is limited to the liver and who do not have a significant tumour focus outside the liver. In addition, the patient’s suitability for treatment is also assessed during the preparatory angiography.
Is it possible to treat liver metastases?
The treatment of liver metastases depends on the location of the spread (cancer of which organ), the extent of the spread (how many metastases are in the liver), the location of the metastases in the liver and whether there is spread elsewhere than the liver. Lymphomas in particular can be treated with certain combinations of chemotherapy. Breast and lung cancers benefit partly from chemotherapy. The treatment of liver metastases must be differentiated from the treatment of metastases from large bowel (colorectal) cancer.
Colorectal cancers often metastasise to the liver and surgical removal of metastases in the liver is very important for treatment.
What is liver metastasis?
The spread of cancer in any part of the body from its origin (organ) to another place is called metastasis of that cancer. The appearance of these metastases in the liver is known as liver metastasis.
Is metastasis in the liver a common condition?
Yes, it is. The liver is a large organ that filters the blood.
Therefore, cancer cells that enter the bloodstream remain stuck in this organ and continue to grow. Liver metastases from cancers of the digestive system (intestines) are particularly common because the blood from these organs first passes through the liver. Cancers of organs such as the large intestine, stomach, pancreas, biliary tract and small intestine often metastasise to the liver.
Metastases from breast cancer, lung cancer and lymphomas are also common.
What is the life expectancy of metastatic liver cancer?
This period varies from patient to patient, depending on the type of treatment and many parameters.
Is liver cancer a problem that can be solved with herbal treatment?
Herbal solutions have no place in the treatment of liver cancer. Herbal treatment should never be used without asking a doctor.
What are the risk factors for the development of liver cancer?
- Hepatitis B virus infections
- Hepatitis C virus infections
- Hepatitis D virus infections
- Aflatoxin (aspergillus flavus poison)
- Cirrhosis
- Genetic, congenital, metabolic diseases
- Haemachromatosis, Wilson, Glycogen storage disease
- Chemicals; Nitrites, hydrocarbons, solvents
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS COLON CANCER?

Colon cancer, a disease that develops in the last part of the digestive system, commonly known as the “large intestine”, is seen in 1 out of every 20 people during their lifetime.
The colon and rectum are parts of the digestive system. The large intestine is the organ that comes after the small intestine and is approximately 1.5 m long. It starts with the blind intestine in the lower right side of the abdomen in the shape of an inverted letter U, goes up and crosses the abdomen horizontally by turning under the liver. It comes under the spleen, which is located in the upper left corner, and again makes a turn downwards from the left side and joins with the rectum. The rectum is the last part of the digestive system, which is approximately 15 cm long and formed as a result of the expansion of the large intestine.
Colon cancer starts in the cells in the colon. As the number of cells increases, it spreads circularly around the colon like a napkin ring. In case of early diagnosis, cancer cells can be detected only in the colon. In the absence of early diagnosis, the cancer may spread to nearby organs, lymph nodes and through the bloodstream to the liver, lung and other organs.
The most important criterion for success in colon cancer treatment is early diagnosis. When colon or large intestine cancer is detected at an early stage, it is possible to completely get rid of the disease.
RISK FACTORS FOR COLON CANCER
In developed countries, the rate of colon and rectal cancer is 4 to 10 times higher than in developing countries. The causes of colorectal cancer can be listed as lifestyle, changes in environmental factors and inherited genetic factors.
Genetic Factors
People with a family history of colorectal cancer have an increased risk of cancer. Inherited genetic factors increase the risk. Both familial adenomatous polyps in the large intestine and hereditary non-polyp colorectal cancer, also known as Lynch syndrome, increase the risk of colon cancer. Although genetic colorectal cancers account for only 5-10% of the disease, people with these genetic factors have a younger age of onset and a higher risk of survival than other colon cancer patients.
Hereditary non-polyp colorectal cancer (Lynch syndrome) is the most common of the genetic colorectal cancers. It is caused by inherited gene mutation as a result of incompatible DNA matches. The average age of diagnosis is 45 years. This type of gene mutation predisposes to cancer of the endometrium (inner lining of the womb), ovary, small intestine, ureter (urinary tract) and renal pelvis (kidney basin).
The presence of a history of cancer in the family and first-degree relatives has a significant effect on the occurrence of the disease.
People with a family history of colon cancer should start having a colonoscopy 10 years before the age at which colon cancer was detected in their relatives. Completely healthy people who do not have a family history of colon cancer or who do not have any complaints should have a colonoscopy at least once from the age of 50. You can easily make an online hospital appointment to see specialised doctors.
WHAT CAUSES COLON CANCER?
Polyps as well as excessive fatty, red meat-based diet, obesity, smoking and alcohol consumption are effective in the formation of colon cancer. When polyps are seen in the large intestine during screening colonoscopies, it is possible to prevent the disease by removing them before they become cancerous. A history of breast and ovarian cancer in women also increases the risk of colon cancer in these individuals. It is recommended that people with breast and ovarian cancer should be screened for colon cancer before the age of 50.
Polyps usually start to give symptoms in the late period, that is, when they turn into cancer. Only a small proportion of polyps turn into cancer. However, since the majority of cancers develop from polyps, it is an issue that requires great attention. When we look at the general population, this rate is around 10-15 per cent. Around the age of 50, approximately 25% of the population has different types of polyps. At the age of 70, the incidence is close to 50%; in other words, the incidence of polyps increases with age.
Characteristics of polyps;
- It does not pass on its own.
- They have genetic characteristics. Patients with colon cancer in first degree relatives and polyps detected in previous examinations constitute the risk group and close follow-up is required.
- Polyps are usually around 1 cm. Polyps larger than 2 cm can be dangerous and should be removed.
- Symptoms such as severe pain, intestinal obstruction, weight loss are usually late symptoms. Problems such as haemorrhoids and fissures in the anus may cause delays in the diagnosis and treatment of rectal cancer in some patients because they have similar symptoms. These symptoms may mislead both patients and rarely physicians. In general, the possibility of rectal and large intestine cancer should be investigated well in bleeding from the rectal area at the age of 40 and above.
- It is not yet possible to prevent polyp formation. People who adopt a sedentary lifestyle, people with excessive stress, smokers and alcohol users, obesity patients and those who are predominantly fed with red meat are at risk. However, eating foods with pulp, not smoking, that is, everything that regulates bowel movements is an important factor in preventing the formation of polyps.
Other Colon (Large Bowel Cancer) Risk Factors
Age: Although it can occur at any age, it is most common in people over 50. The risk of colon cancer increases with age. Patients over 60 are 10 times more likely to develop colon and rectal cancers than people under 40.
Intestinal Inflammations: There are mainly two types of intestinal inflammation. The first is ulcerative colitis, which is ulceration of the colon mucosa due to infection. The second is Crohn’s disease, which occurs with intermittent inflammation in any part of the digestive system from the mouth to the anus or in several different parts at the same time. Although it is a long-lasting, chronic disease, it is treatable. Due to the high risk of cancer, colorectal cancer screening tests should be performed more frequently.
Nutrition: The incidence of colon and rectal cancers is quite high, especially in the USA and European countries where fast food consumption is common. Consumption of food without pulp increases constipation and causes the feces to remain in the intestine for a long time and causes cancer in that area. Deli products, pickled foods, smoked meats, barbecue foods and fried foods are foods that cause constipation. In addition, consuming foods rich in fruits, vegetables, legumes, chicken and cereals has been found to reduce the risk.
Obesity: Regardless of whether it is a man or a woman, being overweight increases the risk of colon cancer.
Smoking: Many studies have shown a relationship between smoking and colon cancer.
WHAT ARE THE SYMPTOMS OF COLON CANCER?
The question “What are the symptoms of colon cancer?” can be answered as follows. The most common colon cancer symptoms:
- Continuous diarrhoea and constipation,
- Bleeding in the anus and feces
- White stain in the stool
In cases where colon (large intestine) cancer progresses and obstructs the intestine, abdominal swelling and pain occur. It is important for those with such complaints to consult a doctor for early diagnosis.
- Feeling that the intestines cannot empty sufficiently,
- Difficulty in defecation
- Painful defecation
- Unexplained weight loss
- Vomiting
Symptoms are among the most important symptoms of colon cancer, also known as colon cancer. Colon cancer involving the right side of the intestine and colon cancer involving the left side may give different symptoms. Since the left side of the intestine is a narrower region, complaints such as thinning in the stool, bleeding, change in stool pattern are more common in cancers of this region, while on the right side, since the intestine is wider, the cancer progresses insidiously here and takes longer to give symptoms.
The patient has symptoms such as weakness, anaemia, loss of appetite and abdominal pain. Painful defecation, iron deficiency anaemia, feeling of a mass in the abdomen are important symptoms of colon cancer. Diagnosing colon cancer before the disease progresses greatly increases the chance of life. Therefore, it is very important to follow the symptoms of colon cancer for early diagnosis.
HOW IS COLON CANCER DIAGNOSED?
Colon cancer is a type of cancer that is included in screening programmes. The most effective way to prevent cancer or to detect the disease at an early stage is regular endoscopic examinations. The most important of these is colonoscopy. Colonoscopy is a procedure that can both detect an existing tumour at an early stage and detect polyps and similar problems that can lead to cancer before they become cancerous and protect the person from cancer development. Every individual over 50 years of age is recommended to undergo colonoscopic examination at intervals of 2-5 years according to their risk status, personal health history and family history. Preparation and application of colonoscopy has become much easier and more comfortable for the patient today. New colonoscopes are extremely easy to apply and the desired results are obtained without causing discomfort to the patient.
Colon cancer is diagnosed with some tests under the leadership of specialist physicians. After the patient’s application to the doctor and physical examination, the following tests are performed respectively;
- Examination of occult blood in faeces: It is an extremely simple test, a small amount of faecal samples are examined in the laboratory.
- Radiological examinations: Double contrast colon radiography and computed tomography are performed.
- Laboratory tests: Complete blood count and biochemical tests are performed. Among these, CEA (carcinoembryonic antigen) is one of the tests that can be elevated in the blood in large intestine cancers and helps the diagnosis.
- Endoscopic examinations for definitive diagnosis: Rectoscopy, sigmoidoscopy, colonoscopy and biopsy are performed. A piece of the lesion is taken and examined by a pathologist.
If a person has a family history of colon cancer before the age of 50, he/she should have a colonoscopy from the age of 40. It is very important to repeat the colonoscopy once every 5 years. In addition, it is very important to look for occult blood in the stool once a year for the detection and early diagnosis of cancer. If a person has no family history of colon cancer, it is appropriate to have a colonoscopy regularly every 5 years from the age of 50.
Classical colonoscopy enables the diagnosis of the presence of polyps or cancer, and if the patient has polyps, it has the ability to treat them and prevent the formation of cancer. Once in 5 years, it should not be difficult for the patient. Because colonoscopy is now a procedure that is performed by relaxing the patient with an intravenous needle and made more tolerable with sedation and painkillers.
WHAT ARE THE TREATMENT METHODS FOR COLON CANCER?
In colon cancer, surgery may not be required when the cancer is caught at an early stage on the polyps taken in colonoscopy. It is only followed up closely. Colonoscopy is of great importance in the diagnosis of polyps at an early stage before they turn into cancer. Recent studies have shown that colon cancer can be prevented to a great extent by colonoscopy and removal of polyps at an early stage. For this reason, every man after the age of 45 and every woman after the age of 50 should undergo faecal occult blood screening and colonoscopy. Patient comfort is of great importance during colonoscopy. For this reason, the patient is made semi-conscious with a mild intravenous painkiller called “conscious sedation”. Beforehand, the intestine must be completely emptied by various methods. Then a fibreoptic camera is inserted into the intestine and all polyps are removed. However, the experience of the physician performing the colonoscopy, the disinfection of the device used and the high image quality are of great importance here.
The standard treatment option for advanced colon cancer is surgery, i.e. removal of the tumourous area together with some surrounding healthy tissue and lymph nodes.
Studies show that surgeries performed in accordance with the principles of oncology and by experienced surgeons are the most important factor for the patient’s future. In colon cancer, additional, preventive chemotherapy is administered after surgery, depending on the stage of the disease. For example, in “stage III” cases where the tumour has spread to the lymph nodes adjacent to the intestine, “adjuvant” chemotherapy (preventing the spread of the disease) is now a standard practice all over the world.
In colon cancers, in tumours very close to the anus, it may sometimes be inevitable to cancel the anus and switch to defecation through the abdomen (with colostomy bags). However, in recent years, preoperative radiotherapy and chemotherapy can significantly preserve the anus. In patients who have spread to other organs (metastatic), all three treatment methods (surgery, chemotherapy, radiotherapy) are applied depending on the general condition of the patient, age and the extent of the disease. The aim is to increase the duration and quality of life of patients.
Thanks to the new targeted biological drug therapies found in the last few years, success rates in treatment are increasing day by day.
Diet and screening tests are of great importance in the prevention of colon cancer. It is important to consume plenty of fibrous foods such as vegetables, fruits and cereals, and to get enough calcium and vitamin D. As a secondary prevention measure, screening tests and early diagnosis are of particular importance. For this, screening tests are recommended for both sexes starting from the age of 50. In individuals with a family history of colon cancer, screening tests should be started at an earlier age.
THINGS TO BE CONSIDERED TO PREVENT COLON CANCER
Although it is not yet possible to prevent colon cancer, the risk of colon cancer can be reduced by paying attention to harmful habits such as inappropriate nutrition, sedentary life, obesity, smoking and alcohol. Some life changes should be made for this. These are
- Nutrition: Eating foods rich in fruits, vegetables and legumes is beneficial in reducing the risk of colon cancer. Red meat and alcohol consumption should be moderate as it increases the risk of colon cancer. Healthy eating and consuming foods low in fat will help to keep the weight at a certain rate.
- Exercise: Studies have shown that regular exercise reduces the risk of colon and rectal cancer, as well as many types of cancer. It is necessary to consult a doctor before starting an exercise programme. The doctor will help you with a suitable exercise programme. Exercise for 30 minutes 5 days or more than 5 days a week is recommended. Exercise for 45 minutes to 1 hour may provide more benefit. Moderate activities include brisk walking, cycling on flat terrain… Vigorous activities include climbing and running.
- Non-steroidal anti-inflammatory drugs (such as aspirin): As a result of research, the colon suggests that this type of medication reduces the risk of cancer. They have potential benefits if used regularly. However, when there is a potential risk of colon cancer, it is in your best interest to use them under the supervision of a doctor. Otherwise, it may cause harm with the risk of stomach bleeding.
- Calcium: It may be of little benefit for colon cancer. It is known that 1200 mg calcium consumed daily reduces the colorectal adenoma form by 20% and the advanced adenoma form by 45%. Furthermore, it has been determined that vitamin D and calcium consumed together reduce the form of adenoma.
- Vitamin D; It is a fat-soluble vitamin and is found in dietary products such as fortified milk, cereals, mackerel, salmon, tuna and certain types of fish, and in sunlight. Vitamin D is hypothesised to play an important role in preventing some types of cancer, including colon cancer.
- Precancerous (polyps that can lead to cancer) Polyp Screening and Treatment: Screening tests applied in cancer types, especially in breast cancer, do not prevent the development of cancer, but increase the success rate in treatment by helping to diagnose at an early stage. The development of cancer can be prevented by screening tests applied in the detection of precancerous polyps. Removal of detected polyps can prevent cancer that will develop later.
- Preventive Surgical Intervention: Preventive surgery may be recommended for people at high risk of colorectal cancer. In this surgery, the colon and sometimes the rectum and other related organs are removed before cancer develops. However, this type of surgery may only be available for patients at high risk of colon and rectal cancer. It is important to discuss the benefits and consequences with your doctor before deciding on surgery.
FREQUENTLY ASKED QUESTIONS ABOUT COLON CANCER
What are the stages of colon cancer?
Colon cancer consists of four stages. In the first stage, the cancer has spread to the bowel wall. In stage 2, cancer has spread to all layers of the intestine. In stage 3, cancer spreads to the lymph nodes. In stage 4, it spreads to places such as the liver, peritoneum and lungs.
At what ages is colon cancer seen?
Colon cancer, which can be seen at any stage of life, is often seen in advanced ages. Genetic predisposition, inactivity, overweight, overweight, alcohol, tobacco use and excessive consumption of processed meat are the main risks in colon cancer, where the advanced age factor is basically important.
What is the most important symptom of colon cancer?
In colon cancer, bleeding from the 15 cm part of the large intestine close to the anus is among the most important symptoms. However, colon cancers originating from the initial part of the large intestine close to the small intestine cause blood loss with occult bleeding rather than rectal bleeding and manifests itself with anaemia.
How does colon cancer bleeding occur?
Bleeding from the anus, which is among the symptoms of colon cancer, can be fresh, bright red.
Is colon cancer completely cured?
In many types of cancer, the disease may spread and spread to different organs. Generally, colon cancer can metastasise to the liver. Chemotherapy can be applied after surgery to prevent this situation.
Can colon cancer be cured by surgery?
The most important factor for the future of the patient is the surgeries performed in accordance with the principles of oncology and performed by experienced surgeons.
Does colon cancer recur after surgery?
In colon cancer, chemotherapy is applied after surgery to prevent recurrence depending on the stage of the disease.
What is the risk of death from colon cancer?
Colon cancer, the most common type of cancer, is the third leading cause of cancer-related death in both men and women. However, the risk of death from colon cancer can be reduced with early diagnosis and treatment.
Where does colon cancer pain occur?
In colon cancer, where diarrhoea and constipation occur as symptoms, frequent desire to go to the sink and severe abdominal pain negatively affect the quality of life. These symptoms, which will cause a loss of self-confidence, can bring about a psychologically challenging period. Psychological support can be provided at this stage where depression and anxiety disorders may occur.
I have no family history of colon cancer or polyps. Should I start getting tested for colon cancer?
Genetic transmission of diseases to the next generation is possible. However, the absence of a family history does not mean that colon cancer will not be seen. Therefore, tests should be performed even for control purposes in the early period.
Do polyps mean that I will get colon cancer?
Polyps are usually benign. However, whether polyps will cause cancer should be evaluated under the follow-up of a specialist physician.
Is colon cancer genetic?
In colon cancer, in which environmental factors play an important role, it is possible that some genetic disorders may be transmitted from parents to the next generation. Genetic disorders may develop with environmental factors.
Can women get colon cancer?
Colon cancer, known as colon cancer, which is one of the most life-threatening cancer types, can be seen in men and women regardless of gender.
What kind of diet should I follow to prevent colon cancer?
It is thought by experts that the Mediterranean-type diet plays an important role in preventing colon cancer. According to researches, excessive red meat consumption can trigger colon cancer. According to the Mediterranean-type diet, red meat consumption is minimised and vegetables are predominantly consumed. Consumption of fresh fruits and vegetables cooked in daily life is a part of this diet.
Who can get colon cancer?
It is stated that it is more common in advanced age, those with a sedentary life, overweight, those who use alcohol or tobacco, and those who consume processed meat products.
Where is colon cancer most common?
Colon cancer is reported to be more common in African and American races. It is also a common cancer in our country.
Can colon cancer be detected in a blood test?
Colon cancer cannot be diagnosed with a blood test alone. Additional examinations are required.
Why does colon cancer occur?
The causes of colorectal cancer can be listed as lifestyle, malnutrition, overweight, changes in environmental factors and inherited genetic factors.
Is stage 4 colon cancer curable?
Surgery is not preferred in stage 4. Chemotherapy and radiotherapy aim to shrink the cancerous cells. The treatment and prognosis of each stage 4 patient is not the same. It varies according to the spread of the disease and the response to treatments.
Is colon cancer benign?
Colon cancer is a malignant tumour of the large intestine. Sometimes benign polyps can turn into cancer.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS BLADDER CANCER?

The bladder, whose main task in the body is to store urine, is an organ that can stretch as it fills with empty urine. Bladder cancer usually starts from the urothelial cells of the mucosa lining the inner surface of the bladder. Bladder tumours can be malignant or benign. However, non-cancerous benign bladder tumours can also be seen.
WHAT ARE THE SYMPTOMS OF BLADDER CANCER?
Bladder cancer symptoms are as follows;
- Blood in the urine (haematuria): In bladder cancer, painless bleeding is usually seen in the urine. There may be visible bleeding in the urine, as well as bleeding that can be seen under a microscope. Haemorrhages may not be in the whole urine but may also occur in the form of blood clots. Blood in urine can be caused by many reasons other than tumours. It should not be forgotten that different diseases such as kidney stones or infection can cause blood in the urine.
- Painful urination
- Frequent urination
- Urinary urgency
- Discomfort such as difficulty urinating or even inability to urinate due to clots may be a symptom of bladder cancer.
In some cases, when the first symptoms of bladder cancer appear, the cancer may have already metastasised to another part of the body. Symptoms experienced in patients with metastasis may vary depending on the area where the cancer has spread. In progressive bladder tumours;
- Back pain
- Pain in the lower abdomen
- Symptoms such as loss of appetite and weight loss may occur.
WHAT ARE THE CAUSES OF BLADDER CANCER?
Although the exact cause of bladder cancer is not known, there are risk factors that may cause it.
- Smoking: The most common risk factor for bladder cancer is smoking and tobacco use. Smokers of cigarettes and tobacco products are 4-7 times more likely to develop bladder cancer than non-smokers. The risk also increases in passive smoking.
- Age: Bladder cancer is more common after a certain age. The majority of people diagnosed with bladder cancer are over the age of 50.
- Gender: Men are 3 to 4 times more likely to develop bladder cancer than women. However, in recent years, the widespread consumption of cigarettes among women causes an increase in the incidence of bladder cancer in women. Women are more likely to die from bladder cancer than men.
- Chemicals: Chemicals used in the textile, rubber, leather, paint, chemical, battery industry or printing industry increase the risk of bladder cancer
- Belonging to the white race
- Chronic bladder infections
- Not consuming enough fluids and retaining urine too much
- Consuming a lot of high-fat or additive foods
- Family history of bladder cancer
- The risk of developing bladder cancer is higher in patients who have received chemotherapy with cyclophosphamide and in patients who have undergone radiotherapy to the adjacent areas of the bladder for other reasons.
HOW IS BLADDER CANCER DIAGNOSED?
Bladder cancer is detected by symptoms or as a result of suspicion during routine checks. Firstly, an examination by an experienced urology doctor is required.
Urology doctor examination
The urologist will first assess risk factors for bladder cancer such as genetics, smoking or radiation exposure. The urologist will perform a physical examination;
- Perform a systemic check and determine if there is a sign of cancer.
- Checks for abdominal and hepatic distension.
- Checks for enlarged lymph nodes in the groin, abdomen and neck.
In cases of abnormal and suspected bladder cancer, additional tests may be requested to clarify the diagnosis.
Urine tests in bladder cancer
- Urinalysis; It is a simple laboratory test. It is done to check blood and other substances in the urine sample.
- Urine cytology: The urine sample is examined under a microscope to check for the presence of cancer cells.
- Urine culture: What kind of microbes are examined in the urine sample kept in the laboratory. It is important for determining whether there is a bladder infection.
- Urine tumour marker tests: A sensitive and specific marker has not yet been found. These tests look for substances released into the blood by bladder cancer cells.
Imaging methods of bladder cancer diagnosis
- Ultrasonography (USG): Ultrasound, which does not require the administration of contrast media, easily detects bladder tumours larger than 5 mm and can also help to find out if the kidneys or ureters are blocked. Ultrasound can also be used to determine the size of bladder cancer and whether it has spread to nearby organs or tissues.
- Computed Tomography (CT urogram): It can provide information about the size, shape and location of all tumours in the urinary tract, including the bladder. It can also help to show enlarged lymph nodes that may contain cancer, as well as other organs in the abdomen and pelvis. Sometimes a contrast medium is given to the patient by mouth or intravenously so that the image can be obtained in more detail. Patients who are allergic to iodine and other substances should tell their doctor in advance.
- Intravenous pyelogram (IVP): This method, which was used in the past to determine abnormalities in the bladder and urinary system, has been replaced by newer and better informative methods.
- Retrograde pyelogram: It is an application similar to intravenous pyelogram. The contrast material used is injected directly into the urinary system using cystoscopy rather than intravenously. The retrograde pyelogram procedure is used to find out what is causing the obstruction to the normal flow of urine. It can also help diagnose cancer in the lining of the ureter or kidney.
- MRI (Magnetic Resonance): It can be used to measure the depth and size of a bladder tumour and to view the lymph where the cancer has spread. The patient needs to be given contrast material to get a detailed image of the tumour and its effects.
- PET CT Scan: A small amount of radioactive material is injected into the patient’s body. As this radioactive material is absorbed by cancerous cells that tend to use energy, it is possible to visualise where in the body the cancer has spread. PET CT is not accepted as standard imaging for bladder cancer. It may have a potential role in the evaluation of metastatic bladder cancer.
- Chest X-ray: Can be used to determine whether bladder cancer has spread to the lung. Chest X-ray is not required if a CT scan of the chest has been performed.
Cystoscopy
Cystoscopy is one of the gold standard procedures in the diagnosis of bladder cancer. A thin flexible endoscope with a light and a camera at the end is used to examine the urethra and the inside of the bladder. During cystoscopy, the size, location and growth patterns of abnormalities in the bladder can be determined. Biopsies and urine samples can also be performed during cystoscopy.
Biopsy – Transurethral resection of bladder tumour (TUR-BT)
During cystoscopy, the urologist takes a piece of abnormal tissue and sends it to the laboratory for examination. During this procedure, which is also called transurethral resection of bladder tumour (TUR-BT), a sample of the bladder tumour and bladder muscle close to the tumour can also be removed. During the biopsy procedure, he can assess the bladder to see if any masses are palpable. TUR-BT can also be used in the treatment of non-muscle invasive bladder tumours.
TREATMENT OF BLADDER CANCER
Bladder cancer treatment options depend on various factors such as the patient’s general health condition, the type of cancer, the grade of cancer and the stage of cancer.
Surgical treatment of bladder cancer
The type of surgical treatment in bladder cancer may vary depending on the type of bladder tumour and the stage of the cancer.
TUR surgery (Transurethral resection): Transurethral resection of bladder tumour,
TUR surgery, is generally used to remove tumours that are not muscle invasive, that is, tumours that are located in the mucosa of the bladder and do not extend to the muscle layer of the bladder wall. TUR can also be used in the diagnosis and staging of bladder cancer.
TUR surgery can be performed under general anaesthesia or regional anaesthesia. TUR surgery is performed without any incision in the body, by entering through the natural hole at the end of the urinary tract.
During TUR surgery, the urologist reaches the bladder with an endoscope with a small “U” shaped wire at the end.
The cancerous tissue is cut with electric current and removed from the body. In very small tumours, the treatment is eliminated by burning the cancerous cells area after the piece is removed.
After TUR surgery, the urologist may recommend chemotherapy administered through a catheter into the bladder once a week for 6-8 weeks or once a week for 6-8 weeks to destroy the remaining cancer cells and prevent recurrence.
Partial or segmental cystectomy: Surgical removal of the tumour and part of the bladder. The place of partial cystectomy surgery in the treatment of bladder cancer is extremely limited and is only applied in the treatment of cancers with special histology.
Radical Cystectomy: It is a surgical method in which the entire bladder and nearby tissues and organs are removed together with the tumour. In radical cystectomy surgery, in addition to the bladder, the prostate and seminal vesicles of men, and the entire urinary tract in necessary patients are removed. In women, all or part of the uterus, fallopian tubes, ovaries and uterus are removed in the classical definition, but removal of the bladder with safe limits while leaving the gynaecological organs in place has also been applied in recent years.
In both men and women, pelvic lymph node dissection, the removal of the lymph in the pelvis, is also part of the operation. Pelvic lymph node dissection is the most accurate way to detect cancer that has spread to the lymph.
In radical cystectomy surgery, which can be performed laparoscopically or robotically, the surgical procedure can be completed with smaller incisions instead of large incisions in open surgery.
New bladder from the intestine (Neobladder reconstruction): Since the bladder of patients undergoing radical cystectomy surgery is removed, a new way for urine to exit the body is required. There are different types of urinary diversion surgery, including methods in which a new bladder is created from part of the intestine. Which urinary diversion method is suitable for the patient is decided by the urology doctor by evaluating the biological age of the patient, the stage of the existing diseases and the possibility of treatments such as chemotherapy and radiotherapy that may be required later. The final decision is made after a detailed discussion with the patient.
Chemotherapy treatment in bladder cancer
It is used to destroy bladder cancer cells that have spread throughout the body. Living without a bladder can sometimes negatively affect the patient’s social life.
Chemotherapy and radiation therapy can be used as an alternative to bladder removal for patients who are eligible to keep all or part of the bladder.
Chemotherapy for bladder cancer can be administered in two different ways.
- Systemic Chemotherapy: Systemic chemotherapy is also known as whole body or intravenous chemotherapy. In the method applied by a Medical Oncologist, chemotherapy drugs given intravenously are aimed to circulate throughout the body and destroy cancerous cells.It is used for metastasised bladder cancer or after radical cystectomy in selected cases. Systemic chemotherapy can also be used to shrink the tumour before surgery.
- Intravesical Chemotherapy: Intravesical or local chemotherapy is usually administered by a urologist. Since cancer cells do not reach deep muscle tissues in superficial bladder cancers, intravesical chemotherapy can be used as a complement to TUR treatment in these patients. In intravesical chemotherapy, drugs are delivered to the bladder through a catheter inserted into the urethra.
Radiation Therapy in Bladder Cancer
It can be used in addition to TUR or after TUR in combination with chemotherapy to treat bladder cancer in patients who are not suitable for surgery or who do not want surgical treatment. It may be preferred to reduce complaints caused by a tumour such as pain, bleeding or obstruction or in the treatment of metastasised cancers.
Immunotherapy in Bladder Cancer
Immunotherapy, also called biological treatment, is the use of drugs to help the immune system recognise and destroy cancer cells. In the treatment of bladder cancer, immunotherapy is usually applied directly into the bladder. BCG vaccine, which is administered into the bladder with a catheter as a liquid, provides treatment by activating the immune system cells in the bladder.
In recent years, studies on T cells, which support the immune system and are known to have a protective effect against infection and cancer, have yielded positive results.
FREQUENTLY ASKED QUESTIONS ABOUT BLADDER CANCER
How common is bladder cancer?
Bladder cancer is the seventh most common cancer in men, it is less common in women. However, bladder cancer is a more deadly cancer in women. The American Cancer Society estimates that 80,000 people (62,000 men and 18,000 women) will be diagnosed with bladder cancer in the US in 2019.
Which doctor should I see for bladder cancer or benign bladder tumours?
The diagnosis and treatment of bladder cancer or benign tumours of the bladder, which can occur at any age, although it is usually seen after the 50s, is carried out by Urology doctors. Since there are also surgical methods in the treatment of bladder cancer and benign bladder tumours, it is important to choose a urology doctor specialised in this field.
What are the types of bladder cancer?
Different cell types in the bladder can be cancerous. Bladder cancer can be divided into types according to the bladder cell where the cancer starts. The type and stage of bladder cancer are also determined by the tests used in the diagnosis of bladder cancer.
- Urothelial carcinoma: Urothelial carcinoma, also known as transitional cell carcinoma, is the most common type of bladder tumour. It arises in the urothelial cells lining the inside of the bladder. Urothelial cells are also found in other parts of the urinary tract. For this reason, the entire urinary tract of patients with bladder cancer should be checked.
- Squamous cell carcinoma: It starts with the formation of thin, flat cells in the bladder after a prolonged infection, irritation of the bladder or prolonged use of a catheter. Under the microscope, the cells look very similar to the flat cells found on the surface of the skin.
- Adenocarcinoma: About 1 per cent of bladder cancers are adenocarcinomas. It occurs in the mucus-secreting glands of the bladder. It occurs after prolonged irritation or infection in the bladder.
- Small cell carcinoma: Less than 1% of bladder cancers are small cell carcinomas. It starts in nerve-like cells called neuroendocrine cells. These cancers often grow rapidly and need to be treated with chemotherapy, which is usually used in small cell carcinoma of the lung.
- Sarcoma: Sarcomas start in the muscle cells of the bladder, but are very rare.
Bladder cancer tumours can also be classified according to the microscopic appearance of the cancerous cells.
- Low-grade bladder tumour: Also called well-differentiated bladder tumour. The appearance and organisation of cancerous cells are close to normal healthy cells. Low grade bladder tumours grow more slowly.
- High grade bladder tumour: Also called poorly differentiated bladder tumour. The appearance of cancerous cells and tumour is not similar to normal healthy cells. High-grade bladder tumours show a more aggressive behaviour.
Bladder cancers can also be diversified by their proximity to the bladder wall.
There are many layers of different cells in the wall of the bladder. Most bladder cancers start from the innermost layer of the bladder in contact with urine and spread to the muscles of the bladder over time. Those that reach the bladder muscle layer then spread outside the bladder and to nearby neighbouring structures. Bladder cancer can metastasise to nearby lymph or other parts of the body. Bladder cancer often spreads to distant lymph nodes, bones, lung or liver.
- Non-invasive bladder cancer: It is a cancer of the bladder that does not spread to the muscle and remains in its inner layer. It is also defined as superficial bladder cancer or early stage bladder cancer.
- Invasive bladder cancer: It means that cancer cells have spread deeper than the inner layer of the bladder, into the muscle layer. If left untreated, there is a risk of the cancer spreading to other parts of the body. These cancers are more likely to spread and must be treated.
Bladder cancer is also diversified according to the way it grows.
- Papillary Urothelial Carcinoma: Papillary tumours are growths that start in the urothelial cells in the bladder mucosa and extend into the inner cavity of the bladder. Sometimes, although these cancers grow, they remain in the bladder without spreading. However, more aggressive types of this cancer can spread to the deeper layers of the bladder and then to other organs.
- Flat carcinoma (carcinoma insitu): It does not grow into the deep part of the bladder or into the inner cavity. It is an invasive tumour form that spreads in the bladder wall in a flat tumour layer structure.
What are the stages of bladder cancer?
In order to determine the stage of bladder cancer, 3 criteria are taken into consideration.
- The depth of the cancerous tumour in the bladder wall and the degree of the tumour
- Whether the bladder tumour has spread to regional lymph nodes
- It is examined whether bladder cancer has metastasised to other organs such as the lung or liver.
The information obtained from pathology and examinations is used to find out which parts of the bladder are cancerous, whether the cancer has spread from where it started and where the cancer has spread. Bladder cancer staging is performed according to the international TNM system.
Risks and Side Effects of Surgical Treatment in Bladder Cancer
TUR surgery
- Side effects of bladder cancer TUR surgery are usually mild and do not last long. Pain during urination and mild bleeding may occur after TUR surgery. These effects return to normal within 1-2 weeks.
- Although the bladder tumour is completely removed after TUR surgery, the tumour may recur.
- Multiple TUR surgeries may cause problems such as stenosis in the urinary tract.
Radical Cystectomy and new bladder from the intestine or ileal loop diversion surgery
- Radical cystectomy surgery is heavier than TUR surgery. Side effects of anaesthesia can be seen.
- Bleeding
- Infection
- Blood clots in the legs or lungs
- Damage to neighbouring organs
- Incontinence or obstruction of urine flow
- In men, the disappearance of sperm output and erection problems can be seen. Erection problems and sexual reluctance can be prevented with new nerve sparing surgical techniques. In women, menopause and sexual reluctance may occur, but organ preserving techniques are preferred in age appropriate patients.
What should be the follow-up process after bladder cancer treatment?
Since there is a risk of recurrence of bladder cancer in bladder cancer patients after treatment, the follow-up process is very important. Follow-up is an important part of cancer treatment. Follow-up after bladder cancer treatment may vary depending on the stage and grade of cancer and the type of treatment applied. The possibility of recurrence of bladder cancer is high for the first 2 years after treatment, after which follow-up is extended up to 10 years, although the possibility of recurrence decreases.
Although the follow-up process varies according to the patient, it is important to check every 3 months in the first year. During the follow-ups, the liver and lymph nodes are checked and the bladder is observed by cystoscopy to determine whether there is any recurrence in the bladder. Imaging methods such as CT, MRI, ultrasound, PET CT are also used when deemed necessary by the treating physician.
What is the survival time in bladder cancer?
Survival or survival time from bladder cancer varies from person to person. Success varies according to the type of bladder cancer, its stage, the number and size of tumours, the characteristics of the cancer, recurrence, the selected treatments and the patient’s response to the treatment.
Therefore, survival rates in bladder cancer are actually personalised. In the study of the American Cancer Society considering all stages of bladder cancer, the 5-year survival rate for people with bladder cancer is 77%, 10-year survival rate is 70%, 15-year survival rate is 65%.
To which organ does bladder cancer most often metastasise?
Bladder cancer most often metastasises to the lungs, liver or bones.
How should bladder cancer be nourished?
It is not known exactly what reduces the recurrence rate after bladder cancer treatment. The benefit of nutrition in the development of bladder cancer or after treatment is not clear in scientific studies. However; quitting smoking, eating a natural and balanced diet, and engaging in regular physical activities can be beneficial.
Is there a herbal or natural treatment method for bladder cancer?
There is no scientific evidence that diet, herbal products, vitamins and minerals prevent the development of bladder cancer or reduce the possibility of recurrence. Many studies have been conducted on this subject, and in general, natural and healthy nutrition and active mobility are recommended.
Does bladder cancer occur in young people?
Bladder tumour is generally a common disease over the age of 50. However, in practice, it is observed even in the 20s. In addition, the incidence of bladder tumours in men is approximately 4 times higher than in women. However, when seen in women, it tends to have a worse prognosis.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS METASTATIC CANCER?

Metastasis refers to the spread of cancer to a more distant site than the organ from which it originated. Metastasis becomes detectable when cancer cells spread from their origin to another part of the body through the bloodstream or lymphatic vessels and form new tumour foci.
Cancer can spread in one of three ways:
- Through tissue: Cancer can spread from the site of origin to nearby areas by growing through the neighbourhood.
- Through the lymphatic system: Cancer cells can spread through the lymph vessels to other parts of the body.
- Through the blood: Cancer cells can move through blood vessels to other parts of the body.
Lymph nodes are the most common place where cancer metastasises. Cancer cells also tend to spread to different organs such as the liver, brain, lungs and bones. Some types of cancer are more likely to spread to certain organs. For example, prostate cancer most often spreads to the bones. Cancer cells originating from bone tissue tend to settle in the lung tissue most often.
WHAT ARE THE SYMPTOMS OF METASTATIC CANCER?
The complaints (i.e. symptoms) of metastatic cancer vary depending on the type of cancer and where it has spread. For example, common symptoms of cancer that has spread to the brain, i.e. brain metastases, may include headache, seizures, vision problems (such as blurred vision, double vision, visual field defects), dizziness, while liver metastases may cause complaints such as loss of appetite, bloating, early satiety, indigestion, jaundice (yellowing of the skin or eyes).
In some cases, cancer cells can spread even after the primary cancer has been treated. Metastatic tumours can occur months or even years after the initial cancer treatment.
WHAT ARE THE DISTINGUISHING FEATURES OF METASTASIS?
In order for a cancer cell to be “metastatic”, it must have the following characteristics
Mobility and invasion
Invasion, the defining characteristic of malignancy, is the capacity of tumour cells to disrupt the basement membrane (a thin, fibrous, extracellular tissue matrix that separates the lining of an internal or external body surface from the underlying connective tissue) and pass through the underlying connective tissue (the connective tissue of the tumour). Motility, i.e. the capacity of cancer cells to move, is not sufficient for metastasis; if a cancer cell can successfully detach from a tumour focus but does not survive afterwards, it cannot metastasise.
The ability to change secondary sites
Cancer cells recruit new cells into the local microenvironment, mobilise immune/inflammatory cells, restructure other tissues, alter the metabolism of the surrounding stroma, inhibit all antitumour actions of the immune system, manipulate and alter the behaviour of other cancer cells.
Reconstructs the extracellular matrix and normal behaviour of other cells.
Plasticity
Primary or secondary tumours are not static; at the cellular level they are actually very dynamic. Cancer cells must adapt their metabolism to meet the demands that accompany the rapid growth of the primary tumour and the colonisation of different metastatic sites. Moreover, neoplastic cells can alter the growth rates of other cells, drug resistance and metastatic capacity.
Ability to colonise secondary tissues
Colonisation of secondary tissues is the hallmark of metastatic cancer. In the Hurst-Welch study, if a tumour cell or cells break away from the primary tumour and survive, but fail to take root elsewhere in the body, it cannot metastasise.
WHAT ARE THE TREATMENT OPTIONS FOR METASTATIC CANCER?
Metastatic cancer is more difficult to treat than early stage cancer. Treatment options differ greatly for each type of cancer. As a matter of fact, there is no single treatment method defined for cancer or metastasis. As researchers continue to make advances in treatment, certain types of metastatic cancer are increasingly treatable.
In some clinical situations, metastases can be treated in specific ways.
For brain metastases;
Depending on the number of tumours and the extent of disease in the rest of the body, treatment options may include surgery (in very special cases), radiotherapy, gamma knife surgery, smart therapies, chemotherapy and/or steroids.
For bone metastases
If bone metastases do not cause pain or threaten fracture, they can be monitored during systemic treatment or treated with medication. If severe pain is present or the bone is fragile, surgery and/or radiotherapy may be performed at the site of damage. There are non-chemotherapy drugs known to reduce the risk of pain and fractures associated with bone metastases.
For lung metastases
The treatment of lung metastases depends on the number and size of the metastases and how the primary cancer is being treated. In most scenarios, they will be treated in the same way (with the same medicines) as the primary cancer. If the metastasis is causing fluid to form around the lung, a procedure to remove the fluid to make breathing easier (thoracentesis) and a procedure to seal the lung membranes to prevent fluid from forming again (pleurodesis) may be performed.
For liver metastases
There are various ways to treat liver metastases, depending on the type and extent of the primary cancer as well as the number and size of the liver metastases. In most cases, liver metastases will be treated in the same way (with the same drugs) as the primary cancer.
In cases where there is limited disease, both primary and metastatic, there are different new approaches, for example surgery and radiofrequency ablation (RFA), radio or chemoembolisation (such as TARE, TAKE), microsphere therapy. Liver transplantation is usually not an option for metastatic disease.
Note : In cases where the cancer cannot be cured, the mainstay of treatment is to slow the growth of the cancer or to reduce or alleviate the symptoms it causes.
WHAT ARE THE STAGES OF METASTASIS?
The spread of cancerous cells to new parts of the body occurs in the following stages:
- Separation from the primary tumour
- Invasion from tissues around the initial lesion and penetration of their basement membrane
- Entry into blood vessels and survival in the blood. (Spreading through blood vessels is called haematogenous spread)
- Entry into the lymphatics or the peritoneal cavity (so-called lymphatic spread, which spreads through the lymph ducts)
- Lungs, liver, brain bone, etc. reach distant organ
- The formation of a new lesion with new blood vessels supplying the tumour (the formation of new blood vessels is called angiogenesis).
HOW TO CONTROL METASTASIS?
Some cancers are metastatic at the time of diagnosis, while others become metastatic after the cancer has progressed or relapsed. Doctors use different medical tests to help check for metastasis:
Laboratory tests involve checking body tissues, blood, urine or other substances in the body. These tests help the care team to know how the person’s organs are working.
Imaging tests use X-rays, magnets, radio waves and computer technology. These tests create detailed images of bone and internal organs and structures to check for cancer.
WHY IS METASTASIS DANGEROUS?
Metastasis is of great importance as most cancer deaths are due to the spread of the primary cancer to distant sites. In most cases, cancer patients with localised tumours have a better chance of survival than those with metastatic tumours.
New evidence suggests that 60 per cent to 70 per cent of patients have initiated the metastatic process at the time of diagnosis. In addition, even patients with no evidence of tumour spread at the time of diagnosis are at risk of metastasis.
WHAT IS THE SEED AND SOIL THEORY OF METASTASIS?
Some organs are more prone to metastasis of primary tumours than others. This was first discussed by Stephen Paget a century ago in 1889 as the ‘seed and soil’ theory. For example, bones are the preferred site for prostate cancer, colon cancer spreads to the liver, stomach cancer can metastasise to the ovaries. The theory states that it is difficult for cancer cells to survive outside their primary foci. In other words, cancer cells need to find a place with similar characteristics in order to spread. For example, breast cancer cells need calcium ions from breast milk to multiply.
Therefore, since bones are rich in calcium, bone can be a site of spread.
Malignant melanoma supports melanocytes and nerves and can therefore spread to the brain, as neural tissue and melanocytes originate from the same cell line in the embryo.
The ‘seed and soil’ theory was challenged by James Ewing in 1928. Ewing proposed that metastasis occurs by purely anatomical and mechanical means. Ewing postulated spread through lymphatic channels and blood vessels, noting that cancer cells affect regional lymph nodes close to the primary tumour.
CAN METASTASIS BE PREVENTED?
The risk of developing secondary cancer depends on many factors, such as the type of cancer and the age of the patient in whom the cancer develops. While it is possible to prevent metastasis in a significant group of patients, it is unfortunately not yet possible to prevent it completely.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS STOMACH CANCER?

Stomach cancer, which is the 4th most common cancer among all cancers, is located in any part of the stomach and can usually spread to organs such as lymph nodes, liver and lungs. Gastric cancer occurs as a result of the development of malignant tumours in the gastric mucosa due to various reasons. Gastric cancer, which is among the most common cancers in our country, causes 800 thousand people to lose their lives every year in the world. Stomach cancer, which is more common in men than in women, can be diagnosed early and controlled with the right treatment applications thanks to the developments in technology in recent years. It is possible to prevent and get rid of stomach cancer with expert control and proper nutrition.
WHAT ARE THE SYMPTOMS OF STOMACH CANCER?
Stomach cancer may not give any symptoms in the early period. The first symptoms of stomach cancer are indigestion and bloating. Reluctance to meaty foods is also among the symptoms of stomach cancer. In the later stages of stomach cancer; abdominal pain, nausea, vomiting, bloating after eating, weight loss are observed. Especially patients over the age of 40 who have not had similar complaints before should definitely pay attention to indigestion and weight loss.
Symptoms of stomach cancer are very important to catch the disease at an early stage. As soon as you notice various digestive system disorders, pain in the stomach area and indigestion complaints, it is very important to consult a specialist doctor to catch stomach cancer at an early stage.
We can briefly list the symptoms of stomach cancer as follows.
- Acidity and belching: Increased stomach acid and belching are very common symptoms in stomach cancer cases. However, it does not mean that everyone who experiences these complaints will have stomach cancer.
- Feeling of fullness: One of the prominent symptoms of stomach cancer is feeling full earlier than normal while eating. Prolonged feeling of fullness can cause weight loss.
- Bleeding and fatigue: Stomach cancer can cause bleeding in the stomach in the early stages. Continuous bleeding can also cause anaemia. As your red blood cells decrease, you may start to look paler and become breathless. In some cases, vomiting blood can also be seen.
- Blood clots: People with stomach cancer are more likely to have blood clots. Therefore, in case of sudden chest pain, shortness of breath and swelling of the legs, it is urgent to prevent blood clots. In this case, it is necessary to consult a specialist doctor immediately.
- Nausea and difficulty swallowing: Nausea and dysphagia are very important symptoms of stomach cancer. They are two of the most prominent symptoms seen in more than half of people with stomach cancer. These symptoms are accompanied by pain under the stomach or breastbone.
- Symptoms of advanced stomach cancer: When stomach cancer progresses, blood in the stool, fluid in the abdomen, loss of appetite and weight loss may be encountered
Stomach cancer can sometimes progress insidiously without any symptoms. When symptoms are seen in late stages, the patient may have lost the chance of surgical intervention. Therefore, early diagnosis is very important for stomach cancer.
WHAT CAUSES STOMACH CANCER?
Stomach cancer can have many causes. Stomach cancer can develop and spread in any part of the digestive system organs. Behaviours and risk factors affecting all organs involved in the digestive process can also trigger stomach cancer. These can be listed as follows;
- Diet: The most important cause of stomach cancer is wrong eating habits. Especially barbecued meat and similar foods, over-salted and pickled vegetables, processed foods prepare the ground for stomach cancer. The best way to prevent stomach cancer is to adopt a Mediterranean-type diet. Organic and fresh fruits and vegetables are protective against stomach cancer.
- Infections: An important factor causing stomach cancer is H.plori infection.
H.plori infection is seen in 65-85% of stomach cancer cases. Gastric cancer is also found in 2% of cases with H.plori infection.
- Smoking and Alcohol: Another preventable cause of stomach cancer is smoking. Especially when consumed with alcohol, it increases the likelihood of stomach cancer. The risk of stomach cancer can be reduced by avoiding smoking and alcohol.
- Genetics: Genetic factors are important in stomach cancer as in all other cancers. Genetic factors come to the fore in 10% of stomach cancer cases.
HOW TO RECOGNISE STOMACH CANCER? HOW IS IT DIAGNOSED?
Early diagnosis of stomach cancer is very important for the success of treatment. For this reason, it is very important for people who have problems in their stomach to be followed up with endoscopy under the control of specialist doctors in the early period. With endoscopy, your doctor can observe your oesophagus, stomach and the first parts of the small intestine with a long tube with a lighted camera. If there are parts that appear abnormal, a biopsy is taken for a definitive diagnosis. With the appropriate use of endoscopy, it is possible to catch the disease at an early stage. Apart from endoscopy, contrast radiographs and computed tomography are other important diagnostic methods that provide the diagnosis of gastric cancer.
Further tests are needed to determine the stage of stomach cancer and to see whether it has spread to other organs.
These tests are also necessary to determine the most appropriate treatment for the patient. Tests such as Computed Tomography (CT) to determine the size and location of stomach cancer, Laparoscopy and MRI to check whether the cancer has spread, PET-CT, Kidney ultrasound, chest x-ray can be applied.
TYPES OF STOMACH CANCER
After the diagnosis of stomach cancer and the type of cancer is determined, the treatment to be applied is decided. The most common type of stomach cancer is adenocarcinoma. We can explain the types of stomach cancer as follows;
- Adenocarcinoma: 95 out of every 100 stomach cancers are adenocarcinoma. Adenocarcinoma, which is the most common type of stomach cancer, starts in the stomach lining gland cells.
- Squamous cell cancer: Squamous cell cancer, which is treated in the same way as adenocarcinoma, is skin cell-like cells between the gland cells that make up the stomach lining.
- Lymphoma of the stomach: Lymphoma of the stomach is very rare, but it is different from other cancers of the stomach.
- Gastrointestinal stromal tumours (GIST): Rare gastrointestinal stromal tumours (GIST) can be benign or malignant. This type of cancer occurs in the connective tissue cells that support the organs of the digestive (gastrointestinal) tract, most commonly in the stomach.
- Neuroendocrine tumours (NETs): Neuroendocrine tumours (NETs) can be benign or malignant (cancer). This rare type of cancer usually grows in hormone-producing tissues in the digestive tract.
HOW IS STOMACH CANCER TREATMENT PERFORMED?
After the diagnosis of stomach cancer and the type of cancer is determined, the treatment to be applied is decided. Stomach cancer treatment requires a multidisciplinary approach. Success can be achieved with expert teamwork and a well-equipped hospital. In the treatment of gastric cancer, the most important part of the treatment is the appropriate removal of the tumour causing cancer. Successful surgical operations performed at an early stage are very important for the patient’s life expectancy. A part or all of the patient’s stomach can be removed by surgery. In patients whose stomach is completely removed, a new stomach is made from the intestine and the patient can continue his/her life normally.
Patients living in this way are offered dietary recommendations that require eating little and often. In some patients, after the stomach is removed, radiotherapy or drug treatment can be applied as determined by the doctor depending on the form of cancer.
HYPERTHERMIA TREATMENT IN STOMACH CANCER
During the treatments that vary according to the stage of stomach cancer, chemotherapy is applied if the tumour has spread to the lymph nodes.
Chemotherapy treatment given before the operation, especially in stomach cancer starting from the second stage, is very important to increase the effectiveness after the operation. In addition, hot chemotherapy called “Hyperthermia” in the treatment of gastric cancer provides successful results in suitable patients. Hot chemotherapy called hyperthermia is actually a treatment method that has been applied for the last 20-30 years. The method, which was first applied on female cancers for the first time, has recently been applied frequently in large intestine and stomach cancers.
Stomach Cancer Surgery
During gastric surgery, which takes approximately 2-5 hours, a large part or all of the stomach is removed. After gastric surgery, it is recommended that the patient be fed at frequent intervals, in small portions and chew and swallow the food very well. After stomach cancer surgery and treatment, regular controls should be continued.
FREQUENTLY ASKED QUESTIONS ABOUT STOMACH CANCER
Do barbecued meat and smoked foods cause stomach cancer?
Although barbecued meat is very popular, cooking the meat to the point of burning and using too much salt while marinating causes the meat to turn into a carcinogenic food. Especially in the eastern regions, we encounter smoked foods more frequently. Smoked meat, fish, cheese, pickled foods, raw meat, foods containing nitrate salts, canned and prepared foods can lead you to stomach cancer
How does hot tea affect the stomach?
Although tea is usually consumed hot, if it is drunk too hot, it causes irritation on the oesophagus and gastric mucosa. This irritation also prepares the ground for cancer. Hot tea is one of the most common causes of stomach cancers in the Black Sea and Eastern Black Sea regions.
What is the relationship between smoking and stomach cancer?
Stomach cancer is more common in smokers. However, stomach cancer is a type of cancer that is more common in people with polyps in the stomach, in people with helicobacter pylori infection or in Asian societies who consume a lot of smoked foods and pickles. However, the frequency of stomach cancer decreases where people have more access to fresh fruit and vegetables.
Do gastritis and ulcers turn into cancer?
Helicobacter pylori infection causes gastritis and ulcers and is one of the causes of stomach cancer. In cases of gastritis and ulcers, this bacterium must be eliminated. In addition, smoking and alcohol use should be avoided to prevent stomach cancer. Zinc and lead in the water you drink is an important factor causing stomach cancer. In addition, environmental factors such as talc and asbestosis in the air you breathe are also risk factors.
Do stomach cancer patients have bad breath?
A dead tissue appears in the stomach outlets of people with stomach cancer. In the place where this dead tissue is located, bacteria that start to feed from here grow. This condition causes an extremely bad odour. However, if stomach cancer is advanced enough to cause bad breath, it means that there are other symptoms before it. Therefore, people with bad breath should not worry if they think that the cause of this odour is stomach cancer.
How to prepare for chemotherapy for stomach cancer?
It is important to have a support person during the treatment process. Especially on chemotherapy days, it is important to have a supporter, pay attention to hygiene, and prepare for the chemotherapy process by cutting the hair short as it will fall out.
How long does the recovery process take after stomach cancer surgery?
It may take time to adapt to a new diet after stomach surgery. During this time, abdominal cramps may be experienced at an uncomfortable level. Generally, in the recovery process after stomach cancer surgery, oncological treatments can be taken after a period of 1 month.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS PANCREATIC CANCER?

The pancreas, a 15-centimetre-long dual-functional gland located in the abdominal cavity, is surrounded by the stomach, small intestine, spleen and liver. The pancreas, which has two basic tasks under the name of exocrine and endocrine, has two separate cell groups that enable it to fulfil these tasks. Exocrine secretes the sap that helps digestion and transmits it to the small intestine. Thus, carbohydrates, proteins and fats in food are separated and stored as energy. The endocrine function tries to keep the glucose in the blood at a certain level by secreting glycogen and insulin hormones.
WHAT CAUSES PANCREATIC CANCER?
Pancreatic cancer occurs when the cells in the pancreas begin to proliferate uncontrollably. Mostly pancreatic cancer starts to form in the area where the exocrine cells surrounding the pancreatic ducts are located. Pancreatic cancer that starts in this area is an exocrine tumour, also known as adenocarcinoma. The much rarer type of pancreatic cancer, endocrine tumour, starts in islet cells.
TYPES OF PANCREATIC CANCER
Pancreatic cancer consists of the rare “neuroendocrine” or “islet cell” type, which occurs in hormone-producing cells, and the more common “exocrine” type, which occurs in the ducts carrying pancreatic juice. In exocrine pancreatic cancer, cystic tumours and acinar cell types are less common. “Ampulla Vateri” tumours, which can manifest themselves at the junction of the pancreas and bile duct with the duodenum, are a type that is not considered different from pancreatic cancer until the surgical process.
RISK FACTORS IN PANCREATIC CANCER
Although the causes of pancreatic cancer are not known exactly, smoking and genetic factors are recognised as the most important risk factors for cancer formation.
The biggest known causes of pancreatic cancer can be listed as follows;
- Thirty per cent of pancreatic cancers are caused by smoking.
- Advanced age is an important risk factor for pancreatic cancer.
- Eating a diet that is mostly protein-intensive and devoid of fruits and vegetables increases the risk of cancer.
- People with a high body mass index (BMI) are more likely to develop pancreatic cancer.
- Pancreatic cancer is more common in people exposed to petrol and chemical substances.
- Chronic pancreatitis that is not treated for a long time increases the risk of developing pancreatic cancer.
- Diabetes increases the rate of pancreatic cancer twice compared to healthy individuals.
WHAT ARE THE SYMPTOMS OF PANCREATIC CANCER?
Pancreatic cancer can progress without symptoms in the early stages. Most of the time when it starts to give symptoms, the disease has progressed.
Symptoms of pancreatic cancer may include nausea, loss of appetite, weight loss, slowly developing jaundice, obstruction and pain in the stomach outlet. In the case of cancer located in the head of the pancreas, painless jaundice and a light colour of the large bladder, like glass putty, are observed. Pain in the back, which can be seen due to pancreatic cancer, is usually a harbinger of local spread of the disease and is usually seen in the body and tail of the pancreas and is considered as a sign of progression of the disease. Less common symptoms of the disease are diabetes, diarrhoea and depression, which we may remember as the “3 Ds”. These symptoms can also be observed in pancreatic cancer;
- Abdominal pain that increases after a meal or when you assume a horizontal position
- Gas pains, bloating
- Vomiting and loss of appetite
- Dark or bloody urine
- General weakness
- Enlargement of the liver and gallbladder
- Itching
- Varicose veins
In case of such symptoms, it is important to consult a doctor immediately.
DIAGNOSIS OF PANCREATIC CANCER
Early diagnosis of pancreatic cancer may not be very easy. Because there are no symptoms and findings in the early stages of pancreatic cancer. The fact that the symptoms of pancreatic cancer resemble the symptoms of many diseases and that the pancreas is hidden behind organs such as stomach, small intestine and liver are also effective in the lack of early diagnosis.
Pancreatic cancer is usually diagnosed by detailed imaging of the pancreas and its surroundings with the help of various tests. Staging is used to determine the extent to which cancer cells have spread into and out of the pancreas (the extent of cancer spread). Radiological imaging methods are used for staging. For a correct treatment plan in pancreatic cancer, early diagnosis and cancer stage are very important.
We can list the tests applied to diagnose pancreatic cancer as follows;
- Health history and physical examination of the patient: General physical examination of the patient is performed and past diseases are questioned. If the patient has diseases such as diabetes and pancreatitis, which are risk factors for pancreatic cancer, they are examined.
- Blood test: A blood test is performed to measure the amount of certain substances such as bilirubin. Measurements that are higher or lower than normal are considered as a sign of the disease occurring in the organs or tissues that secrete that substance.
- Tumour markers: In order to detect the presence of cancer in the blood or tissue, a tissue, urine or blood sample is taken and some measurements are made. During these measurements, two tumour markers, CA 19. 9 and CEA, can provide helpful information for pancreatic cancer. These tests are guiding in the follow-up of patients diagnosed with pancreatic cancer rather than making a diagnosis. These types of tests are not performed on healthy individuals.
- Magnetic Resonance Imaging (MRI): MRI is one of the most important imaging methods for pancreatic cancer as in all cancers. It is especially effective in understanding the relationship between the pancreas and the surrounding tissues and the findings inside the liver.
- Computed Tomography (CT): It is one of the most guiding imaging methods in cancer diagnosis. In CT, also known as computed tomography or computed axial tomography, the patient may be given contrast material intravenously or orally to improve the images.
- Positron Emission Tomography (PET scan): PET scanning is also used to determine the location and extent of the tumour. The patient is injected with a small amount of radionuclide-labelled glucose and the places where glucose accumulates are detected. Since cancerous cells accumulate more glucose, they appear darker in colour and are detected.
- Abdominal ultrasound: With abdominal ultrasound, high-energy sound waves are sent into the abdomen. These sound waves hit the tissues and echo. Thus, the abdominal cavity and organs are visualised.
- Endoscopic Ultrasound (EUS): It is a diagnostic method generally performed by inserting an endoscopy device with a light and imaging lens at the end through the anus or mouth. Echoes formed by high-frequency sound waves are perceived by the device and a detailed image of the organs called sonogram is obtained, allowing biopsy of suspicious areas if necessary.
- Endoscopic Retrograde Cholangiopancreticography (ERCP): With this method, the pancreatic duct and the common bile duct and bile ducts can be visualised from the duodenum. A small tubular catheter is inserted through an endoscope into the pancreatic ducts and contrast material is injected to obtain a detailed image of the bile ducts.
- Percutaneous Transhepatic Cholangiography (PTC): A catheter is inserted through the skin with the help of ultrasonography to access the bile ducts. The bile ducts are visualised using X-rays with the help of contrast material given through the catheter. If necessary, the catheter is left in place to drain the bile. This procedure is only used when ERCP cannot be performed.
- Laparoscopy: It is a surgical method that controls the symptoms of disease by looking at the abdomen and internal organs from the inside. Tubular instruments called ports are inserted through millimetric incisions made in the abdominal wall. The abdominal cavity is examined with a camera and instruments inserted through these ports. The location of the tumour and whether it has spread to the peritoneum or other organs can be visualised. A biopsy can be taken to make a diagnosis.
- Biopsy: It is the process of taking a cell or tissue sample for detailed investigation of cancer findings in the tissue. There are several different biopsy methods for pancreatic cancer. It is possible to take a cell sample from the pancreas with a thin needle during X-ray or ultrasound, or the same procedure can be performed during laparoscopy.
PANCREATIC CANCER STAGES
Cancerous cells spread throughout the body through the tissues, lymphatic system and blood. Cancer cells can break away from the main tumour and move to other parts of the body through blood vessels or lymphatic channels and form different tumours. This is called metastasis. Secondary or metastatic tumours have the same characteristics as the main tumour. Pancreatic cancer stages are difficult to detect using imaging tests. Therefore, it is very important to decide whether to remove the entire cancerous tumour before surgical intervention. We can explain the stages of pancreatic cancer in this way;
0: There is no spread at this stage. And pancreatic cancer is limited to only one layer of cells. Pancreatic cancer is neither visible in imaging tests nor with the naked eye.
Stage I: In this stage, the cancer grows locally. Pancreatic cancer is limited to the pancreas.
Stage II: Pancreatic cancer grows outside the pancreas or near the lymph nodes.
Stage III: In this stage, pancreatic cancer spreads more widely. The tumour spreads to nearby major vessels, lymph nodes or nerves, but does not metastasise.
Stage IV: In this stage, pancreatic cancer spreads to distant organs such as the liver.
PANCREATIC CANCER TREATMENT
Pancreatic cancer treatment consists of 3 different methods: surgery, chemotherapy and radiotherapy. This brings up the intervention and control of different specialists in the treatment of pancreatic cancer.
Pancreatic cancer treatment is performed by doctors specialised in gastroenterology, surgery, medical oncology, radiation oncology, interventional radiology and many other fields.
Most patients with pancreatic cancer are not candidates for curative surgery because of early cancer spread to distant organs or widespread local involvement. These patients undergo surgical interventions to relieve obstructive symptoms such as jaundice and pain, which do not prolong life but aim to provide a more comfortable period. Depending on the general condition and comorbidities of the patients, the average life expectancy is between 3 and 6 months in patients in whom pancreatic cancer has spread to other organs in the body. In patients with local spread of the disease, the average life expectancy is 6 to 10 months.
The stage of the disease has a very important place in determining the treatment of pancreatic cancer.
Resectable (suitable for surgical intervention, operable): If the tumour is resectable in pancreatic cancer, surgery, which is the only solution method to cure pancreatic cancer, should be applied. Although the tumour is removed by surgical method, pancreatic cancer may recur most of the time.
Chemotherapy treatment with gemcitabine (gemzar) or 5-FU after pancreatic surgery can delay the recurrence of cancer for up to 6 months.
Locally advanced: Pancreatic cancer is locally advanced but has not spread to distant organs. If the patient is not suitable for surgical intervention, interventions are performed according to the patient’s clinic. If there is bile duct obstruction, a stent can be placed. If there is an intestinal area blocked by cancer, a new pathway is opened between the stomach and small intestine by bypass.
Metastatic (spread to a large area): If pancreatic cancer has spread to the abdomen, liver, lung, bones and brain, radiotherapy or surgery alone is not enough. One of the standard treatment methods for pancreatic cancer that has spread is chemotherapy. This treatment treats the cancer
It prolongs the patient’s life span by shrinking.
Recurrent Pancreatic Cancer: After pancreatic cancer surgery, cancer that recurs in or near the same area is called recurrence. If the cancer will recur in a distant area, it will first occur in the liver. When exocrine pancreatic cancer recurs, the same treatment as for metastatic cancer is planned and the patient is treated with chemotherapy.
Neuroendocrine Pancreatic Cancer (Pnet)
Resectable (suitable for surgical intervention): If surgery can be performed, it is operated by determining the appropriate surgical technique according to the type, size and location of the tumour in the pancreas. Preoperative laparoscopy may be performed to determine the stage and exact location of the tumour.
Anresectable (not suitable for surgical intervention): Neuroendocrine pancreatic tumours usually grow slowly. In these tumours, Gallium 68 DOTATOC method, one of the molecular imaging methods called endocrine cancer imaging, is used and the tumour can be examined. Two methods are applied together in treatment. In order to eliminate the problems caused by the hormone secreted from the tumour, the patient is given proton pump inhibitors called acid secretion reducing stomach drugs. Afterwards, chemotherapy, smart drug application and/or targeted radioisotopes are applied to regress the tumour.
WHIPPLE SURGERY FOR PANCREATIC CANCER
Pancreatic cancer operations are the most difficult and complex operations of surgery. Due to the risk of complications that may occur especially in the postoperative period, it is vital for the patient that both the surgeon and the hospital facilities are adequate.
Whipple surgery in pancreatic cancer is a life-saving surgery for tumours of the pancreatic head, biliary tract and duodenum. Whipple surgery is ideal for the complete removal of tumours occurring in 3 organs that are close and connected to each other. During Whipple surgery, a “Pylorus Protective Whipple” operation is performed to protect the muscular system, also called the stomach valve.
Thus, digestive system complaints are not experienced after the surgery. With Whipple surgery, the head of the pancreas, almost half of the stomach, the entire 12-finger intestine and the part of the bile ducts adjacent to this area are completely removed. The most important aspect of the operation is to ensure the correct coordination of these organs with each other. For this reason, Whipple surgery must be performed by specialised doctors.
BEFORE PANCREATIC CANCER SURGERY
Approximately 85 per cent of patients diagnosed with pancreatic cancer have no chance of surgery. In this case, some treatment options are used. These include shrinking the tumour before surgery and making it suitable for the surgical margin, as well as supportive treatment after surgery.
RADIOTHERAPY IN PANCREATIC CANCER
The most commonly used type of radiotherapy in the treatment of pancreatic cancer is external-beam radiotherapy. Chemotherapy and radiation therapy are usually administered at the same time because they are more effective. Simultaneous chemotherapy and radiotherapy can help shrink and destroy pancreatic tumours.
CHEMOTHERAPY IN PANCREATIC CANCER
Chemotherapy, i.e. drug treatment, is used to stop the growth and division of pancreatic cancer cells.
TARGETED THERAPY FOR PANCREATIC CANCER
Targeted therapy in pancreatic cancer is a treatment method that targets specific genes, proteins or tissue environment that contribute to the growth and survival of cancer.
NANOKNIFE TREATMENT IN PANCREATIC CANCER
An important option for patients who have no chance of surgery in pancreatic cancer is nanoknife ablation treatment. It is a procedure to destroy the tumour without leaving damage to tissues such as vessels, nerves and intestines.
The most suitable patient group in pancreatic cancer, which is one of the most important areas of use of the method, is patients who do not have distant metastasis but cannot undergo surgery because the surrounding vessels are involved. In this group of patients, called local-advanced stage, nanoknife can kill the surrounding tumour tissue without damaging the involved vessels and make patients suitable for surgery again, or increase the survival time by shrinking the tumour.
Patients who are candidates for pancreatic cancer surgery should pay attention before surgery. Patient and doctor communication before surgery, full-fledged surgery and good preparation for surgery, performing all examinations according to the age and general condition of the patient and making decisions according to these examinations, meticulously performing the method of surgery and preliminary examinations according to the condition of the tumour are of great importance.
WHAT IS THE PROCESS AFTER PANCREATIC CANCER TREATMENT?
Pancreatic cancer surgery is one of the biggest operations of general surgery. It is important to have an experienced surgical team for it to be effective. Some people may need to reduce sugar consumption after these operations. After the operation, the patient should follow the doctor’s recommendations. Treatment depends on the patient’s condition and the stage of the disease. Chemotherapy and radiotherapy may also be required. At the end of the treatment, physicians will want to see the patient at certain intervals. These appointments should be kept. Doctors should be told in detail what kind of discomfort the patient is experiencing. Various examinations may be requested at the controls. Sometimes side effects may occur after the treatment is finished. These must be shared with the physicians. Sometimes weight loss may occur due to cancer. For this reason, physicians may ask for various nutritional supplements or new eating habits. Some patients may experience pain. Any pain should be reported to the physician. Effective and rapid pain management can be provided in this regard. Good nutrition, regular physical activity and maintaining a healthy weight are important after treatment. Patients may need emotional support if necessary.
WHAT ARE THE SYMPTOMS OF RECOVERY IN PANCREATIC CANCER?
After Whipple surgery, which is a very important option in the treatment of pancreatic cancer, your patient can recover and return to normal life in about 6 months. Surgery, which was not considered as an option for patients diagnosed with pancreatic cancer in the past 10 years, is an important alternative for patients with many different methods under today’s conditions. Thanks to advanced imaging methods, the patient’s chance of surgery is determined in advance and appropriate treatment is performed. Again, the prolonged recovery periods due to open surgeries that cause large incisions in the body have been replaced by laparoscopic (closed) and robotic surgeries, which have been replaced by a faster return to normal life where aesthetic concerns are eliminated. The rapid recovery after surgery allows patients to receive additional treatments that may be necessary more quickly. In this way, the ten most common symptoms that indicate the presence of pancreatic cancer; symptoms such as intense nausea, loss of appetite, involuntary weight loss, darkening of urine colour, obstruction in the stomach outlet, slowly developing jaundice, back pain, diarrhoea, diabetes and depression disappear after treatment.
FREQUENTLY ASKED QUESTIONS ABOUT PANCREATIC CANCER
Can pancreatic cancer be detected on ultrasound?
Pancreatic cancer can be detected by methods such as abdominal ultrasound, MRI, CT, PET scan.
Where does pancreatic cancer metastasise first?
Pancreatic cancer can metastasise to distant organs at stage 4. The cancer can first spread in the abdomen and liver. Then it can spread to the lungs and bones.
How to recognise pancreatic disease?
There may be symptoms such as loss of appetite, nausea, weight loss, change in stool colour, back pain, gas pains, weakness, itching.
Who can get pancreatic cancer?
The risk of pancreatic cancer is higher in smokers, diabetic patients, people with chronic inflammation of the pancreas, family history, obesity, advanced age and malnutrition.
Does pancreatic cancer kill?
Pancreatic cancer is one of the most dangerous types of cancer because it is usually detected late. Early diagnosis prolongs the life expectancy of patients.
Can pancreatic cancer be overcome?
Pancreatic cancer is a treatable disease when diagnosed early.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.*
Prostate cancer

Prostate cancer is one of the most common types of cancer in men and while the frequency is 28 per hundred thousand in the world, this rate is slightly higher in our country and is 37 per hundred thousand. According to the data of the American Cancer Society, the lifetime risk of men to encounter prostate cancer is 16.7% and the risk of loss of life is 2.5%. One out of every 5-6 men has a lifetime risk of prostate cancer. While prostate cancer is diagnosed every 3 minutes in the world, prostate cancer-related loss of life occurs every 14 minutes.
Prostate cancer is one of the cancer types with high treatment success when caught at an early stage. Since it is a cancer that usually does not give symptoms in the initial stage, every man from the age of 40 must have an annual prostate examination and blood tests. Among the surgical applications that have a very important place in the treatment of prostate cancer, the “da Vinci Robotic Surgery System”, which has revolutionised the world of medicine, provides the patient with important privileges in terms of quality of life as well as achieving a cancer-free life.
With robotic surgery, it is possible to better protect the nerves that provide urinary retention and continuation of sexual life.
WHERE IS THE PROSTATE GLAND LOCATED AND WHAT FUNCTIONS DOES IT HAVE?
The prostate gland, which is part of the male reproductive system, is a gland located just below the bladder, in front of the intestines, surrounding the outlet of the bladder. The prostate, whose main task is to produce the fluid that protects the sperm and to store the sperm in this fluid in a healthy way, also prevents urinary incontinence by squeezing the mouth of the bladder with sphincter muscles. The prostate capsule, which is divided into three regions surrounded by a capsule, separates the prostate from other parts of the body.
WHAT IS BENIGN PROSTATE ENLARGEMENT?
As men get older, the prostate gland enlarges. This enlargement is called benign prostatic hyperplasia (benign enlargement of the prostate) and usually occurs in the transition zone of the prostate surrounding the urethra (urethra). An enlarged prostate can block the bladder or urethra, preventing the flow of urine. Men may experience frequent, painful, bloody urine or sperm problems, and may experience stiffness and pain in the lower back. These symptoms may be the result of benign enlargement of the prostate or may occur as a sign of cancer.
WHAT IS PROSTATE CANCER?
Prostate cancer develops in the prostate, a small walnut-shaped gland that is part of a man’s reproductive system. Prostate cancer occurs when cells in the prostate gland grow out of control. The cancerous cells first grow uncontrollably and spread into the prostate.
Then it extends to the capsule surrounding the prostate, pierces the capsule and spreads outside the prostate. Unlike benign prostate gland enlargement, prostate cancer does not originate from the centre of the prostate, but from the region close to the capsule, away from the centre.
Therefore, urinary complaints in prostate cancer disturb the patient at a later stage. During the growth and spread period, it may spread to nearby organs, lymphatic system and other parts of the body through blood circulation. As prostate cancer has a slow course, the tumour can show a very aggressive character and can spread to bones and other organs.
SYMPTOMS OF PROSTATE CANCER
Symptoms of prostate cancer may appear depending on the progression of the disease. In this respect, it is an insidious disease. Especially in the early stages, there may be no symptoms and complaints.
When the symptoms of prostate cancer appear, the patient may lose some treatment chances, so regular medical check-ups are of great importance in the success of treatment.
Symptoms of prostate cancer can be listed as follows;
- Difficulty urinating
- Decreased strength in the urine stream
- Blood in semen or urine
- Pain during ejaculation
- Discomfort in the groin area
- Bone pains
- Erectile dysfunction
These symptoms that indicate prostate cancer may sometimes be an indicator of benign prostate enlargement. Similar symptoms and complaints may also be seen in benign prostatic hyperplasia (benign enlargement of the prostate), which develops due to enlargement of the prostate gland. If prostate cancer has spread to other parts and organs of the body, it may also give symptoms related to that area. For example; if it has spread to the bone, such as bone pain…
PROSTATE CANCER RISK FACTORS
The cause of prostate cancer is not known exactly. Prostate cancer occurs when some prostate cells grow out of control due to genetic defects at the cellular level and replace normal cells. It can then spread to the surrounding tissues and, in advanced stages, to distant organs.
The causes and risk factors of prostate cancer can be listed as follows;
- Hereditary or Genetic Factors
9% of prostate cancers are hereditary and in 15% of those with prostate cancer, the disease is inherited from first-degree male relatives. Mutation in the BRCA2 gene, which is known to be associated with breast and ovarian cancers in women, has been observed to increase the risk of prostate cancer in men.
- Non-Genetic (Environmental) Factors
Environmental factors are more effective than genetic factors in prostate cancer. For example, while the risk of prostate cancer in a Chinese person living in China is very low compared to an American, the same Chinese individual starts to have a prostate cancer risk similar to an American when he lives in the USA for a long time.
- Effect of Age
The risk of prostate cancer increases with age. Rare in men under 50 years of age, prostate cancer is common in men over 55 years of age. It is known that 1 out of every 6 men will be diagnosed with prostate cancer during their lifetime.
- Race Factor
Race factor is also important in prostate cancer. Prostate cancer is most commonly seen in black men, followed by white men. Rarely, it is also seen in men living in Asian / Pacific islands.
- Nutrition
The direct effect of diet on prostate cancer has not been proven. Earlier research has shown that selenium and vitamin E can reduce the risk of prostate cancer, but clearer results from later studies have shown that neither of them is beneficial. Nevertheless, since a healthy diet reduces the risk of cancer, consuming unhealthy foods can directly increase the risk of prostate cancer.
DIAGNOSIS OF PROSTATE CANCER
If the patient’s PSA blood test and/or rectal finger examination results suggest the possibility of prostate cancer, the suspicion should be confirmed by a biopsy. Prostate cancer is diagnosed after one or more biopsies of the prostate gland. The biopsy determines whether the patient has benign prostatic hyperplasia, cancer or other medical problems. During the biopsy, a needle is inserted through the rectum and several small pieces of prostate tissue are sampled. These tissue samples are examined under a microscope to detect any cancer cells.
The following scans are performed to diagnose prostate cancer;
PSA Blood Test: The PSA level in the blood of the patient diagnosed with prostate cancer is equal to the amount of cancer in the body. PSA (Prostate Specific Antigen) is a protein produced by the cells in the prostate, and the higher the amount in the blood, the more advanced the prostate cancer is. At the same time, the PSA level is extremely helpful in monitoring the success of the treatment given or in detecting regeneration after surgery.
Breech Finger Examination: It is one of the most widely used prostate cancer screening tests. The patient’s prostate is touched with a finger and abnormalities are examined according to its size and characteristics.
Transrectal Ultrasonography: During transrectal ultrasonography, a small probe is inserted into the rectum. The probe emits high-frequency sound waves that produce echoes and bounce back by hitting the prostate. The computer uses these echoes to create the picture with the sonogram, which can show abnormal areas. Research is ongoing that transrectal ultrasonography reduces the risk of survival in prostate cancer.
Advanced PSA Test: Work is underway to improve the PSA test for more specific results for pancreatic cancer. The clearer the PSA results, the less anxiety the patient has and the less need for further tests.
Insulin-like growth factor: Insulin-like growth factor (IGF) is an important growth and antiapoptotic (cell death inhibitor) factor for cancer cells in many types of cancer. Insulin-like growth factor binding protein-3 (IGFBP-3) stimulates apoptosis (cell death) independent of IGF-1 and inhibits growth. Recent studies suggest that high levels of IGF-I and low levels of GFBP-3, or elevated ratios of both, are associated with an increased risk of prostate cancer.
EARLY DIAGNOSIS IN PROSTATE CANCER
As in other cancers, early diagnosis of prostate cancer can reduce the rate of loss of life. Another benefit of early diagnosis is that the side effects of prostate cancer treatment are minimised. Blood test measuring the protein level known as Prostate Specific Antigen (PSA), digital-rectal examination and/or transrectal ultrasound methods are used to detect prostate cancer early.
However, screening for prostate cancer is a complex and controversial issue and there is insufficient evidence that it reduces the risk of survival. Moreover, all screening tests carry some risks. It is important that the uncertainties associated with the benefits and potential harms are discussed with a specialised doctor before prostate cancer screening tests.
Once the potential benefits, uncertainties and risks of screening tests have been discussed together, they should or should not be performed according to the patient’s personal preference.
PROSTATE CANCER STAGES
Prostate cancer is divided into stages according to the extent of its spread. Whether the prostate tumour has spread to surrounding tissues such as the bladder or rectum, whether it affects lymph nodes and bones are the most important criteria in staging. Gleason score and PSA level, which indicate the grade of the tumour, are also important to determine the stages of prostate cancer.
- Stage 1
In stage 1, the tumour is only in the prostate. Sometimes it may be too small to be felt during rectal examination. Gleason score is 6 or lower. PSA level is below 10.
- Stage 2
In stage 2, the tumour is still in the prostate. However, the structure of the tumour is aggressive. It can be felt clearly on finger examination or the tumour grade may be high.
- Stage 3
In stage 4, prostate cancer has spread outside the prostate. It has usually spread to the seminal vesicles. However, it has not spread to bone and lymph nodes.
- Stage 5
At this stage, the prostate cancer has spread to the bladder, rectum or surrounding tissues (except the seminal vesicles). It may also have spread to nearby lymph nodes and bones.
PROSTATE CANCER TREATMENT
In the treatment of prostate cancer, different treatments may be preferred depending on the growth rate of the cancer, its spread, the general health status of the patient and the effectiveness of the treatment to be applied, as well as possible side effects. If prostate cancer is at an early stage, follow-up may be recommended instead of immediate treatment. Surgery is one of the most common and effective treatment methods in prostate cancer. Robotic, laparoscopic and open surgical methods are available and each surgical method should be preferred according to the patient. The aim of the surgical approach is to remove the entire prostate. In appropriate cases, the nerves around the prostate that help penis erection can be preserved.
Laparoscopy is the preferred surgery in early stage prostate cancer. Prostate radiotherapy (radiotherapy) is also an important treatment option in appropriate patients.
Laparoscopic surgery provides the patient with a comfortable operation process and has high success rates in terms of cancer control. After these surgeries, which are performed through 4-5 small holes, the patient experiences less pain and can return to daily activities in a short time. Since there is no surgical incision, these surgeries provide a great deal of patient satisfaction cosmetically. Major advances in the diagnosis and treatment of prostate cancer make this disease no longer a feared disease.
TREATMENT ACCORDING TO PROSTATE CANCER STAGE
If prostate cancer is in stage 1 or 2, it can be treated with surgery or radiotherapy. Afterwards, hormonal treatment can be started or can be acted according to the patient’s condition. Stage 3 plan in prostate cancer treatment should be either surgery or radiotherapy.
According to the researches, it has been determined that a 5-month chemotherapy after surgery and radiotherapy prolongs the life expectancy in prostate cancer. In patients with a PSA above 40, lymph node involvement or Gleason score above 7, chemotherapy should be considered in addition to hormonal treatment after surgery or radiotherapy. In stage 4, the main treatment of prostate cancer should be hormonal therapy. With hormonal treatment, the ovaries of the patient can be surgically removed or the male hormone can be blocked with injections every 1-3 months. After 2010, there have been many innovations in the treatment of stage 4 prostate cancer. Some drugs and chemotherapy have been shown to significantly increase life expectancy in stage 4. In addition, some agents have been developed that are used when traditional hormone blockers do not work. Although prostate cancer vaccine has been tried, it has not shown the expected effect. Radiotherapeutic agents have been shown to be effective only for patients with bone metastases. In addition, treatments with PSMA combined with radioactive Lutetium in prostate cancer are also possible in our country.
DA VINCI ROBOTIC SURGERY
Prostate cancer surgeries performed with the da Vinci Robotic System are especially important for the patient not to experience loss of sexual function after surgery. For the experienced laparoscopic surgeon, the arms of the da Vinci robot, which provides a 3D, “high definition” quality image with 10-20 times magnification, can remove the cancerous prostate and provide a radical treatment by easily protecting the nerves and vessels in the body and even in the most difficult place.
FREQUENTLY ASKED QUESTIONS ABOUT PROSTATE CANCER
What is the prostate gland?
The prostate gland is part of the male reproductive system. The gland makes fluid that mixes with semen during ejaculation. This fluid helps to preserve the sperm.
Who has a higher risk of prostate cancer?
Men over 55 are more susceptible to the disease. The risk of developing prostate cancer increases with age. In fact, about 60 per cent of prostate cancers occur in men over the age of 65. Other risk factors for prostate cancer include:
- Ethnicity (black men have the highest risk)
- Family history of prostate cancer
- Smoking
- Obesity
What are the complications of prostate cancer?
Some aggressive cancers spread rapidly outside the prostate (metastasise). Prostate cancer most often spreads to the bones and lymph nodes. It can also develop in the liver, brain, lungs and other organs.
What is a prostate ultrasound examination?
Ultrasonography is a diagnostic method used to examine internal organs using sound waves with a frequency too high for the human ear to hear. The device consists of a console containing computer and electronic elements, a video display screen and parts called probes used to scan the body. Ultrasonographic examination used to detect benign and malignant growths of the prostate is called Trans Abdominal Ultrasound (TAUS) if it is performed through the anterior abdominal wall and Trans Rectal Ultrasound (TRUS) if it is performed through the anus.
How is Prostate Ultrasonography Examination Performed?
In the TAUS procedure, the ultrasound probe is placed on the abdomen and the prostate is visualised with the strengthening effect of ultrasonography waves. The bladder must be full for this procedure. It is sufficient to drink 1.5 litres (approximately 6 glasses) of water 1.5 – 2 hours before the procedure. In the TRUS procedure, the prostate is visualised through the anus with a sterile coated special ultrasonography probe. Since bowel cleansing is required for this procedure, it is necessary to drink a laxative after dinner the day before and empty the bladder just before the procedure.
What are the benefits of prostate ultrasonography?
An important advantage of ultrasonography in prostate control is that it does not harm the patient. Other distinct advantages are that it is easy to perform, low cost and does not contain ionising radiation. In the transabdominal ultrasound procedure, the size, weight and anatomical shape of the prostate are determined. In the transrectal ultrasound procedure, in addition to these, the tissue details of the prostate are also evaluated. During this procedure, colour Doppler and Power Doppler methods can be used to evaluate the blood supply in the areas where cancer is suspected, and biopsy can be performed in the same session with preliminary preparation. Ultrasonography examination can provide the physician with detailed information about the patient’s prostate, help in reaching the correct diagnosis and planning the appropriate treatment.
What measures can be taken against prostate cancer?
From healthy and proper nutrition to lifestyle, there are effective measures that can reduce the risk of prostate cancer. Lycopene, which gives red fruits such as tomato, watermelon, rosehip, pink grapefruit and papaya their colour, is a powerful antioxidant. There are many studies suggesting that isoflavone, which has anti-inflammatory properties, provides protection against prostate cancer. Consuming pomegranate, especially pomegranate juice, has protective properties against prostate cancer while keeping PSA levels under control. Turmeric is a great protector against prostate enlargement and prostate cancer due to its anti-inflammatory properties as well as the curcumin substance it contains. On the other hand, there are various studies that show that regular physical activities also reduce the likelihood of developing prostate cancer.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS RECTAL CANCER?

Rectal cancer is a disease in which cancerous or malignant cells form in the rectal tissues. Rectal cancer is usually caused by polyps in the lining of the rectum. Cancer of the rectum and colon is often referred to as “colorectal cancer”.
WHAT ARE THE SYMPTOMS OF RECTAL CANCER?
Symptoms of rectal cancer can occur in many different ways. However, many rectal cancers are detected in routine screening without symptoms. Symptoms of rectal cancer generally include the following.
- Bleeding in the anus or blood in the stool is one of the most common symptoms of rectal cancer. Almost 8 out of 10 patients experience bleeding symptoms.
- Mucus in faeces
- Changes in bowel movements such as constipation, diarrhoea, excessive amounts of gas may be the first sign of rectal cancer.
- In addition to changes in bowel movements, the feeling that the bowel is empty or the inability to defecate adequately despite frequent visits to the toilet are also among the symptoms of rectal cancer.
- Painful bowel movements
- Unnoticed bleeding in the stool can lead to anaemia. Shortness of breath, dizziness and rapid heartbeat due to anaemia should be taken seriously as symptoms of rectal cancer.
- Intestinal obstruction may occur as a result of the tumour growing and blocking the exit route. Intestinal obstruction can cause severe pain and cramps in the abdomen.
- The growth of the tumour may cause changes in stool size. Pencil-thin stools can be a sign of rectal cancer.
- Unexplained weight loss not related to diet or exercise is among the first symptoms of rectal cancer.
WHAT CAUSES RECTAL CANCER?
The cause of rectal cancer is not known for certain. However, there are many risk factors that cause rectal cancer.
- The majority of rectal cancers occur in advanced age
- Alcohol and smoking increase the risk of rectal cancer.
- A high-fat diet of animal origin can cause rectal cancer.
- A history of colorectal cancer or polyps may cause rectal cancer.
- Chronic inflammatory diseases of the colon and rectum such as ulcerative colitis and Crohn’s disease increase the risk of rectal cancer.
- Genetic syndromes such as nonhereditary colorectal cancer without polyps (Lynch) and familial adenomatous polyposis (FAP) are among the causes of rectal cancer.
- Sedentary life and obesity
- Receiving radiotherapy treatment for cancer treatment, especially in the abdomen, can cause rectal and colon cancer.
- Diabetes (diabetes)
- The presence of colon and rectal cancer in the family, especially in first-degree relatives, is an important cause of rectal cancer.
HOW IS RECTAL CANCER DIAGNOSED?
- Routine screening programmes should be implemented in order to detect rectal cancer early. Starting routine screening at the age of 50 in people without any risk factors is vital for early diagnosis of rectal cancer. In people with risk factors, the screening age may start earlier. Rectal cancer is usually diagnosed in controls performed after rectal bleeding or iron deficiency, which are symptoms of rectal cancer.
- The most commonly used method for screening programmes and diagnosis is colonoscopy. During colonoscopy, it is usually possible to remove small tissue samples from suspicious areas. Laboratory analysis of tissue samples removed for biopsy helps in the diagnosis of rectal cancer.
TREATMENT OF RECTAL CANCER
Treatment is planned after the stages and grade of rectal cancer are determined. In the treatment of rectal cancer; planning is made according to the stage and grade of cancer, the location and size of the tumour in the rectum, the age and general health status of the patient.
Chemotherapy and Radiotherapy treatment of rectal cancer
Chemotherapy treatment for rectal cancer usually consists of two or more drugs that target cancer cells. In rectal cancer, chemotherapy and radiotherapy can be used before or after surgery. Surgery may be the only necessary step in the treatment of rectal cancer stage 1. In stage 1 rectal cancer, the risk of recurrence after surgery is low and therefore chemotherapy is generally not recommended. In stages 2 and 3 of rectal cancer, chemotherapy and radiotherapy treatment is applied after surgery to prevent recurrence of the cancer. In patients with Stage 2 rectal cancer and Stage 3 rectal cancer, chemotherapy and radiotherapy treatment can be applied to shrink the tumour before surgery.
Rectum cancer surgery
Surgery is one of the most frequently used methods in the treatment of rectal cancer. Rectal cancer surgery is planned according to the location and size of the tumour.
Rectal cancer surgery can be analysed in 2 groups: rectum-sparing rectum surgery and rectum surgery requiring rectal loss.
In rectal cancer surgery;
- End colostomy
- Coloanal anastomosis
- Low anterior resection
- Local excision – Local or Transanal Excision – Transanal Endoscopic Microsurgery
- Intraoperative radiation therapy (IORT).
- Abdominoperineal Excision (APR) – Extra-Levator Abdominoperineal Excision
- Polypectomy
- Radiofrequency ablation
- Cryosurgery
Surgical techniques such as minimally invasive surgery can be used
FREQUENTLY ASKED QUESTIONS ABOUT RECTAL CANCER
Who Can Get Rectal Cancer? Is it a Common Cancer?
Rectal cancer is more common in men than in women. With the advancement of endoscopic and radiological examinations, rectal cancer can be diagnosed more easily. With the increase in awareness, there is an increase in incidence rates. Approximately 1 million people in the world are diagnosed with colon and rectal cancer every year. Although there is no exact figure in our country, it is estimated that 30 thousand people are diagnosed with colon and rectal cancer every year. The most common type of rectal cancer is adenocarcinoma, a cancer originating from the mucosa.
At what age is rectal cancer seen?
There is no definite age of onset for rectum and colon cancer. However, rectal cancer is usually seen after the age of 35. The majority of patients are older than 50 years of age.
Which Doctor Should I Go to for Rectal Cancer?
In cases where one or more of the symptoms of rectum and colon cancer are seen, gastroenterology or general surgery department doctors should be consulted without wasting time. Since surgical methods come to the forefront in the treatment procedure of rectum and colon cancer, it is important to choose a specialist doctor in this field. Since the treatment of colorectal cancers requires a multidisciplinary approach by bringing together many medical units such as general surgery, gastroenterology and oncology, it is important to choose hospitals with sufficient medical infrastructure.
Is Rectal Cancer Contagious?
There is no transmission from one person with rectal cancer to another person. There is no evidence that cancer is transmitted by respiration, air, contact or sexual transmission. However, rectal and colon cancer has genetic characteristics. People with rectal and colon cancer in their family are more likely to have colorectal cancer.
What is the difference between rectal cancer and colon cancer?
The symptoms and causes of rectal and colon cancer are very similar. Although rectal and colon cancers are similar in many ways, their treatments are different. The main reason for this is that the rectum sits in a narrow space that is barely separated from other organs and structures in the pelvic cavity
Does Haemorrhoids Cause Rectal Cancer?
Rectal cancer is not associated with haemorrhoids. However, bleeding, especially in the rectal area, and the pain experienced are seen in haemorrhoids as well as in rectal cancer. Many people with colon and rectal cancer also have haemorrhoids.
Patients may delay in consulting a doctor by attributing the problems they experience to haemorrhoids. With the onset of symptoms, it is important to consult a specialist without wasting time for early diagnosis.
Which tests are performed for rectal cancer staging?
After the diagnosis of rectal cancer is made by physical examination of a general surgeon specialised in colorectal cancers and colonoscopy examination, the stage of rectal cancer should be determined.
Rectal cancer staging is important for deciding the most appropriate course of treatment. The following examinations can be applied during the staging of rectal cancer.
- Rectal Examination: It is a finger examination using a slippery glove placed in the anus to feel the cancer in the rectum wall. In cases where the tumour is far from the anus, rectal cancer may not be detected in this examination. If an abnormality is detected by digital rectal examination, an endoscopy is performed to further evaluate the cancer.
- Flexible sigmoidoscopy: As in the colonoscopy method, a flexible tube with a camera on it is inserted through the anus and into the rectum. This examination can give an idea for both the diagnosis of rectal cancer and the stage of rectal cancer.
- Rigid sigmoidoscopy: It is the insertion of a rigid optical scope through the anus and into the rectum. Rigid sigmoidoscopy is usually performed by a gastroenterologist or general surgeon. The advantage of rigid sigmoidoscopy is that a more precise measurement of the distance of the tumour to the anus can be made.
- Complete blood count: Determining whether the number of red blood cells in the blood is low is important to show whether the tumour is causing blood loss. A high level of white blood cells may be a sign of infection, with the risk of the tumour growing through the wall of the rectum.
- Tumour marker tests: Cancer can sometimes produce substances called tumour markers in the blood. Having more tumour markers in the blood than normal can be a sign of rectal cancer. Carcinoembryonic antigen and carbohydrate antigen can be checked for rectal cancer. Carcinoembryonic antigen (CEA) is normally found at very low levels in the blood of adults. CEA can be increased in certain types of cancer and in non-cancerous (benign) conditions.
- Computed tomography (CT): Computerised tomography can be used to check whether colorectal cancer has spread to the lymph nodes in the chest, abdomen and pelvis or to organs such as lung and liver. The distance of the tumour from the anus can also be determined by computer tomography and rectal cancer staging can be performed.
- Magnetic Resonance (MR): A detailed image of the muscles, organs and other tissues surrounding the tumour in the rectum can be provided. In addition, the lymph nodes next to the rectum and the different layers of tissue in the rectal wall can be visualised with magnetic resonance.
- Chest X-ray: X-rays can be used to determine whether rectal cancer has metastasised to the lung.
- Endoscopic Ultrasound (EUS): It is based on the combination of endoscopy and ultrasonography. EUS shows the wall layers in the digestive tract in detail. It facilitates the diagnosis of diseases in the digestive tract or in organs neighbouring the digestive tract.
- PET scan (positron emission tomography scan) : It is a procedure for finding malignant tumour cells in the body. A small amount of radioactive glucose is injected into a vein. The PET scanner rotates around the body and shows where glucose is used in the body. Malignant tumour cells appear brighter in the picture because they are more active and take up more glucose than normal cells.
- Cell and tissue tests: Cell and tissue tests are to find the type of colon or rectal cancer. KRAS is a gene that is mutated in some colorectal cancer cells. KRAS testing is usually performed in colorectal tumours that have metastasised. It is important in terms of the appropriateness of targeted drug use. MSI test can also be performed to determine whether the tumour is caused by Lynch syndrome
Rectum Cancer Stages
The grade of rectal cancer and the stage of rectal cancer are important for the treatment. Rectal cancer grading is about how cancer cells look compared to normal and healthy cells. Knowing the grade of rectal cancer can give an idea of how fast the cancer can grow and how likely it is to metastasise, that is, spread.
In low-grade rectal cancer, the cells are abnormal but look like normal cells. Low-grade rectal cancer tends to grow slowly and is less likely to metastasise. High-grade rectal cancer has more undifferentiated cancer cells. High-grade rectal cancer, whose cells do not look like normal cells, tends to grow rapidly and is more likely to metastasise than low-grade cancers.
Staging of rectal cancer varies according to the information obtained from the examinations, which parts of the rectum have cancer, the size of the tumour, whether the cancer has spread from where it first started. Staging is important for planning the treatment of rectal cancer.
Staging of rectal cancer;
- How deep the tumour is in the wall of the rectum
- Whether there is cancer in the lymph
- It is assessed whether rectal cancer has metastasised to other organs such as the lung or liver.
Rectal cancer stages are evaluated in 5 groups.
- Rectal Cancer Stage 0: Cancer cells are found only in the inner lining of the colon or rectum called mucosa. Cancer cells have not passed the muscle layer of the mucosa.
- Rectal Cancer Stage 1: The tumour has spread to the layer of connective tissue surrounding the mucosa or the thick outer muscle layer of the rectum.
- Rectum Cancer Stage 2: Stage 2 of rectal cancer is handled in three stages.
- Rectal Cancer 2 Stage- A; The cancer has reached the outermost layer of the rectum wall and has not spread to the surrounding organs. There is no metastasis to lymph and distant organs.
- Rectal Cancer 2 Stage- B: Cancer has invaded all layers of the rectal wall but has not spread to surrounding organs or tissues There is no metastasis to lymph or distant organs.
- Rectal Cancer 2 Stage- C; The cancer has spread beyond the rectum wall. It has grown towards nearby organs or tissues. There is no metastasis in lymph and distant organs.
- Rectum Cancer Stage 3: Cancer has spread to nearby lymph. Stage 3 of rectum cancer is handled in 3 parts depending on where the tumour grows and how many lymph nodes it has spread to.
- Rectum Cancer Stage 4: In Stage 4 of rectal cancer, metastasis to organs such as the liver or lungs has occurred. Cancer can be in only 1 organ or distant lymph. It is handled in 3 stages.
- Rectal Cancer Stage 4-A: The cancer has spread to an area or organ that is not close to the rectum, such as the liver, lungs, ovary or a distant lymph.
- Rectal Cancer Stage-B: The cancer has spread to more than one area or organ not near the rectum, such as the liver, lung, ovary, or a distant lymph node.
- Rectal Cancer Stage-C: The cancer has spread to the tissue lining the abdominal wall and may have spread to other areas or organs.
What are Rectal Cancer Metastases?
When cancer spreads to another part of the body, it is called metastasis. The cells of rectal cancer leave the place where they started (the primary tumour) and can metastasise to different parts of the body through the lymph system or blood.
The answer to the question of which organs rectal cancer spreads to includes the following;
- Metastasis of rectal cancer is most commonly experienced in nearby lymph
- Rectal cancer can spread to the peritoneum.
- Metastasis may occur in tissues close to the abdomen or pelvis.
- It can be seen in distant lymph.
- Rectal cancer can metastasise to the kidney and adrenal gland.
- Rectal cancer liver metastasis is usually seen in stage 4.
- Lung metastasis of rectum cancer is usually seen in stage 4.
- Rectum cancer metastasis can be seen in bones and brain.
What is the Life Span of Rectal Cancer?
One of the most curious issues for rectal cancer patients is the question “How long does rectal cancer live?”. The life expectancy of rectal cancer depends on many factors such as cancer grade, stage, carcinoembryonic antigen (CEA) levels, general health status of the patient, the treatment method chosen, and the patient’s response to treatment. The answer to a question such as “How long does rectal cancer survive?” is not definite and varies from patient to patient.
Rectal cancer survival statistics are very general estimates and should be interpreted very carefully.
According to general statistics in the world, 5-year survival rates are as follows
Rectal Cancer Stage 1 5-year survival 80- 88
Rectal Cancer Stage 2 5-year survival 60% – 81
Rectal Cancer Stage 3 5-year survival %40-75
Rectal cancer Stage 4 (last stage of rectal cancer) 5-year survival %8-13
How should follow-up be after rectal cancer treatment?
Some of the tests performed to diagnose rectal cancer or to find the stage of rectal cancer may be repeated after treatment. The decision about whether to continue or change treatment may be based on the results of these tests.
After treatment for rectal cancer, tests such as measuring the amount of carcinoembryonic antigen, colonoscopy, virtual colonoscopy can be repeated to check whether the cancer has recurred.
Can Rectal Cancer be Prevented?
Rectal cancer is a preventable cancer like colon cancer. Rectal cancer can develop from benign rectal polyps in the rectal wall. Detection and removal of these polyps by colonoscopy reduces the risk of rectal cancer. Considering the family history, screening for rectal cancer after the age of 45-50 is of vital importance. The most accurate and effective screening test is colonoscopy.
In addition to screening controls, there are many scientific studies showing that diet is also associated with rectal cancer. Consumption of low-fat foods such as whole grains high in fibre, fruits, vegetables and nuts can reduce the risk of developing rectal cancer.
To prevent rectal cancer in general;
- Routine colorectal screening should not be neglected
- Weight control should be ensured
- An active life should be preferred. Exercise and sports should be done regularly
- Vegetables such as salad greens, tomatoes, onions, broccoli, aubergines, carrots, garlic and fruits such as melons, apples, pears, oranges and bananas should be consumed frequently. In addition, foods such as oats, black rice, barley, wild rice, lentils, beans should be added to the diet.
- Meat, processed meat, fast food style nutrition should be avoided.
- Alcohol and smoking should be quit.
Rectal Cancer Nutrition
A balanced diet before, during or after treatment for rectal cancer can help you feel well and maintain your strength and speed up recovery.
- Ensure your weight control. Treatments such as chemotherapy, radiotherapy and rectal cancer surgery can often cause unwanted weight loss. It is important to prevent excessive weight loss during treatment, as poor and unbalanced nutrition can reduce the body’s ability to fight infection.
- Eat small, frequent meals throughout the day. Eating frequent small meals ensures that your body gets enough calories, protein and nutrients to tolerate the treatment. Small meals can also help reduce treatment-related side effects such as nausea.
- Choose protein-rich foods. Protein helps the body repair cells and tissues. It also helps the immune system recover from illness. Include a source of lean protein at all meals and snacks. Good sources of lean protein are:
- Lean meat such as chicken, fish or turkey
- Eggs
- Low-fat milk or dairy products such as milk, yoghurt and cheese
- Nuts
- Beans
- Soya foods
- Include whole grain foods in your diet. Whole grain foods provide a good source of carbohydrates and fibre, which help keep your energy levels high.
- Good sources of whole grain foods include:
- Oatmeal
- Wholemeal bread
- Brown rice
- Whole grain pasta
- Eat a variety of fruit and vegetables every day. Fruit and vegetables provide the body with antioxidants, which can help fight cancer. Choose a variety of colourful fruits and vegetables to get the most benefit.
- Choose healthy sources of fat. Avoid fried, greasy and fatty foods
- Limit sweets.
- Remember to drink water. Drinking enough fluids during cancer treatment is important to prevent dehydration.
- Pay attention to changes in bowel habits. Colorectal cancer and its treatments can often cause changes in bowel habits such as diarrhoea, constipation, bloating and gas. Share any changes in your bowel habits with your doctor.
- Talk to your healthcare team before taking any vitamins or supplements.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS GALLBLADDER CANCER?
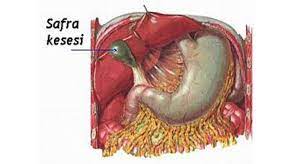
Gallbladder cancers are malignant tumours that originate from the wall of the gallbladder. Polyps in the gallbladder, gallbladder inflammation, obesity, certain chemicals such as nitrosamine can be the main causes of gallbladder cancer. Gallbladder cancer, which can be diagnosed much more easily in people with gallstones, is caught in the advanced stage of cancer when it starts to give symptoms for different reasons.
SYMPTOMS OF GALLBLADDER CANCER
Although gallbladder cancer is mostly seen in people aged 60 and over, it is a very insidious type of cancer. Since the patient can continue his/her life even if the gallbladder does not fulfil its function, it may not give many symptoms or its symptoms may indicate different diseases.
Symptoms of gallbladder cancers often include;
- Jaundice,
- Abdominal pain,
- Problems with digestion,
- Nausea, vomiting,
- Food intolerance,
- Slimming,
- Dark urine and white stools are observed.
The most important symptoms of advanced gallbladder cancer are jaundice, a feeling of a large mass in the abdomen and in the area where the gallbladder is located, and pain. Symptoms of gallbladder cancer usually make themselves felt 3-6 months before the onset of the disease. In some patients, gallbladder cancer may occur after 1 year of gallbladder-related disorders. Jaundice without any symptoms is also considered a sign of gallbladder cancer alone. 75% of gallbladder cancer is seen in women and 80% of these patients have stones in the gallbladder. If the stones are larger than 3 cm, the risk of gallbladder cancer increases. If any of the symptoms of gallbladder cancer are noticed, it is necessary to consult the General Surgery department of a fully equipped hospital as soon as possible.
RISK FACTORS FOR GALLBLADDER CANCER
Risk factors for gallbladder cancer include gallbladder polyps and gallbladder disease called “porcelain gallbladder”. Obesity, unhealthy diet and exposure to chemicals such as nitrosamines are also recognised as important risk factors. In addition, recurrent infections in the biliary tract are also recognised as one of the factors leading to gallbladder cancer.
Infections are accompanied by jaundice, high fever and pain complaints occur, and the patient is admitted to hospital when the attacks are severe. Although its relationship with cancer has not been conclusively proven, it is recommended that patients with stones in the gallbladder should not interrupt their controls and have regular follow-up.
CAN GALLSTONES CAUSE CANCER?
The presence of gallstones in more than 90% of patients with gallbladder cancer has been proven by studies. However, although this situation has led to the view that cancer may be affected by gallstones, the view that “gallstones cause cancer” has not gained certainty. Only the close association of gallstones and cancer has been a cause of scepticism for years. Cancer ranks last among the diseases caused by gallstones. Gallstones cause infection, biliary obstruction, jaundice and pancreatitis before cancer.
DIAGNOSIS AND STAGES OF GALLBLADDER CANCER
It is very important to diagnose gallbladder cancer at an early stage. Imaging methods such as ultrasound, tomography and MRI are used according to the symptoms seen in the patient. As with many types of cancer, the definitive diagnosis of gallbladder cancer is made by biopsy after advanced imaging techniques. Diagnostic methods are determined according to the patient’s health status, age, disease symptoms and previous test results.
These methods are used for the diagnosis of gallbladder cancer;
Blood tests: The diagnosis of gallbladder cancer requires measuring abnormal levels of bilirubin and other substances in the blood.
Ultrasound: It is the use of sound waves to check for tumours in the body. Cancerous tissues present different sound waves than normal tissues.
Computed tomography (CT) scan: A CT scan provides a three-dimensional image of the body. It is checked for tumours or any abnormalities. It also allows the size of the tumour to be understood.
Magnetic resonance imaging (MRI): With MRI, it is possible to find out whether the cancer has spread outside the gallbladder and the size of the tumour.
Biopsy: A definitive diagnosis can be made with a biopsy performed by examining a small tissue sample under a microscope. Biopsy can be performed by minimally invasive surgical technique or by fine needle or thick needle aspiration. Computerised tomography and endoscopy can also be used.
Endoscopic retrograde cholangiopancreatography (ERCP): The inside of the body is visualised with an endoscope inserted down the patient’s oesophagus into the stomach and small intestine. A small tube or catheter is passed through the endoscope and into the bile ducts. It is more commonly used for the diagnosis of bile duct cancer. It is also used when gallbladder cancer has spread and blocked the bile ducts.
Percutaneous cholangiography: In this imaging method, a thin needle with a dye to create a clear image on X-rays is inserted through the skin into the gallbladder area. X-rays are used to determine whether there is a tumour in the gallbladder.
Laparoscopy: To look at the gallbladder and other internal organs, an endoscope is inserted through a small incision in the abdomen and imaging is performed.
Endoscopic ultrasonography (Endosonography): A more extensive and specialised endoscope can reach the stomach and intestines starting from the mouth under sedation.
Positron emission tomography (PET) scan: PET scanning is a way of creating images of organs and tissues inside the body. This allows us to determine which organs in the body an existing tumour has spread to and to stage the cancer.
The gallbladder stages can be defined as follows;
Stage 1: In-situ carcinoma, the gallbladder tumour is located only intramuscularly.
Stage 2: The tumour involves only the muscular layer of the gallbladder.
Stage 3: All layers of the gallbladder wall are faced with cancerous tumour. Ductus cysticus lymph nodes may or may not be involved.
Stage 4: At this stage, gallbladder cancer has spread to the liver and other neighbouring organs. Bile ducts and other lymph nodes are involved.
GALLBLADDER CANCER TREATMENT
The treatment of gallbladder cancer is based on surgical removal of the tumour. It may also be necessary to remove part of the liver during the treatment, which consists of a large-scale operation. Since gallbladder cancers are usually diagnosed at an advanced stage, patients often have no chance of surgery. However, early diagnosis of cancer ensures successful treatment of gallbladder cancer. Some endoscopic procedures to relieve jaundice and pain, pain treatment, percutaneous drainage (radiological intervention) can be performed in patients with advanced stage disease that cannot be operated. Hot chemotherapy and some recently developed smart drugs can also affect the progression of the tumour.
*Page content is for informative purposes only. Please consult your doctor for diagnosis and treatment.*
WHAT IS TESTICULAR CANCER?

The testicles, part of the male reproductive system, are two oval glands that sit behind the penis in a sac of skin called the scrotum. The testicles produce and store sperm. In addition to this function, they also produce testosterone, which is responsible for the development of facial hair, increased muscle mass as well as sex drive (libido). Sperm formation and testosterone secretion are controlled by the hormones FSH and LH secreted by the pituitary gland.
WHAT IS TESTICULAR CANCER?
Testicular cancer is a tumoral growth that starts in the testicles and can sometimes spread to other parts of the body. Testicular cancer occurs when cancerous (malignant) cells develop in the tissues of one testicle. Testicular cancer is the most common cancer in men aged 20 to 35. The disease can usually be successfully treated. The incidence of testicular cancers in the right testicle is 52.3 percent, while the incidence in the left testicle is 47.7 percent. The development of cancerous cells can occur in both testicles, but this is very rare (2-3 percent).
WHAT ARE THE RISK FACTORS FOR TESTICULAR CANCER?
Risk factors for testicular cancer generally include the following:
Age
Most cases occur between the ages of 15 and 40. Testicular cancer is the most common cancer in men between the ages of 20 and 35.
Race-ethnicity
The risk of developing testicular cancer is 5 times higher in white men than in black men. Worldwide, the risk of developing the disease is higher in America and Europe and lower in Africa and Asia.
Family history of testicular cancer
Family history increases the risk of developing testicular cancer. In fact, if a man in the family has testicular cancer, the likelihood of testicular cancer in a brother and/or son in the same family increases.
Undescended testicle (cryptorchidism)
Men with testicles that do not descend into the scrotum before birth are at high risk. Men who have surgery to correct this condition are still at risk of developing testicular cancer.
Abnormal testicular development
Conditions that cause abnormal development of the testicles may increase the risk of testicular cancer
HIV infection
The risk of testicular cancer is increased in men with HIV infection, especially in patients with AIDS.
History of cancer in the other testicle
About 3 to 4 percent of men who are cured of cancer in one testicle will also have cancer in the other testicle.
Klinefelter syndrome
Klinefelter syndrome is also a factor that increases the risk of testicular cancer.
WHAT ARE THE TYPES OF TESTICULAR CANCER?
About 90 to 95 percent of testicular cancers arise from cells called “germ cells”, which are used to produce sperm. There are two main types of testicular cancer: Seminoma and non-seminoma.
Seminoma tumors
Seminoma tumors have two main characteristics:
- Tends to develop more slowly than non-seminoma tumors
- Although it usually occurs between the ages of 25 and 45, it can also occur at older ages
Non-seminoma tumors (non-seminoma)
The characteristics of non-seminoma tumors are as follows:
- Tends to develop faster than seminoma cancers
- There are four main subtypes: Teratoma, choriocarcinoma, yolk sac tumor and embryonal carcinoma
- It usually occurs in late adolescence and early 30s.
Other tumors
Mixed tumors
Sometimes a testicular cancer may contain a mixture of seminoma cells and non-seminoma cells or a combination of different subtypes of non-seminoma cells (mixed tumors).
Stromal tumors
Stromal tumors form in the cells that make up the supporting (structural) and hormone-producing tissue of the testicles. They are usually benign and are surgically removed.
Note: Some testicular cancers start as a condition called intratubular germ cell neoplasia (ITGCN or IGCN). In this case, the cells are abnormal, but they do not spread outside the area where sperm cells develop. ITGCN is not cancer, but there is about a 50 percent risk that it will develop into testicular cancer within five years. About 5 to 10 percent of people diagnosed with testicular cancer have ITGCN. ITGCN has similar risk factors to testicular cancer. ITGCN is difficult to diagnose because there are no symptoms and it can only be diagnosed by testing a tissue sample.
WHAT ARE THE SIGNS AND SYMPTOMS OF TESTICULAR CANCER?
The first sign of testicular cancer is usually a swollen testicle or a hard lump in the testicle. There is usually no pain in the testicles, but there may be pain or discomfort in the scrotum, the bag-like organ where the testicles are located in men.
Other symptoms of testicular cancer are as follows:
- A pulling sensation or discomfort in the scrotum
- A testicle that appears larger than normal
- Mild pain in the lower abdomen and groin area
- Fluid accumulation in the scrotum (hydrocele)
Other symptoms may also develop, depending on the stage of testicular cancer, including
- Back pain
- Coughing
- Swelling of one or both legs or shortness of breath from a blood clot can be symptoms of testicular cancer. A blood clot in a large vein is called deep venous thrombosis or DVT. A blood clot in an artery in the lung is called a pulmonary embolism. This causes shortness of breath.
- Weight loss
- Infection Infection of the testicle is called orchitis. Infection of the epididymis is called epididymitis. If infection is suspected, the patient may be prescribed antibiotics. If antibiotics do not solve the problem, further tests will be needed, usually for suspected testicular cancer.
- Breast tenderness or enlargement: Although rare, some testicular tumors produce hormones that cause breast tenderness or enlargement of breast tissue, a condition called gynecomastia.
Since diagnosing testicular cancer at an early stage will increase the success rate of treatment, it is necessary to consult a doctor immediately in case of the above symptoms.
HOW IS TESTICULAR CANCER DIAGNOSED?
Physical examination, testicular ultrasound and blood tests are needed for the diagnosis of testicular tumors. In addition to these tests, chest X-rays and tomography are also performed in case the tumor spreads. As with many cancer tumors, delay in diagnosis can be dangerous. A 6-week delay in the diagnosis of testicular cancer increases the risk of death from cancer by 2 times.
If a palpable mass is detected in the testicle, it is assumed to be a tumor and treatment is started accordingly, unless otherwise proven by tests. The diseased testicle should be removed immediately and the necessary pathological examination should be performed to confirm the diagnosis.
The following blood tests will also be performed to measure the levels of tumor marker proteins.
- Alpha-fetoprotein (AFP)
- Beta-human chorionic gonadotropin (beta-hCG)
- Lactic dehydrogenase (LDH)
- Placental alkaline phosphatase
According to the results of all tests (CT scan, MRI scan, chest x-ray) and pathological examination, the stage of the disease and the subtypes that vary according to cell structure are identified. Based on the results, it is determined whether additional treatment such as “chemotherapy” or “radiotherapy” is needed. After surgery, a good follow-up should be done according to the stage and type of the tumor. As with other types of cancer, the chances of success are very high with early diagnosis and appropriate treatment in a short time.
WHAT ARE THE TREATMENT METHODS FOR TESTICULAR CANCER?
The treatment of testicular cancer varies according to the area of spread of cancerous cells, the type of cancer and the general health status of the patients. Stage 1 means that the cancer is found only in the testicle; Stage 2 means that the cancer has spread to lymph nodes in the abdomen or pelvis. Stage 3 testicular cancer means that the cancer has spread beyond the lymph nodes to other parts of the body, such as the lungs. It can be said that surgery is the main treatment method, especially for cancer diagnosed at an early stage. In other words, if the cancer is only in the testicle (stage 1), removal of the testicle (orchidectomy) may be the only treatment required. If the cancer has spread beyond the testicle, the patient may also receive chemotherapy and/or radiotherapy. Testicular cancer can recur or spread to other parts of the body. Follow-up care is therefore important after successful treatment.
Surgery
The main treatment for testicular cancer is an operation to remove the testicle affected by cancer, called orchidectomy. It can be said that surgery is the main treatment for testicular cancer diagnosed early.
After the operation, a team of specialists, including an oncologist, will examine all the results. For example, if the cancer is more advanced, another surgical procedure may be needed to remove lymph nodes in the abdomen.
Chemotherapy
Chemotherapy can often be used to treat testicular cancer if the cancer has spread outside the testicle or has recurred after surgery. Even if the cancer has not spread, the doctor may give the patient a course of chemotherapy if needed. This is to reduce the chance of testicular cancer recurring in the future.
Radiotherapy
Radiotherapy uses radiation to kill cancer cells. Radiotherapy is used to treat seminoma-type testicular cancers because seminomas are very sensitive to radiation. Radiotherapy may be used to prevent the cancer from coming back after surgery or if the cancer has spread beyond the testicle.
FREQUENTLY ASKED QUESTIONS ABOUT TESTICULAR CANCER
What are the stages of testicular cancer?
Stage 1: In stage 1, the tumor is only in the testicle.
Stage 2: In stage 2, the tumor has spread to the abdominal lymph nodes.
Stage 3: In stage 3, the tumor has spread to the abdominal lymph nodes and beyond (most commonly to the lung).
Can I have children after testicular cancer?
After an orchidectomy to remove one testicle, there are usually no problems with infertility or erections. This is because the other testicle produces more sperm and more testosterone hormone to make up for what is missing. However, chemotherapy and radiotherapy can reduce fertility. Fertility can also be affected if both testicles and lymph nodes are removed during treatment.
Can testicular cancer be prevented?
There is no way to prevent testicular cancer, but early detection is important. Men should perform a testicular self-examination (TSE) once a month. If any changes in the testicles are noticed (lumps or nodules, hardness, persistent pain or enlargement or shrinkage of the testicles), a doctor should be consulted immediately.
The best time for testicular self-examination is during or after bathing when the skin of the scrotum is loose.
Both hands should be used to examine each testicle. The index and middle fingers should be placed under the testicle and the thumbs on top of the testicle. The testicles should be gently rotated between the fingers (it is normal for the testicles to be different sizes).
You may notice a cord-like structure above and behind the testicle. This structure is called the epididymis. The epididymis stores and carries sperm and should not be confused with a lump.
Any palpable hardness in the testicle should be checked for a mass or swelling. If a lump is felt, a doctor should be consulted (lumps can be pea-sized or larger and are usually painless).
What is the prognosis (chance of recovery) for men with testicular cancer?
This type of cancer is successfully treated in more than 95 percent of cases. On average, even men with unfavorable risk factors have a 50 percent chance of recovery.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS A NAIL TUMOUR

Nail tumours are called formations that occur under and on the edges of the nail plate. They are tumours that originate from the main cells of the nail called nail matrix and the nail bed where the nail plate extends. Most nail tumours are benign. Some of the nail tumours can be seen more frequently on the hands and some on the feet. They occur especially on the big toes of the feet and hands. Nail tumours that cause serious deformity of the nail should be surgically removed. Benign (benign tumours) and malignant (cancers) tumours can affect the nail and cause changes in the structure (dystrophy) and colour (dicholarisation) of the nail.
Benign nail tumours:
Myxoid tumours
Glamos tumours
Pyogenic granulomas
Onychomatricoma
Malignant nail tumours:
Bowen’s disease
Squamous cell carcinoma
Malignant melanoma
WHAT ARE THE CAUSES OF NAIL TUMOURS
As with other skin cancers, the most important cause of nail tumours is sun rays. Nails should be protected against the harmful effects of sun rays just like the skin. Sun protection creams should also be used for nails. Especially people with sensitive skin should be especially careful.
Other causes of nail tumours include chronic traumas, chemical exposures, radiation treatments, cancer types that suppress the immune system such as lymphoma, leukaemia and drugs that affect the immune system such as chemotherapy and infections (AIDS). Apart from these reasons, the possibility of cancer should be considered in all kinds of chronic wounds and bleeding.
WHAT ARE THE SYMPTOMS OF A NAIL TUMOR?
Nail tumors are especially noticeable when the nail structure deteriorates. Nail tumors can give symptoms as deformities such as cracking, thickening, breaking in the nail structure and shape, masses and swellings under the nail. In malignant tumors, color changes in the nail, swelling under the nail and bleeding can be seen. Black or brown discoloration and spreading around the nail plate, nail bed and nail and non-healing wounds are also among the symptoms of malignant nail tumors.
Nail tumors are often confused with nail fungus. Nail fungus treatment can be applied to nail tumors that cannot be diagnosed correctly. Treatment of a nail tumor, which is considered as nail fungus and treated accordingly, may also be delayed at an early stage.
Early and non-progressed benign or malignant tumors can be easily treated, whereas late detected nail cancer can spread and even spread to internal organs. Late detection of nail tumors can lead to amputation of the finger or joint.
HOW IS NAIL TUMOR DIAGNOSED?
Nail tumors are diagnosed by examination, dermoscopic examination and nail biopsy when necessary. A dermatologist can usually determine whether there is a nail tumor after examination and dermoscopic examination with a dermoscope. In cases where cancer is suspected, nail and under-nail biopsy is performed to confirm the diagnosis and the tumor is surgically removed as soon as possible.
HOW ARE NAIL TUMORS TREATED?
Nail tumors are often treated surgically. The area where the tumor is located is anesthetized with local anesthesia and surgical procedures appropriate for the tumor are performed. Nail tumors can be treated by curettage, burning with electrocautery or radiotherapy. Even if the type of tumors varies, the most successful treatment approach is usually surgical treatment of the tumors.
Myxoid cysts are translucent cysts containing fluid. They can be treated by draining the fluid, but there is a possibility of recurrence. Myxoid cysts can also be treated by surgical removal.
Pyogenic granulomas are slightly raised, red, hemorrhagic masses caused by overgrowth of capillaries. They cause swelling of the surrounding tissues. These tumors tend to bleed easily and can be removed by curettage and electrocautery or surgically. Pyogenic granulomas can sometimes be confused with the amelanotic form of malignant melanoma.
Glomus tumors are composed of cells found in vascular structures called glomus. They can occur in any area where blood vessels pass. They can also occur in the glomus structures of the vessels in the toenails and fingernails. They can be painful depending on the location. Nail swelling and deformity can also be among the symptoms. They are mostly benign but can be difficult to diagnose because of their small size. The treatment is surgical removal.
Onimatricoma tumors are caused by excessive keratin production. It appears as a dark line under the nail and the nail plate thickens. Yellowing of the nail, swelling, longitudinal lines and splinter bleeding are also seen in onychomatricoma tumors. It is treated by surgical removal of the tumor.
In malignant nail cancers, the treatment is to biopsy the tumors and surgically remove the tumor as soon as possible. Further treatment options are evaluated according to the stage of the cancer.
Squamous cell carcinoma is a malignant nail cancer. One of the most important causes is overexposure to ultraviolet rays. It is 2 times more common in men than in women. Apart from nails, it can also occur on the face, hands, arms and legs.
Bowen’s disease is also called intraepidermal squamous cell carcinoma. It is an early form of skin cancer. It usually affects the upper layers of the skin.
Malignant melonoma is a cancer that originates in melanocyte cells that produce the pigment melanin, which gives the skin, hair and eyes their color. People with dark skin are more likely to be affected by this disease. The most common age group is between 40-70 years old.
It is called subungual melanoma if it occurs in the nail bed, ungual melanoma if it occurs under the nail plate, and periungual melanoma if it occurs on the nail plate and skin. Malignant melanoma needs to be surgically removed.
Checking the changes occurring in the nail by a specialist and regular doctor examinations are among the best measures to be taken against nail cancer.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS A TYMUS GLAND?
The thymus gland, which is located behind the area of the body known as the breastbone, in front of the trachea, under the thyroid gland and in front of the heart, is popularly known as the sleepy gland. The thymus gland, a small encapsulated organ resembling the letter H, is pink-gray in color. The thymus gland, which is large at birth, may shrink and become invisible during puberty. It is estimated to weigh about 5 grams in older adults. The thymus gland, which is slightly larger in boys than in girls, can be seen on direct radiographs in children until the age of 3. Although the thymus gland shrinks in size and becomes invisible after puberty, it continues to function for life.
WHAT ARE THE FUNCTIONS OF THE THYMUS GLAND?
The thymus gland, one of the least known organs, has important functions in the body. The thymus gland, an indispensable organ of the immune system, is fully developed at birth. It produces T cells, the most important elements of the immune system. The thymus gland produces antibodies against microorganisms that are foreign to the body. The thymus gland is part of both the lymphatic system, together with the tonsils, adenoids and spleen, and the endocrine system. The thymus gland produces T cells, which help to destroy infected or cancerous cells in the body. The T cells produced by the thymus also help other organs in the immune system to grow properly.
WHAT IS THYMUS GLAND CANCER?
Thymus gland cancer is a rare type of cancer. There are two types of cancer in the thymus gland. The most common type of cancer in the thymus gland is called thymoma cancer. The other type of cancer, which is very rare in the thymus gland, is called thymic carcinoma.
WHAT IS THYMIC CARCINOMA?
Thymic carcinoma tumors are the rarest cancer of the thymus gland. Thymic carcinoma tumors grow faster. They can also spread faster to other parts of the body. Thymic carcinoma tumors are therefore more difficult to treat. It is much rarer to have autoimmune conditions with thymic carcinoma than with thymoma.
WHAT IS A THYMOMA TUMOR?
Thymoma is the most common tumor of the mediastinum itself in adults, arising from the thymus gland. This malignant disease is very rarely seen in childhood. Thymoma tumors are equally common in men and women and usually occur in the 50s and 60s. Since thymoma tumors grow slowly, the patient’s survival rate is higher than other types of cancer.
HOW ARE THYMOMA TUMORS DIAGNOSED?
Since thymoma tumors often progress without any symptoms, they are usually discovered by chance during tests for another disease. Unless the growth in the thymus gland is very large, it is not visible on a chest X-ray. When the size and shape of the thymus gland is noticed on CT, MRI or PET/CT taken for other reasons, a biopsy is performed and the diagnosis is made. Biopsies are performed by fine needle aspiration biopsy, mediastinotomy and VATS (video-mediated thoracoscopic surgery). Since fine needle aspiration biopsy has a lower accuracy rate, VATS is the most commonly used method.
WHAT ARE THE STAGES OF THYMOMA TUMORS?
There are 4 stages of thymoma tumor.
- Thymoma tumor stage 1: In stage 1, the thymoma tumor is still in the capsule.
- Thymoma tumor Stage 2: In the second stage, the thymoma tumor has spread to the capsule and progressed to the surrounding fatty tissues olabilir.
- Thymoma tumor Stage 3: In the third stage, the thymoma tumor may have reached the surrounding tissues outside the capsule, the trachea, lung and heart.
- Stage 4: In stage 4, thymoma tumors can spread to the pleura and other distant organs.
WHAT IS THE TREATMENT OF THYMOMA TUMORS?
The treatment of a thymoma tumor depends on its stage. Thymoma tumors diagnosed at early stages are treated only with surgical methods. The lesion is removed by thoracoscopic or open surgery. In more advanced stages of thymoma tumors, chemotherapy or chemoradiotherapy can be combined with surgical treatment. Thymomas that spread to distant organs are not operated.
FREQUENTLY ASKED QUESTIONS ABOUT THYMUS GLAND CANCER
What causes thymoma tumors?
The known causes of thymoma tumors are not yet fully known. In some studies, it has been determined that radiotherapy and early infection with the EBV virus may pose a risk for thymoma tumors, whose cause and potential risk factors are unknown. Studies are being carried out to clarify whether thymoma tumors are a genetic disease, that is, the relationship between thymoma and chromosomes.
What symptoms do thymoma tumors cause?
Thymoma tumors usually do not cause any complaints or symptoms in the majority of patients. However, in 30 to 35% of the patients, it manifests itself with the following symptoms:
- Cough
- Chest pain
- Hoarseness
The most common paraneoplastic syndrome associated with thymoma is “myasthenia gravis”. Paraneoplastic syndromes are effects that are not caused directly by the tumor itself, but by hormones or substances released from the tumor. Myasthenia gravis accompanies 30 to 50% of thymoma tumors.
What is myasthenia gravis?
Myasthenia gravis is a disease of the nervous-muscular system characterized by rapid fatigue of voluntary muscles. The most important symptom is muscle weakness that increases with fatigue and disappears at rest. Patients usually feel well when they wake up in the morning. However, their general condition gradually worsens during the day. The disease may also present as a drooping eyelid. Symptoms are more common around the face, eyes and mouth, as well as difficulty with the tongue, chewing and swallowing muscles.
Is thymus gland cancer a fatal disease?
Thymoma tumors, which are cancers of the thymus gland, can be fatal if left untreated. However, since thymoma tumor is a slow-growing tumor, the patient’s survival time is longer than other types of cancer. Especially when it is operated in the early stages, the patient’s survival time is very long.
Which department and doctor performs the diagnosis and treatment of thymus gland cancer?
Diagnosis and treatment of thymus gland cancer is performed by thoracic surgery specialists in the thoracic surgery department of hospitals.
Is thymus gland cancer a genetic disease?
The exact cause of thymus gland cancer is not yet known. However, it is thought that radiotherapy and people infected with the EBV virus at an early age have higher risk factors. It is being investigated whether thymus gland tumors are a genetic disease.
At what age is thymus gland cancer more common?
Cancer of the thymus gland, especially thymoma tumors, is too rare to be seen in childhood. Thymoma tumors are more common in the 50s and 60s.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS THYROID?
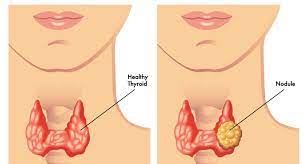
Thyroid is popularly known as a disease. But in fact, the thyroid is a butterfly-shaped organ in front of the trachea just below the area known as Adam’s apple in the throat. The thyroid is responsible for producing many hormones that govern vital functions in the body.
WHAT ARE THYROID NODULES?
The thyroid gland, or thyroid tissue, is a solid or liquid normal structure that can occur in different sizes. The majority of thyroid nodules are not cancerous and can grow without any symptoms. They can be detected incidentally during routine health checks or during an examination. However, some thyroid nodules can grow large enough to be visible and cause different complaints.
WHAT IS THYROID CANCER?
Thyroid cancer is a thyroid gland tumor that occurs when normal thyroid cells in the thyroid gland turn into abnormal cells and grow out of control.
WHAT CAUSES THYROID CANCER?
Thyroid cancers are tumors originating from thyroid nodules. A family history of thyroid cancer, a history of radiation to the neck for another reason and various mutations at the cellular level can cause cancer development from thyroid nodules.
WHAT ARE THE RISK FACTORS FOR THYROID CANCER?
Thyroid cancer risk factors can be listed as follows.
- Thyroid cancers are more common in women than in men. The reason for the higher incidence of thyroid cancer in women is not known exactly, but it is thought to be related to the hormone estrogen.
- Radiotherapy, especially in the head and neck region, can increase the risk of thyroid cancer.
- Genetic factors can increase the risk of thyroid cancer.
WHAT ARE THE SYMPTOMS OF THYROID CANCER?
The most common symptom of thyroid cancer is a feeling of enlargement and swelling in the anterior part of the neck where the thyroid gland is located. In some cases, compression symptoms such as a feeling of getting stuck while swallowing, difficulty swallowing, difficulty breathing, coughing and hoarseness may also develop. Sometimes it can be detected incidentally during a doctor’s palpation or imaging tests performed for another reason without causing any symptoms. Symptoms of thyroid cancer can be listed as follows:
- Growth in the area of the thyroid gland
- Swelling
- Difficulty breathing
- Cough
- Hoarseness
HOW IS THYROID CANCER (GOITER) DIAGNOSED?
The most important examination method in the diagnosis of thyroid cancer is ultrasonography of the thyroid gland. If a thyroid nodule is detected on ultrasonography and the nodule is suspicious for cancer, a fine needle aspiration biopsy is performed. Thyroid fine needle aspiration biopsy is the gold standard method for diagnosing thyroid cancer worldwide. If the sample obtained as a result of the biopsy is suspicious for thyroid cancer as a result of the evaluation of the cytology specialist, the definitive diagnosis is made by the examination of the thyroid tissue removed by surgery by the pathology specialist.
WHAT ARE THE TREATMENT METHODS FOR GOITER CANCER?
The primary treatment of thyroid cancer is surgical removal of the entire thyroid gland or the affected half. If the disease has spread to the lymph nodes in the neck, these should also be surgically removed. After surgery, some types of thyroid cancer require an additional treatment called radioactive iodine therapy (atom therapy). The decision on the need for this treatment is made by the attending physician based on the pathology results and the risk of recurrence. It is usually necessary to stop thyroid medication and follow a special diet for a certain period of time before the treatment. The treatment is given in a radiation-proof environment due to the possibility of radiation emission and radiation precautions must be taken for a period of time after the treatment to prevent those around them from being affected. After thyroid surgery, oral thyroid hormone therapy is given for life, both to meet the body’s need for thyroid hormone and to prevent recurrence of the disease. Apart from these, other treatments such as radiotherapy and chemotherapy are rarely needed in thyroid cancer follow-up.
FREQUENTLY ASKED QUESTIONS ABOUT GOITER CANCER
What is the prevalence of thyroid cancer in men and women?
Approximately 5 percent of all thyroid nodules develop thyroid cancer. It is 4 times more common in women than in men.
How should follow-up be in thyroid cancers?
Thyroid cancer patients should be followed up regularly. In addition to physical examination, blood tests, neck ultrasonography, nuclear screening tests and other imaging methods may be required in some cases. The frequency of follow-ups and the tests to be performed should be determined by the physician performing the follow-up.
Is it possible to prevent factors that can cause thyroid cancer?
As with all cancers, people should adopt a healthy diet and an active lifestyle. In addition, necessary precautions should be taken to protect the neck area from radiation exposure.
How should nutrition be during thyroid cancer?
In thyroid cancer patients, if radioactive iodine treatment is planned after surgery, iodine-poor diet is recommended. However, there is no special dietary recommendation other than a healthy diet that applies to everyone, unless otherwise advised by the physician in the subsequent follow-ups.
When should people with a family history of thyroid cancer have their first check-up?
They should be evaluated by an endocrinologist as soon as possible and the necessary tests should be planned.
Is thyroid cancer fatal?
Although there are different types of thyroid cancer, most of them are papillary thyroid cancer. Papillary thyroid cancer progresses very slowly. Although it often spreads to the lymph nodes in the neck, the disease responds very well to treatment. Thyroid cancer has a very high survival rate when treated appropriately.
Does thyroid cancer spread?
Thyroid cancer can develop within the thyroid tissue or spread to nearby tissues and lymph nodes in the neck. Different types of thyroid cancer, such as follicular thyroid cancer, can spread to the lungs and bones.
Is thyroid cancer completely cured?
Thyroid cancer can be completely cured with early diagnosis and appropriate treatment. However, thyroid cancers can also recur.
Is every thyroid cancer?
The majority of thyroid nodules are benign. The majority of thyroid nodules are cysts filled with a liquid or colloid form of thyroid hormone. Solid nodules are more likely to be cancerous.
How many hours does thyroid cancer surgery take?
The duration of thyroid cancer surgery may vary depending on the type and extent of thyroid cancer and the surgical method to be applied. In general, thyroid cancer surgery can take between 2-3 hours.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS URETHRA?
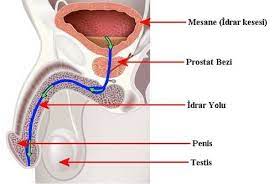
The urethra is a hollow tube that drains urine stored in the bladder out of the body. The urethra is 8 inches long in men and runs from the bladder through the prostate to the tip of the penis. In women, the urethra is 1.5 inches long and is located just above the vagina.
WHAT IS URETHRA CANCER?
Urethral cancer is a type of cancer that develops in the urethra. It is caused by cancerous (malignant) cells in the tissues lining the urethra, a narrow tube that carries urine from the bladder to outside the body. Urethral cancer is the rarest cancer among all urologic cancers. The risk of developing urethral cancer, which is more common in men than women, is higher in people over the age of 60 and in people with a history of bladder cancer. In addition, frequent urinary tract infections and some sexually transmitted diseases such as HPV (human papilloma virus) also increase the risk of urethral cancer by causing chronic inflammation in the urethra. Urethral cancer, which can progress insidiously without any symptoms at first, manifests itself with blood in the urine, frequent, weak or intermittent urine, discharge from the urethra or lymph nodes developing around the urethra.
WHAT ARE THE CAUSES OF URETHRAL CANCER?
As with many types of cancer, the causes of urethral cancer are not yet known for certain. It is known that urethral cancer occurs when healthy cells start to grow uncontrollably and these cells gather together to form a tumor. However, it is not yet known why these cells grow rapidly and cause urethral cancer. Long-term research on urethral cancer patients suggests that these causes increase the risk of cancer:
- People over 60 are more at risk of urethral cancer than younger people.
- Patients with a history of bladder cancer have a high risk of urethral cancer. In addition, urethral cancer may develop later even if the bladder is removed in patients who have been treated for bladder cancer.
- Sexually transmitted diseases such as HPV (human papillomavirus) can increase the risk of urethral cancer.
- People with frequent urinary tract infections have a higher risk of urethral cancer.
- Chronic inflammation of the urethra can cause urethral cancer.
- Stenosis in the urethra can cause chronic swelling and inflammation in men, which can increase the risk of urethral cancer.
- A mass in the urethra can increase the risks of urethral cancer in women.
- The risk of urethral cancer in black people is twice as high as in Caucasians.
WHAT ARE THE SYMPTOMS OF URETHRAL CANCER?
Urethral cancer is a disease that progresses without symptoms at first. This is because the cancer tumors are small. Urethral cancer can cause these symptoms in the patient as the tumors grow:
- Blood in the urine
- Discharge or bleeding from the urethra
- Frequent urination and urge to urinate without passing all the urine
- Having trouble urinating
- Pain when urinating or low flow
- Urinary incontinence
- Enlarged lymph nodes in the groin
- A lump or growth in the area between the genitals and anus
Most of the above symptoms may also be caused by another disease. However, these symptoms should not be neglected and an experienced urologist should be consulted to determine whether there is cancer or not. Because urethral cancer can cause life-threatening risks if not treated with early diagnosis.
HOW IS URETHRAL CANCER DIAGNOSED?
Since the symptoms of urethral cancer are often similar to the symptoms of other diseases, patients are often treated for different diseases. These treatments can be urinary tract infections or benign prostatic hyperplasia in men. Patients who do not get results from these treatments should be examined in detail. After obtaining information about the patient’s reasons for consulting a doctor, risk factors and family history of the disease, the patient is physically examined. Men undergo digital rectal examination and women undergo pelvic examination to obtain information about tumors around the urethra. In addition, your doctor may request the following tests and procedures for a definitive diagnosis:
- Urine test
- Blood test
- Ultrasound
- Endoscopic examination (cystoscopy or ureteroscopy)
- CT scan
- Biopsy
As with most types of cancer, the most important test for the definitive diagnosis of urethral cancer is a biopsy. After a definitive diagnosis of urethral cancer, other tests can be performed to learn more about the cancer. These tests determine the stage of the cancer and how far the cancer has spread (metastasized). After the urethral cancer has been fully staged, the doctor makes a treatment plan with the patient and starts the treatment process as soon as possible.
HOW IS URETHRAL CANCER TREATED?
Urethral cancer treatment options are planned according to the type of urethral cancer you have, where it is located in the urethra, your gender, your test results and the stage of the cancer. The most important treatment methods for urethral cancer are as follows:
Surgical treatment
The most common treatment for urethral cancer is surgery. The cancerous tumor is surgically removed from inside or outside the urethra. Surgery is also used to remove cancer-affected lymph nodes around the urethra.
Radiation therapy
Radiation therapy destroys cancer cells with intense energy beams. In urethral cancer, radiation is usually used in combination with surgery or chemotherapy.
Chemotherapy
Urethra cancer tumor inhibitors are used before surgery to shrink the tumor and after surgery to prevent recurrence.
Surveillance
In the treatment of urethral cancer, in some cases the patient is only monitored. This means that the cancer is not treated immediately. In other words, if the tumor does not cause any problems in the patient, does not tend to grow or spread, the patient is kept under surveillance by the doctor with regular examinations and tests. If the tumor starts to grow or is detected to spread, other treatment options are applied to the patient.
Follow-up after treatment
With urethral cancer treatment, the tumor can be completely removed. However, this does not eliminate the possibility of cancer recurrence. For this reason, the patient should be kept under control by his/her doctor to catch the risk of cancer recurrence early and prevent possible spread.
FREQUENTLY ASKED QUESTIONS ABOUT URETHRA CANCER
What are the side effects of urethral cancer treatment?
Due to the chemotherapy and other drug treatments the patient receives during the urethral cancer treatment process, side effects such as hair loss, sores in various parts of the body, especially in the mouth, vomiting, loss of appetite and nervousness may occur.
Is urethral cancer a fatal disease?
Urethral cancer is an insidious disease that can progress without any symptoms at first. When urethral cancer is diagnosed early, it can be treated with surgery, chemotherapy and radiotherapy.
Does urethral cancer recur?
The possibility of recurrence of the disease after urethral cancer is treated depends on the initial stage and location of the cancerous tumor. Small-stage cancer and cancer in the anterior urethra have a lower risk of recurrence.
Is urethral cancer more common in men or women?
The urethra measures 8 inches in men and 1.5 inches in women. Cancer of the urethra is more common in men than in women.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS OVARIAN CANCER?

Epithelial cells form the main structure of the ovaries, which contain many different cells. Ovarian cancer can occur as a result of uncontrolled division and proliferation in epithelial cells or cells from the embryonic period. Mostly seen after menopause, 80 percent of ovarian cancers occur in epithelial tissue. 60 percent of ovarian cancers seen under the age of 20 are embryonic tumors.
WHAT ARE THE SYMPTOMS OF OVARIAN CANCER?
Ovarian cancer symptoms usually do not show themselves very much. Most of the symptoms of ovarian cancer are patient-specific and there is no typical symptom. Symptoms of ovarian cancer include abdominal pain, bloating and stomach discomfort, which can be said to be symptoms of many diseases.
The biggest symptom of ovarian cancer in advanced stages is a palpable mass in the abdomen, a feeling of downward pressure, fluid accumulation in the abdomen, abdominal swelling, urinary and intestinal complaints due to compression of the surrounding organs.
Some types of ovarian cancer may cause hormone irregularities. Accordingly, menstrual irregularities, hair growth due to increased male hormone secretion, and male pattern hair loss may be observed. Most ovarian cancer complaints are about abdominal swelling.
We can list the general symptoms of ovarian cancer as follows;
- Change in bowel habits, especially the appearance of constipation,
- Change in bladder habits, frequent need to urinate,
- Loss of appetite or feeling full quickly,
- Vaginal bleeding
- Weight loss,
- Abdominal pressure and bloating,
- Fullness or pain in the groin,
- Prolonged indigestion, gas or nausea.
WHAT CAUSES OVARIAN CANCER?
Although the causes of ovarian cancer are not very clear, it can be said that some risk factors cause this disease. Genetic, environmental and hormonal factors can be shown among the causes of ovarian cancer. We can list the causes of ovarian cancer as follows;
- People with a family history of breast or ovarian cancer are at increased risk.
- In recent years, changes in certain genes have led to an increased risk of ovarian cancer.
- The risk of ovarian cancer is increased in people taking ovulation-inducing drugs.
- Taking birth control pills reduces the risk of ovarian cancer.
- The risk of ovarian cancer is higher in women who have never been pregnant. The risk decreases in those who give birth.
HOW IS OVARIAN CANCER DIAGNOSED?
Early diagnosis of ovarian cancer is very important as with all other cancers. For early diagnosis, it is recommended that women do not neglect their annual routine gynecological controls. A palpable mass during gynecological examination or masses seen in the ovaries during ultrasound give the chance to intervene early in cancer.
Not every cyst in the ovaries means cancer. Most cysts, especially in women of reproductive age, are simple and harmless cysts. These cysts, which disappear on their own over time, do not carry a cancer risk. For this reason, the specialist doctor determines whether the cysts monitored by ultrasound are harmful or not harmful to the body. In addition, all kinds of cysts in menopausal women and young girls before menstruation are open to the risk of tumors. They must be evaluated in this respect.
In advanced stages of ovarian cysts and masses with tumor characteristics, tumor markers are checked in the blood. Some tumor markers (especially CA 125) are elevated in some types of ovarian tumors. However, high levels of CA125 and other tumor markers do not always indicate that the mass is cancerous, and low levels of tumor markers do not rule out cancer. In addition to tumor markers, Doppler ultrasonography can also help differentiate benign and malignant tumors by showing blood flow changes. All these methods are auxiliary methods. None of them is sufficient to make a definitive diagnosis. In cases that cannot be differentiated from cysts and masses that are thought to be tumoral (whether benign or malignant), surgery and taking a pathological sample biopsy during surgery provides a definitive diagnosis.
In the presence of a cyst, if tumor markers and doppler examinations are normal, if there are no findings suggesting that it is tumoral by ultrasound and examination and if the cyst is smaller than 8 cm, it can be followed up for a while. If there is no shrinkage or disappearance during follow-up, surgery is preferred.
HOW IS OVARIAN CANCER TREATED?
Ovarian cancer treatment is surgical and not only the uterus and ovaries, but all tissues in the body that are likely to be involved are removed. After surgical treatment, chemotherapy is applied. Surgery is used in all stages of ovarian cancer. In ovarian cancer treatment, if removal of the mass carries the risk of damaging vital organs, chemotherapy is first used to reduce the mass. Then, the surgical method intervenes in the cancerous mass and tissues. After ovarian cancer surgery, chemotherapy may not be necessary if the cancer has not spread to the body. If ovarian cancer has spread, chemotherapy or radiotherapy should be applied. Chemotherapy is applied for 6-9 cycles after the operation, depending on the stage of the disease.
New treatment alternatives in ovarian cancer are now frequently used in our country. Treatments with targeted agents increase the probability of cure, prolong survival and provide significant symptomatic relief. In the treatment of ovarian cancers, great care is taken to preserve reproduction. Especially in germ cell ovarian cancers and borderline type ovarian cancers seen at an early age, only the cancerous tissue or the cancerous ovary is removed and the uterus and the opposite ovary are preserved, making it possible to conceive.
FREQUENTLY ASKED QUESTIONS ABOUT OVARIAN CANCER
What are the stages of ovarian cancer?
The stage at which ovarian cancer is diagnosed is very important in ovarian cancer treatment. You need to know whether the cancer has spread from your ovary to the surrounding and surrounding organs. Staging in ovarian cancer is determined by the degree of spread of the cancer.
Stage 1: The cancer is in one or both ovaries, but only in the ovary.
Stage 1a: The cancer is confined to one ovary and within the ovary.
Stage 1b: The cancer is in both ovaries, but is still confined within the ovaries.
Stage 1c: The cancer is in one or both ovaries, but has spread beyond the ovarian border. A tumoral cyst on the ovary has burst, or cancer cells have been found in the fluid in the abdomen.
Stage 2: The cancer has spread to other organs in the pelvis, the area surrounded by the pelvic bones.
Stage 2a: Cancer has spread to the uterus, tubes or both.
Stage 2b: Cancer has spread to the bladder or colon.
Stage 2c: The cancer has spread to either 2a or 2b. The cancer has also spread beyond the ovarian margin, a tumoral cyst on the ovary has burst, or cancer cells have been found in the fluid in the abdomen.
Stage 3: The cancer has spread into the abdomen or involved the lymph nodes.
Stage 3a: Cancer cells have spread into the abdomen, but only in foci small enough to be seen under a microscope.
Stage 3b: Cancer cells have spread into the abdomen but are less than 2 centimeters in size.
Stage 3c: Cancer cells have spread into the abdomen and are larger than 2 centimeters or have spread to the lymph nodes, or both.
Stage 4: The cancer has spread to the liver, lungs or other distant organs.
What is the importance of early detection of ovarian cancer?
The response of ovarian cancer to treatment is directly related to how far the tumor has spread. When ovarian cancer is diagnosed at an early stage and with appropriate treatments, it can be eliminated by 80-90 percent. The cure rate for ovarian cancers diagnosed in advanced stages is 40-50 percent. After ovarian cancer surgery and chemotherapy, the patient should be checked regularly in case the disease recurs.
Is ovarian cancer fatal?
Ovarian cancer (ovarian cancer) is a very important disease that seriously threatens women’s health and life and can be seen at any age. Ovarian cancer is the most lethal of all cancers of the female genital organs. Compared to other gynecologic cancers, early ovarian cancers are usually diagnosed very late because they do not give almost any preliminary symptoms. Therefore, routine gynecologic USG is important for early diagnosis.
Is there a high risk of ovarian cancer after menopause?
Ovarian cancer is divided into two types depending on the type of tissue it originates from. The type of the disease changes the likelihood of occurrence and the age of onset. People who have never given birth and have a family history of breast and ovarian cancer are at increased risk of developing the disease. However, the most important risk factor is considered to be advanced age. Estrogen hormone support alone, especially after menopause, is among the factors that trigger ovarian cancer.
What is CA 125?
CA125 is a protein found on the surface of most ovarian cancer cells. It can be significantly elevated in the blood of women with ovarian cancer. Small amounts of this protein may also be produced in some other cancers.
What is CA 125 in ovarian cancer?
Values between 0 and 35 in the CA 125 test are normal. If there is a number between 35 and 50, this patient should be under control. At values above 50, ovarian cancer is suspected. However, CA 125 may not be high in every ovarian cancer.
Where does ovarian cancer metastasize?
Ovarian cancer can spread to various organs in advanced stages. In the treatment, it is necessary to know whether it has spread to the ovary and surrounding organs. The most important feature of this cancer is that it spreads to the abdominal organs. Since it can spread to intra-abdominal organs in a short time, patients are usually diagnosed at an advanced stage. Ovarian cancer can spread to the small and large intestines. It can also metastasize to the peritoneum, pelvis, lung and liver.
Can ovarian cancer be confused with other diseases?
Since ovarian cancer can cause symptoms such as digestive complaints, pain in the groin area, constipation, patients may waste time in gastroenterology or internal medicine services wondering if there is a problem in the digestive system. Sometimes the diagnosis can be made by these doctors. If digestive system problems are experienced in the advanced age group, the gynecology department should be consulted.
Is ovarian cancer surgery open?
In advanced stages, if there is fluid collection in the abdomen and tumor spread, open surgery is performed. In some cases, while laparoscopy is used to observe the extent of the tumor, if there is no large spread, the tumors can be removed in the same session. Or in these patients, laparoscopic or robotic surgery can be used to remove the uterus, ovaries, lymph nodes and appendicitis can also be removed if needed. Chemotherapy is also planned according to pathology.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS RADIOTHERAPY?

Radiation is a special type of energy carried by waves or particles. It can be produced by special devices or released by so-called radioactive substances. This energy is used in medicine for imaging purposes and also to treat cancer and some other diseases. Special devices are needed to direct the radiation to the diseased organ. In this way, the use of high doses of radiation energy for treatment is called “radiotherapy” or “radiation therapy”.
HOW DOES RADIOTHERAPY AFFECT THE BODY?
High doses of radiation have the ability to kill cells or prevent them from dividing and multiplying. Since cancer cells divide and multiply much faster than normal cells, radiotherapy is more effective on cancer cells than on normal cells. In addition, it is much easier for normal healthy cells to recover and recover than cancer cells. At the stage called “planning”, the necessary drawings are made to ensure that diseased tissues are exposed to maximum radiation and normal tissues are exposed to minimum radiation, and the treatment is applied in a targeted manner.
WHAT ARE THE BENEFITS AND GOALS OF RADIOTHERAPY?
Radiotherapy is used in almost every type of cancer that can occur in almost any part of the body and in approximately 50% of cancer patients. In some types of cancer, radiotherapy is the only treatment method. Radiotherapy alone or in combination with surgery and/or drug treatment (“chemotherapy”) is a treatment method that can provide complete recovery in many patients.
Radiotherapy;
- For single, targeted, high-dose and short-term treatment (stereotactic)
- To shrink the tumor before surgery (neoadjuvant),
- To remove cancer cells that may remain in the body at microscopic level after surgery (adjuvant),
- During surgery (intraoperatively) for some types of cancer,
- For direct treatment without surgery, in combination with chemotherapy (curative),
- In some cases where it is not possible to cure the disease completely, radiotherapy can be applied to reduce the patient’s complaints such as pain and bleeding. This type of treatment is called “palliative treatment”.
WHO ADMINISTERS RADIOTHERAPY?
A “radiation oncologist”, a physician specialized in the treatment of diseases with radiation, determines the type and plan of treatment the patient needs.
During the treatment, radiation oncologists work with a special team. In this team; 0
Radiation physicist: Checks that the devices work correctly and deliver the appropriate dose of radiation.
Radiotherapy nurse: Provides nursing services during treatment, helps to minimize side effects that may occur for the patient and helps with nutritional support during treatment.
Radiotherapy technician: Prepares the patient before treatment and performs the daily planned treatments using the treatment devices.
WHAT ARE THE TYPES OF RADIOTHERAPY?
Radiotherapy is applied in two ways. External (external) and internal (internal). In some patients, these two forms can be applied consecutively.
External (external):
In most patients, radiotherapy is given externally. It is usually performed in treatment centers and outpatient clinics and is performed by directing the rays to the diseased tissue using radiotherapy devices. Until recent years, external treatments were performed in 2D with devices called Cobalt-60 or linear accelerators. Since wide safety margins were required to deliver sufficient dose to the target volume in two-dimensional treatments, normal tissue damage and side effects were higher. However, thanks to technological changes in radiotherapy devices in recent years, three-dimensional conformal radiotherapy, IMRT (intensity-modulated radiotherapy), sterotactic radiotherapy (linac-based, gamaknife, cyberknife) can be applied to ensure that the target volume receives maximum dose while the normal tissue receives minimum dose. When the decision is made to use radiation therapy, the doctor will also decide which device is more suitable for the patient.
Internal:
With internal radiation, the radioactive material or source is inserted through thin wires or tubes either directly into the tumor or into a body cavity. This method, which is often used in gynecological tumors, can also be applied to the cavity left after surgery.
HOW DOES THE DOCTOR MAKE THE TREATMENT PLAN IN EXTERNAL RADIOTHERAPY?
The radiation sources used in radiotherapy are varied. The doctor may use X-rays or electron beams. The choice of radiation source depends on the type of tumor, its location in the body and especially its depth. High-energy X-rays are used to treat many types of cancer. Electron beams can treat some skin diseases.
Before the treatment begins, a preparation session with a computerized planning tomography is performed. The aim is to individualize the treatment and determine the irradiation technique that should be chosen according to the type and extent of the cancer. Details about this preparation session and the treatment itself (in particular the frequency and duration of the sessions) are explained to the patient by the radiation oncologist during the initial examination. First of all, the patient’s position in the machine during the radiotherapy sessions is determined and then a CT scan is taken in this position. Using CT scanning to plan the treatment allows the identification of the most risky areas for tumors and/or tumor spread, as well as the normal tissues that need to be protected. During the CT scan, immobilization devices, plastic masks may be used, or a contrast agent may be injected into a vein and filmed.
Markings are made on the patient’s skin to ensure that the “target volume” is irradiated under the same conditions from one radiotherapy session to the next. For this purpose, ink pens that do not come off easily are used or tattoos can be made. Since water-resistant tapes are used, daily bathing will not be a problem. In case your markings are erased, it will be appropriate to warn the technician and not to complete them yourself.
After the doctor determines the target volume and normal tissue by tomography sections, your doctor will consult with the radiation physicist to determine how much radiation dose the patient needs, how this dose will be given and how many sessions will last. The planning process may take place on the same day or may take a few days.
After the treatment starts, the doctor monitors the patient’s response to the treatment, general condition and possible side effects of the treatment. You can usually see your radiation oncologist once a week, but depending on the needs of the patient, the check-up may be more frequent. It is very important to receive scheduled treatments on time. Interruptions in treatment, unnecessary breaks may reduce the expected effectiveness of the treatment.
WHAT IS HYPERFRACTIONAL RADIOTHERAPY?
Radiotherapy is divided into daily doses according to tumor type and location. In hyperfractional radiotherapy, the daily dose is also divided into several smaller doses. If several treatments are to be given to an area in one day, they are usually administered at intervals of 4-6 hours.
WHAT IS INTRAOPERATIVE RADIOTHERAPY?
In intraoperative radiotherapy, surgery and radiotherapy are performed at the same time. The surgeon removes as much tumor tissue as possible and radiotherapy is given to the tumor bed in the operating room immediately after surgery to remove any tumor cells that may have remained in the removed area.
WHAT HAPPENS DURING A RADIOTHERAPY SESSION?
The patient takes off his/her clothes and puts on a gown before starting the treatment. For this reason, it is recommended that he/she comes to the treatment with clothes that he/she can change easily.
The radiotherapy technician uses the lines previously marked on the patient’s skin to identify the treatment area. The patient must sit in a special chair or lie on the treatment table. Each session lasts on average 15 minutes in the treatment room and the radiation dose is delivered over a period of 1 to 5 minutes. Receiving external radiotherapy is painless, just like an X-ray.
The patient does not need to hold his/her breath during the procedure unless there are special circumstances and only normal breathing is sufficient. During radiotherapy sessions, it is important that the defined dose is delivered in the most precise way so that the rays reach the right place in the body, that the patient’s position is not disturbed throughout the treatment, that the same position is created for each treatment and that the environment is immobilized to ensure the patient’s comfort in the best way. In this process called immobolization, accessories such as head-neck masks, vacuum beds, under-knee stabilizers or shoulder pullers can be used depending on the area being treated.
The radiotherapy technician leaves the room before the beam is delivered. The equipment is controlled from a small area nearby. The patient can also watch through a monitor or window. If the patient speaks, his or her voice can be heard over the loudspeaker and communication with the technician and the doctor can be established. Due to the large size of the radiotherapy devices, there may be some noise as they rotate at different angles around the treatment area. However, patients should remember that the devices are operated by the relevant technicians and their operation is regularly checked. Any questions about the treatment room or the devices can be asked to the technician or doctor.
It is not possible to see, hear or feel radiation in any way. If a situation occurs during the treatment session in which the patient feels very unwell or uncomfortable, the technician should be informed immediately. If necessary, the operation of the devices can be stopped immediately.
ARE THERE SIDE EFFECTS OF RADIOTHERAPY?
External radiotherapy does not make the body radioactive. Therefore, there is no need to avoid contact with people receiving treatment. Even in cases of contact such as hugging or kissing, there is no risk of adverse effects on other people.
The side effects of radiotherapy are usually complaints about the treated area. The doctor and nurse inform the patient about how to manage these side effects. The doctor or nurse should be informed if the patient complains of cough, fever, sweating or unusual pain during the treatment. Side effects usually disappear within a few weeks after the end of treatment and can be managed with medication or diet. Side effects that may persist for longer can also be managed with appropriate treatments.
The effectiveness of the treatment is monitored by the doctor. After treatment, pain, bleeding and other similar complaints are felt to decrease and other signs of improvement appear over time. The doctor may order some blood tests while monitoring the effects of the treatment.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is radiotherapy?

Radiation therapy is one of the most frequently used methods in the fight against cancer. When the German physicist Wilhelm Röntgen was working with cathode rays, he named these rays, which he had never discovered and recognized before, X-rays, or unknown rays. X-rays with increased energy are directed at cancerous tissues. Radiation therapy, which targets only the area where cancerous tissues are located, is used in many types of cancer. The main aim here is to disrupt the structure of cancerous cells so that they lose their ability to divide. In this way, it is possible to control the disease. Radiotherapy is used for different purposes (radical, adjuvant, neoadjuvant, prophylactic, palliative).
In which diseases is radiotherapy used?
Radiation therapy can be used in cancer patients who are deemed suitable. Radiotherapy can be used as a primary cancer treatment, especially in lymphoma (lymphoma) and head and neck cancers.
The National Cancer Institute (NCI) lists the types of cancer for which radiotherapy is used as follows
- Breast cancer
- Lung cancer
- Prostate cancer
- Colon cancer
- Head or neck cancers
Brachytherapy may be a particularly effective treatment for cancers in certain parts of the body.
- Cervical cancer (cancer of the cervix)
- Uterine cancer
- Rectal cancer
- Head and neck cancers
- Eye tumors
- Brain tumor
- Lung cancer
- Skin cancer
- Breast cancer
- Esophageal cancer
- Cancers of the anus region
- Bladder cancer
What are the advantages of radiotherapy?
Between 50% and 60% of all types of cancer require radiotherapy. In approximately 25% of individuals who regain their health, this is due to the effect of radiotherapy. Radiation therapy is used to remove cancerous cells that may persist after surgery for cancer treatment. Radiotherapy is also used to reduce the symptoms of cancer.
The advantages of radiotherapy are listed as follows:
- Cancers caught at an early stage can be cured in a short time.
- The spread of cancer to other parts of the body can be stopped.
- Effective treatment of recurrent cancers can be achieved
- Symptoms can be alleviated in advanced home cancers
- No soreness and pain during application
- No radiation is felt during the application
How is radiotherapy applied?
Radiation therapy (radiotherapy) is divided into external (external treatment) and brachytherapy (internal treatment). Generally, applications are performed with the external (external) method. During the treatment, the patient is asked to lie motionless on the table where the treatment will be performed. Radiotherapy, which has its own devices and apparatus, is often applied in individuals diagnosed with cancer, as well as in individuals with some benign tumors. In this room where special devices are positioned, treatments are carried out in sessions. Radiation therapy (radiotherapy) targets the point where the cancer formation is present. The situation is checked with cameras in a different room to confirm the duration of the radiation and the accuracy of the area to be irradiated. No pain, burning or shock is felt during radiotherapy. People do not realize that they are receiving radiation. Masks and accessories are used to reduce movement during radiotherapy in some anatomical regions.
Frequently asked questions
What are the stages of radiotherapy?
As with any other disease, cancer treatment follows a certain scheme or path. The following road map is planned for radiation therapy (radiotherapy) application:
- The basic step is the evaluation of the patient (staging, indication of treatment).
- Simulation (planning, CT scan)
- Drawings of the target tissue and organs that need to be protected by means of computer programs and the creation of 3D structures (tumor size, location, intact, environment, tissue)
- Treatment planning (beam types, dose calculations, comparison of techniques)
What is the difference between radiotherapy and chemotherapy?
Radiation therapy or radiotherapy is the treatment of cancer cells by targeting the area where they form. This region-focused treatment aims to eliminate the cancer cell in that area and prevent cancerous cells from forming in the same area again. The treatment method that aims to destroy cancerous cells by targeting the whole body and is applied through drugs is called chemotherapy. The treatment option according to the type and stage of cancer is determined by specialist physicians.
At which stage of cancer is radiotherapy applied?
Radiation therapy (radiotherapy) can be applied in all organ diseases that contain tumors, starting from the diagnosis period until the last stage.
How many sessions is radiotherapy?
This process varies depending on the stage of the cancer and the current conditions. This process, which is carried out by making decisions under the supervision of specialist physicians, is usually completed by administering certain radiotherapy doses between 10 and 40 days, divided into small pieces and given every day (except weekends).
How long does radiotherapy last?
Radiotherapy lasts approximately 10-20 minutes each day, depending on the area treated and the stage of the disease.
Is there pain during radiotherapy?
No pain is felt during radiotherapy. Radiation therapy is invisible to the eye. As it cannot be seen, there is no taste, smell or hearing.
When does radiotherapy give results?
Radiation therapy usually cannot be expected to give very fast and immediate results. Radiation therapy does not kill cancerous cell foci immediately. The death of cancerous cells can be expressed in days, weeks or months. These cells continue to die even after the radiotherapy is finished.
How should a patient receiving radiotherapy be fed?
It is important that patients receiving radiotherapy consume foods rich in protein. Loss of appetite may be observed during the treatment phase. Appetite problems may not occur in every individual, but sore throats, vomiting, fatigue, exhaustion, tooth and gum problems, changes in taste can lead to nutritional problems. In addition to the importance of protein consumption for the regeneration of tissues, carbohydrate consumption, which provides energy to the body, is very important for fighting the feeling of weakness and fatigue during this phase. Oral and dental care and intestinal health should be taken very seriously during radiotherapy.
Does the patient receiving radiotherapy emit radiation?
This is a common misconception in the society. It is impossible for people to emit radiation after receiving radiotherapy.
What should a person receiving radiotherapy do?
First of all, in the first stage, the recommendations of the physician who monitors the disease should be followed. In general, one should not go above or below the ideal weight. As with all healthy individuals, it is important to provide energy to the body with food intake such as vitamins, protein, carbohydrates, etc., especially fluid consumption. In this process, importance should be given to the consumption of foods that provide cell renewal. However, supplementary foods, herbal teas, vitamins, special recipes that are thought to provide healing should never be used without consulting a specialist physician. Care should be taken to protect from sunlight by choosing clothes with fabrics that will not irritate the skin. Professional psychological support can be provided during this process.
What are the side effects of radiotherapy?
As with any treatment, radiotherapy may have some side effects. These side effects vary depending on the location and stage of the disease. The point to remember here is that since radiotherapy is a local treatment, side effects are not expected outside the area where it is applied. Generally, these include irritation, hair, hair and hair loss in the area where radiotherapy is applied. Difficulty in swallowing, changes in taste, burning in urine, feeling exhausted, diarrhea and dry mouth may occur. For example, in individuals undergoing breast radiotherapy, skin irritation and difficulty in swallowing are expected depending on the stage, but hair loss due to this treatment is not expected. In the treatment of abdominal cancers, diarrhea, stomach pain, burning in urine and frequent urination may be observed. As such, the side effects that may occur after the treatment of each region may differ from each other. In addition, another important point to know is that you can easily continue your daily life during the radiotherapy session.
What happens if radiotherapy is interrupted?
Radiotherapy is a treatment with different doses and durations depending on the type and stage of cancer and is usually administered on weekdays. Except for technical reasons, it is important for the success of the treatment to be applied continuously under these conditions.
However, in order to reduce the side effects that may sometimes occur, a break may be taken under the supervision of a physician, and if the treatment is interrupted due to technical problems, a revision can be made in the treatment period by making the necessary calculations under the supervision of a physician.
Where is radiotherapy applied?
Radiation therapy is applied in advanced cancer centers. Cancer patients can be treated with multidisciplinary approaches by teams including medical oncology, radiation oncology, nuclear medicine and related branch doctors.
Which devices are used in radiotherapy?
Advanced technologies such as Electa Versa Hd, Elecra Versa Signature and TrueBeam STx are used in our country for radiotherapy.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is radiotherapy?

Radiation is a special type of energy carried by waves or particles. It can be produced by special devices or released by so-called radioactive substances. This energy is used in medicine for imaging purposes and also to treat cancer and some other diseases. Special devices are needed to direct the radiation to the diseased organ. The use of high doses of radiation energy for treatment is called “radiotherapy” or “radiation therapy”.
In which diseases is it used?
Radiotherapy is used in almost every type of cancer that can occur in almost any part of the body and in approximately 50% of cancer patients. In some types of cancer, radiotherapy is the only treatment method. Radiotherapy can be used alone or in combination with surgery and/or drug therapy (“chemotherapy”) to achieve a complete cure in many patients.
Radiotherapy;
- To shrink the tumor before surgery,
- To remove cancer cells that may have remained in the body at microscopic level after surgery,
- Alone as a primary treatment of the disease
- For direct treatment without surgery, in combination with chemotherapy,
- In some cases where it is not possible to cure the disease completely, radiotherapy can be applied to reduce the patient’s complaints such as pain and bleeding. This type of treatment is called “palliative treatment”.
How is it done/applied?
Radiotherapy is administered in two ways. External (external) and internal (internal). In some patients, these two forms can be applied consecutively.
External (external):
In most patients, radiotherapy is given externally. It is usually performed in treatment centers and outpatient clinics and is performed by directing the rays to the diseased tissue using radiotherapy devices. Until recent years, external treatments were performed in 2D with devices called Cobalt-60 or linear accelerators. Since wide safety margins were required to deliver sufficient dose to the target volume in two-dimensional treatments, normal tissue damage and side effects were higher. However, thanks to technological changes in radiotherapy devices in recent years, three-dimensional conformal radiotherapy, IMRT (intensity-modulated radiotherapy), sterotactic body radiotherapy (linac-based, gamaknife, cyberknife) can be applied to ensure that the target volume receives maximum dose while the normal tissue receives minimum dose. When the decision is made to use radiation therapy, the doctor will also decide which device is more suitable for the patient.
Internal:
With internal radiation, the radioactive material or source is inserted through thin wires or tubes either directly into the tumor or into a body cavity. Sometimes it can be placed in the cavity left after surgery.
Stereotactic radiotherapy
In radiation therapy, ablative (destructive) radiation dose is given to certain points and maximum protection of normal tissues is ensured. These treatments are most effectively used in tumors of 3 cm or less.
It is most frequently used in patients who cannot undergo surgery in the early stages of lung cancer. It can also be applied individually to metastatic disease sites.
The treatment is often performed with 1 to 3 applications after special planning. Special devices can be used as well as certain linear accelerators.
It is a painless treatment method with minimal side effects.
What is the radiotherapy treatment plan and preparation process?
- Computerized planning tomography: Before the start of radiotherapy treatment, a preparatory session with a computerized planning tomography is performed. The aim of this is to individualize the treatment and determine the radiation technique that should be chosen according to the type and extent of the cancer. Details about this preparation session and the treatment itself (in particular the frequency and duration of the sessions) will be explained to the patient by the radiation oncologist during the initial examination.
- Identification of areas with tumors or tumor spread: During the radiotherapy session, the patient’s position in the machine is determined and then a CT scan is taken in this position. Using CT scanning to plan the treatment helps to identify the most risky areas for tumors or tumor spread, as well as the normal tissues that need to be protected. During the CT scan, an injection for the vein and sometimes a urinary catheter may be necessary depending on the area to be visualized.
- Radiation dose adjustment: After the doctor determines the target volume and normal tissue by tomography sections, the doctor and the radiation physicist work together to determine how much radiation dose the patient needs, how this dose will be given and how many sessions it will take. This usually takes a few days.
- Determination of the radiation source: The radiation sources used in radiotherapy are varied. The doctor may use X-rays or electron beams. The choice of radiation source depends on the type of tumor, its location in the body and especially its depth. High-energy X-rays are used to treat many types of cancer. Electron beams can treat some skin diseases.
- Marking the area to be irradiated: The radiation therapist makes markings on the patient’s skin to ensure that the “target volume” is irradiated under the same conditions from one radiotherapy session to the next. For this purpose, ink pens that do not come off easily are used or tatuage can be used. Nevertheless, care should be taken not to remove these markings while washing. Because these markings will be needed until the patient’s treatment is over. If erasures occur, the therapist should be informed. The patient should not complete the erased marks themselves.
- Monitoring the treatment effect: Once treatment has started, the doctor monitors the patient’s response to treatment, general condition and possible side effects of the treatment. This check-up is usually done once a week, but the frequency may vary according to the patient’s needs. It is very important that scheduled treatments are taken on time. Disruptions to the plan may reduce the expected effectiveness of the treatment.
What is the treatment process?
The patient takes off his/her clothes and puts on a gown before starting the treatment. For this reason, it is recommended that the patient comes to the treatment with clothes that can be easily changed.
The radiotherapy technician uses the lines previously marked on the patient’s skin to identify the treatment area. The patient must sit in a special chair or lie on the treatment table. Each session lasts 15 to 30 minutes in the treatment room and the radiation dose is delivered over a period of 1 to 5 minutes. Receiving external radiotherapy is painless, just like an X-ray.
The patient does not need to hold his/her breath during the procedure and only needs to breathe normally. During radiotherapy sessions, it is important that the defined dose is delivered in the most precise way so that the rays reach the right place in the body, that the patient’s position is not disturbed throughout the treatment, that the same position is created in each treatment and that the environment is immobilized to ensure the patient’s comfort in the best way. In this process called immobolization (immobilization), accessories such as head-neck masks, vacuum beds, under-knee stabilizers or shoulder pullers can be used depending on the area being treated.
The radiotherapy technician leaves the room before the beam is delivered. The equipment is controlled from a small area nearby. The patient can also watch through a monitor or window. If the patient speaks, his or her voice can be heard through the speaker and the technician can communicate with the patient. Due to their large size, radiotherapy devices may create a noisy environment as they rotate at different angles around the treatment area. However, patients should remember that the devices are operated by the relevant technicians and their operation is regularly checked. Any questions about the treatment room or the devices can be asked to the technician or doctor.
It is not possible to see, hear or feel radiation in any way. If a situation occurs during the treatment session in which the patient feels very unwell or uncomfortable, the technician should be informed immediately. If necessary, the operation of the devices can be stopped immediately.
Frequently asked questions about radiotherapy
HOW DOES RADIOTHERAPY AFFECT THE BODY?
High doses of radiation have the ability to kill cells or prevent them from dividing and multiplying. Since cancer cells divide and multiply much faster than normal cells, radiotherapy is more effective on cancer cells than on normal cells. In addition, it is much easier for normal healthy cells to recover and recover than cancer cells. At the stage called “planning”, the necessary drawings are made to ensure that diseased tissues are exposed to maximum radiation and normal tissues are exposed to minimum radiation, and the treatment is applied in a targeted manner.
WHO ADMINISTERS RADIOTHERAPY?
A “radiation oncologist”, a physician specialized in the treatment of diseases with radiation, determines the type and plan of treatment the patient needs.
During the treatment, radiation oncologists work with a special team. This team includes
- Radiation physicist: Checks that the devices work correctly and deliver the appropriate dose of radiation.
- Dosimetrist Determines the number and duration of sessions in treatments.
- Radiotherapy nurse: Provides nursing services during the treatment, helping to minimize side effects that may occur for the patient and helping the patient to tolerate them.
- Radiotherapy technician: Prepares the patient before treatment and ensures the operation of the treatment devices.
ARE THERE SIDE EFFECTS OF THE TREATMENT?
External radiotherapy does not radioactivate the body. Therefore, there is no need to avoid contact with people receiving treatment. Even in cases of contact such as hugging or kissing, there is no risk of adverse effects on other people.
The side effects of radiotherapy are usually complaints about the treated area. The doctor and nurse inform the patient about how to manage these side effects. The doctor or nurse should be informed if the patient complains of cough, fever, sweating or unusual pain during the treatment. Side effects usually disappear within a few weeks after the end of treatment and can be managed with medication or diet. Side effects that may persist for longer can also be managed with appropriate treatments.
The effectiveness of the treatment is monitored by the doctor. After treatment, pain, bleeding and other similar complaints are felt to decrease and other signs of improvement appear over time. The doctor may also order some blood tests while monitoring the effects of treatment. It is normal for these numbers to be low during treatment.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is hyperthermia?
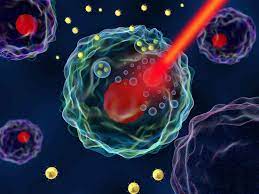
Hyperthermia means ‘treatment with heat’. The method, also known as thermotherapy, is an important treatment option preferred for many diseases, which is applied by increasing the patient’s whole body temperature through specially developed devices.
Which diseases is hyperthermia used to treat?
Hyperthermia methods are used in the treatment of cancer, which has many different subtypes. There are many studies showing that the method enhances the effect of basic cancer treatments such as chemotherapy and radiotherapy. As such, hyperthermia is an evidence-based “complementary” method in the field of cancer.
How is hyperthermia applied in cancer treatment?
Hyperthermia is examined under 2 main headings: ‘Whole Body’ and ‘Regional’.
Cancer treatment with whole body hyperthermia
A healthy person responds to the threat of illness with an increased body temperature – a fever. By heating the whole body, fever triggers an increased immune response. Fever plays an important role in the activation and regulation of the immune system. This can be described as a “natural, temporary immunological special program”. The main role of whole body hyperthermia in cancer treatment is to increase the effectiveness of concomitant chemotherapy and to strengthen the immune system. Especially in patients with widespread tumors, when administered with chemotherapy, it makes the treatment more effective and can also trigger a measurable increase in immune system function.
In whole-body hyperthermia, one of the oldest therapeutic principles is to raise fever by directing skin-safe and depth-effective water-filtered infrared-A ray-emitting lamps directly onto the abdomen and torso. During the procedure, the patient’s vital functions (blood pressure, pulse, oxygen saturation, respiratory frequency and body temperature) are monitored to ensure a controlled and targeted increase in body temperature. Since studies have shown that the optimum body temperature for activation of the immune system is between 39 °C – 40 °C, the target body temperature for cancer treatment is between 39 °C – 40 °C, also referred to as “moderate” whole body hyperthermia. Although the treatment may vary depending on the body’s response and the time it takes to reach the target temperature, it takes about 4 hours on average.
Cancer treatment with local hyperthermia
Regional hyperthermia has been developed after many years of research in the field of cancer treatment. Based on the principle of heating the tumor area with radio frequency waves, this method can safely and effectively improve the effectiveness of existing cancer treatments such as chemotherapy and radiotherapy. In this method, also called “regional deep electro hyperthermia”, intense energy is applied to the tumor area and the targeted temperature in the tissue is between 42°C and 44°C. Tumor cells hide from the immune system using various cellular mechanisms. However, with the heat given by applying regional hyperthermia, these cells can be seen. In this way, hyperthermia can make radiotherapy and/or chemotherapy more effective. In some cases, chemotherapy and/or radiotherapy, which were not effective before, may give more successful results when used in combination with hyperthermia.
Under the influence of hyperthermia, cancer cells form “heat shock proteins”; these proteins appear on disrupted cell surfaces. The body’s own immune system recognizes these proteins as foreign cells. This is a clear indication for immune cells to fight cancer cells. Under hyperthermia, there is no significant increase in heat shock proteins in healthy cells and normal cells are not damaged by hyperthermia.
During the treatments, which last an average of 60 minutes, the patient lies comfortably on the treatment bed. Power-adjustable radio frequency waves are directed at the tumor area with two opposing electrode heads, reaching a high temperature of 42 °C to 44 °C. This temperature damages cancer cells and tumor vessels.
- Primary tumors or tumors that have spread (metastasis)
- Tumors in organs (liver, pancreas, kidneys, lungs, etc.)
- Digestive system tumors
- Tumors of the hip region (pelvis)
- Head and neck tumors
- Brain tumors or spread to the brain (metastasis)
- Breast cancer (local recurrence of breast cancer)
- Prostate cancer
- Melanoma
- It is applied for superficial tumors.
Frequently asked questions about hyperthermia applications
What effect does heat applied in hyperthermia have on cancer cells?
The cellular stress and damage caused by heat causes cancer cells to undergo apoptosis (programmed cell death).
How does hyperthermia enhance the effect of chemotherapy and radiotherapy?
There is hypoxia (lack of oxygen) and an acidic environment in cancerous tissue. This reduces the effect of chemotherapy drugs and radiotherapy on cancerous tissue. With an increase in temperature, the blood supply to the tumor increases, thus reducing the acidic environment and helping other treatment methods to play a more effective role.
How does hyperthermia affect the functioning of the immune system?
Heat increases the production of “heat shock proteins” at the cellular level. This increases the activity of immune cells known as ‘natural-killers’. The production of tumor-specific antigens and the release of antigens out of the cell also increase with the effect of heat. In other words, in a sense, the masks that enable cancerous cells to hide from the immune system fall off. This makes it easier for the immune system to recognize the cancer. Both whole body hyperthermia and regional hyperthermia facilitate the passage of antigen-presenting cells, which are specialized cells of the immune system, to the lymph nodes and the immunological response of T cells “at the tumor site”
What changes does hyperthermia cause in the capillary structure of the tumor?
The structure of the capillaries that feed the tumor in cancerous tissue is different from normal vessels, and especially with regional hyperthermia, microthrombosis (clots) can form in these vessels, disrupting tumor nutrition.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS PLEURAL CANCER (MESOTHELIOMA)?

Inside the chest cavity is lung tissue. The lung is covered by a very thin membrane tissue similar to an onion membrane. This membrane tissue covering the lung also reaches the inside of the ribs. The cancer that forms in this membrane tissue is called mesothelioma, i.e. cancer of the lung membrane.
WHAT ARE THE SYMPTOMS OF PLEURAL CANCER (MESOTHELIOMA)?
Pleural cancer (mesothelioma) is usually characterized by the development of fluid around the lungs, commonly known as lung blisters. On whichever side the pleural cancer (mesothelioma) develops, stinging pain can be felt on that side. Cough is less common in mesothelioma. Patients feel shortness of breath due to the development of fluid in the lung. Stinging sensation in the lung can also be a sign of pleural cancer. Early stage symptoms of pleural cancer are rare. Different from lung cancer in many respects, pleural cancer also differs in terms of symptoms. When pleural cancer is characterized by fluid collection, it is usually in stage 2.
Symptoms of pleural cancer (mesothelioma) are as follows;
- Blistering of the lungs
- Shortness of breath
- Pain
- Unexplained weight loss
- In rare cases, cough similar to lung cancer
WHAT ARE THE CAUSES OF PLEURAL CANCER (MESOTHELIOMA)?
“What causes pleural cancer (mesothelioma)?”, “What are the causes of pleural cancer (mesothelioma)?” are among the questions patients are curious about.
Asbestos is the most important known cause of mesothelioma. Although it is very unlikely among the causes of mesothelioma, virus-related developments can be seen. Although asbestos exposure is the most important factor, mesothelioma is not a rare disease. People who work in the ship industry, the insulation industry, the construction industry, the hardware store, the lining industry, the tank pallet factory, the investment industry or who have worked in or lived near these workplaces are more likely to develop mesothelioma due to the high risk of exposure to asbestos.
It takes a period of 10 years after exposure to asbestos for pleural cancer to develop. People who work with asbestos in their young adulthood develop pleural cancer after many years.
Asbestos is not only encountered in the industrial sector. In Turkey, asbestos is naturally found in the soil in provinces such as Diyarbakır Çermik, Eskişehir, Afyonkarahisar and Nevşehir. Asbestos, which is a soft and fragrant substance, is frequently used in these regions for covering houses or making molasses. Natural inhalation of asbestos can also lead to lung cancer.
Living with a person who has been exposed to asbestos can also cause pleural cancer. People exposed to asbestos can carry the fibers home on their skin or clothing. Exposure to asbestos in this way can increase the risk of pleural cancer. People who work with a lot of asbestos at work can reduce the risk of bringing asbestos fibers home by showering and changing clothes before leaving work.
Skin-to-skin contact with asbestos does not cause pleural cancer. Asbestos must be inhaled to cause pleural cancer.
HOW IS MESOTHELIOMA DIAGNOSED?
“How is mesothelioma diagnosed?” is one of the most frequently asked questions by patients.
If the person has symptoms of mesothelioma, and in addition, if there is long-term contact with asbestos, imaging with Computed Tomography is performed first. To clarify the diagnosis of pleural cancer, a biopsy is taken from the patient with a method called Thoracoscopy and sent to the laboratory.
WHAT IS THE TREATMENT FOR PLEURAL CANCER (MESOTHELIOMA)?
“Is there a cure for mesothelioma?”, “Can mesothelioma be treated with chemotherapy?”, “What is the treatment of mesothelioma?”, “How is mesothelioma treatment applied?”, “How is mesothelioma treatment applied?”, “Can mesothelioma be cured?” questions are frequently raised by patients.
It is important to make a good planning in the treatment of pleural cancer. Specialization, good follow-up and a multidisciplinary approach are important in the treatment of pleural cancer (mesothelioma). While surgical methods come to the forefront in the treatment of mesothelioma, chemotherapy, radiotherapy and immunotherapy are also used.
In the past, the lung and pleura were completely removed in mesothelioma surgery. However, as a result of the studies carried out in recent years, it has been understood that it is sufficient to completely remove only the lung membrane. Chemotherapy and, if necessary, radiotherapy are given afterwards. In some patients, the order of treatment may change. In recent years, immunotherapy, i.e. treatments aimed at the immune system, have been used effectively.
FREQUENTLY ASKED QUESTIONS ABOUT LUNG CANCER
What are the types of pleural cancer (mesothelioma)?
There are generally 3 types of mesothelioma;
- Epithelioid
- Sarcomatoid
- Mix type
There are no small cell or large cell types of mesothelioma, as there are in lung cancer.
What is the difference between mesothelioma and lung cancer?
Mesothelioma differs from lung cancer not only in where it occurs. The cells of mesothelioma are different from those of lung cancer. The stem cells that form internal organs as the human body develops are different. The stem cells that make up the membrane regions and nerve tissues differ from each other.
There are no pain sensors in the lung tissue, but there are pain sensors in the lung membrane.
Another difference between pleural cancer and lung cancer is the way it occurs. Since the pleura covers the entire chest cavity, it does not develop at a single point like lung cancer. It affects the lung membrane in the entire chest cavity and covers a very large area.
What are the stages of pleural cancer (mesothelioma)?
The stages of mesothelioma are not as sensitive as lung cancer in terms of indicating the patient’s chances of recovery. It may differ from classical cancer staging. Especially the stages other than the 1st and 4th stages may show differences in terms of life expectancy. Questions such as “What is the treatment of pleural cancer stage 3?”, “What are the symptoms and treatment of pleural cancer stage 4?”, “What are the stages of pleural cancer?”, “Last stage of pleural cancer”, “Is there a treatment for pleural cancer stage 4?”, “What is the treatment of pleural cancer stage 1?” are frequently raised by patients.
In general, pleural cancer (mesothelioma) is in 4 stages,
- Pleural cancer stage 1: The tumor is limited to the pleura. There is very little thickening of the lining of the lung.
- Pleural cancer stage 2: The tumor has spread to the membrane over the chest wall, heart and esophagus.
- Pleural cancer stage 3: The tumor has spread past the diaphragm and into the peritoneum. Lymph nodes may be involved.
- Pleural cancer stage 4: The tumor has metastasized to other organs.
What is the life expectancy for mesothelioma?
The life expectancy of patients with mesothelioma depends on the stage of the disease, the treatment received and the patient’s response to the treatment. Life expectancy in mesothelioma can vary from patient to patient. “How long does pleural cancer live?”, “What is the life expectancy of pleural cancer stage 4?”, “How long does a pleural cancer patient live?”, “How long does a pleural cancer patient live?”, “How long does a pleural cancer patient live?”, “Does pleural cancer kill?”, “How long is the life expectancy of pleural cancer? “, “What is the life expectancy of pleural cancer?”, “What is the survival rate of pleural cancer?”, “How many years does pleural cancer live?”, “Is there a chance of surviving pleural cancer?” are among the most curious questions.
A patient with pleural cancer;
- 8 months if he never takes the treatment,
- 12-18 months with chemotherapy treatment,
- With triple treatment, including surgical treatment, it has an average life expectancy of 24 months.
However, the results in each patient vary, and especially in recent years, immunotherapy treatment aimed at the immune system has led to significant prolongation in the survival of pleural cancer.
The life expectancy may vary according to the response of the patients to the treatment.
There are many options in the treatment of pleural cancer (mesothelioma). Since the risk of recurrence of mesothelioma is high, it is important to stagger treatment options. Instead of using all treatment options at the same time, applying treatment in stages according to the course of the disease paves the way for the best results.
How is mesothelioma surgery performed?
In pleural cancer (mesothelioma), a surgical method called open surgery is applied.
- The patient is placed on his or her side on the operating table and one of the ribs is removed and the pleural cancer surgery is performed.
- During the operation, the entire membrane on the lung and in the chest cavity is removed.
- If necessary, the diaphragm muscle can also be removed during pleural cancer surgery. If necessary, the pericardium can also be removed.
- It is not necessary to completely remove the lung in pleural cancer surgery.
- Mesothelioma surgery takes approximately 3-4 hours.
- After mesothelioma surgery, the patient stays in hospital for about 1 week.
- Since a large area is affected in pleural cancer surgery, there is an intensive care period of 1-2 days depending on the patient’s condition against the risk of bleeding.
What can be done to prevent pleural cancer (mesothelioma)?
Mesothelioma occurs in a very large area as the pleura surrounds the entire lung and ribs. Unlike other cancers, it is not seen in a single spot but in the form of tumors on the entire lung membrane in the form of grape seeds.
Before the development of pleural cancer, complete removal of the pleura is considered in risky patients. However, since it is not possible to completely remove the membrane of the lung that spreads over a very large area in millimeters, pleural cancer can still develop in patients in whom this method is applied.
It is important to prevent asbestos exposure to prevent pleural cancer. It should be checked whether there is asbestos in the workplace or living area.
It is important that workers in jobs with asbestos exposure follow all safety precautions, such as wearing protective equipment. In addition, showering or changing work clothes before taking a lunch break or going home should not be neglected in order to protect those in contact with asbestos.
Are smart drugs used in mesothelioma?
Immunotherapy, which has been used in the treatment of mesothelioma in recent years, gives positive results in the life expectancy of patients. Immunotherapy treatment is particularly effective in sarcomatoid, mixed type mesothelioma.
Is there a herbal treatment for pleural cancer (mesothelioma)?
The question “Is phytotherapy useful in mesothelioma?” is frequently raised by patients. According to scientific studies, there is no natural or herbal treatment for mesothelioma. The most important precautionary measure is to avoid asbestos exposure. However, there is no harm in consuming products grown in asbestos soil.
How should nutrition be in pleural cancer (mesothelioma)?
As with all cancers, it is important to eat more protein and less carbohydrate in mesothelioma.
Does pleural cancer (mesothelioma) metastasize?
Patients are curious about questions such as “Metastatic mesothelioma”, “Does mesothelioma metastasize?”, “Where does mesothelioma metastasize?”.
- In pleural cancer, especially the sarcomatoid type metastasizes. Sarcomatoid type of pleural cancer usually metastasizes to bone, liver, brain, heart and peritoneum.
- Epithelioid lung cancer usually grows at the site of origin and recurs in the same area. It can metastasize to the abdomen or the opposite lung.
- The areas where pleural cancer metastasizes are often the peritoneum and the lining of the heart.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS SKIN CANCER (MELANOMA)?

The skin, the largest organ in the body, has many functions. It covers the internal organs, protects the body against possible injury, prevents excess water and fluid loss and helps the body to provide vitamin D. It also protects against germs such as bacteria and harmful ultraviolet (UV) rays and helps control body temperature. Skin cancer, or skin cancer, is a malignant growth on the skin that occurs for many reasons. The skin consists of 3 layers: epidermis, dermis and subcutis.
Epidermis The epidermis is the top layer of the skin. The epidermis is very thin and is about 0.05-0.1 mm thick. It protects the lower layers of the skin and organs against external factors. Keratinocytes are the main cell types of the epidermis. These cells produce an important protein called keratin, which helps the skin to protect the body. The outermost part of the epidermis is called the coat (stratum corneum). In this part, dead keratinocytes are replaced by new ones. The cells in this layer are called squamous cells because of their flat shape. Living squamous cells are located under the chorion (stratum corneum). These cells move from the outer part of the epidermis to the lowest part of the epidermis, the basal layer. The cells in the basal layer are called basal cells. Their job is to divide to form new keratins. Thus, they replace older keratinocytes on the surface of the skin, which diminish over time.
Melanocytes are cells in the epidermis that can develop into melanoma (skin cancer). These skin cells produce brown pigments called melanin, which give the skin a bronze or tan color. Melanin protects the lower layers of the skin from some of the harmful effects of the sun. In many people, when the skin is exposed to the sun, melanocytes produce more of these pigments, causing the skin to tan. The epidermis is separated from the lower layers of the skin by a basement membrane. This is an important structure. Because when skin cancer progresses, it develops through this barrier and into the lower layers.
Dermis: This is the middle layer of the skin and is much thicker than the epidermis. It contains hair follicles, sweat glands, vessels and nerves, held in place by a protein called collagen, which gives the skin strength and elasticity.
Subcutis The lowest layer of the skin is called the subcutis. The subcutis and the lowest part of the dermis form a network of collagen and fat cells. The subcutis helps to maintain body temperature. This layer also has a shock-absorbing effect that helps protect body organs against injury.
WHAT ARE THE TYPES OF SKIN CANCER?
Melonoma Skin Cancer
Melanoma is a skin cancer that starts in cells called melanocytes, which give the skin its color. It is called malignant melanoma or cutaneous melanoma. Because most melanoma skin cancer cells continue to produce melanin, the tumor is usually brown or black in color. However, some melanomas do not produce melanin.
In this case, the cancer may appear pink, yellowish brown or even white. Melanoma skin cancer can occur on moles that are present in the skin, either naturally or acquired, and can occur anywhere on the skin covering the body, including the scalp and soles of the feet.
Melanoma skin cancer is most common on the neck and back in men and on the legs, neck and face in women. However, cancer can also develop in the palms of the hands, soles of the feet and nails. In addition to all these, it can rarely occur in the eye, mouth, genital or anal area. Melanoma, which is a treatable type of cancer when diagnosed at an early stage, can turn into a type of cancer that reduces the chance of treatment when it spreads rapidly.
Other Types of Skin Cancer
Basal cell and squamous cell cancers are most common in areas that are exposed to the sun, such as the head, neck and arms. However, they are also found in other parts of the body.
Basal Cell Carcinoma: It is the most common skin cancer. It is a cancer with small, bumpy, pink or red, transparent, shiny, shiny, pearl-sized bumps that are mostly flat, hard, pale in color or bleed easily even with a minor accident. The center is sunken and the area is blue, brown or black. Large basal cell carcinomas have a crusted or spreading area.
Squamous Cell Carcinoma: This is the second most common skin cancer. It may look like a growing lump. It often has a hard, scaly or crusted surface. It can also have a smooth, red blotchy appearance that develops slowly. Both of these skin cancers can develop in a flat area with little change from normal skin.
Acnitic keratosis is also known as solar keratosis. It can sometimes be a precancerous condition of the skin and is caused by too much exposure to the sun. Acnitic keratosis are small, hard or scaly spots, usually pink-red or skin-colored. It usually starts on the face, ears, upper hands and arms. However, it can also appear on other parts of the body exposed to the sun. Acnitic keratosis is usually multiple. Some may develop inside squamous cell cancers. Others remain the same or progress on their own.
WHAT ARE THE SYMPTOMS OF SKIN CANCER?
The most important symptom of skin cancer is a new spot on the skin or a change in the size, shape or color of the spot:
- Non-healing and recurring wounds
- Pigments protrude beyond the stain and spread to the surrounding skin
- Red and blue moles larger than 5 mm in size
- Increase in the number and size of moles
- Change in the appearance of the surface of the mole, such as mounding, bleeding, or nodules or lumps
- Redness or a new swelling beyond its border
- Increased sensitivity, itching or pain
It can sometimes be difficult to tell the difference between a normal mole and melanoma. In this case, it is best to consult a specialized dermatologist as soon as possible.
WHAT ARE THE RISK FACTORS FOR MALIGNANT MELANOMA (SKIN CANCER)? WHAT CAUSES SKIN CANCER?
- Exposure to Ultraviolet (UV) Radiation: UV rays are one of the main risk factors for melanoma skin cancer. They damage the DNA of skin cells and skin cancer begins. Sunlight is the main source of ultraviolet rays. Solarium is another source of UV radiation. People exposed to too much UV radiation from these sources have an increased risk of developing many skin cancers, including melanoma. We can list the main skin cancer risk factors as follows;
- UVA Rays: Causes cell aging and can damage cell DNA. It is thought to cause long-term damage to the skin, such as wrinkles, and is thought to play a role in the development of some skin cancers.
- UVB Rays: The main ray that causes sunburn and can directly damage cell DNA. It is thought to cause most skin cancers.
- UVC Rays: Cannot pass through the atmosphere. Therefore, it is not found in sunlight. Therefore, it does not cause skin cancer.
- Tanning beds: Studies show that people who frequently visit tanning beds to get a tan have a higher risk of melanoma skin cancer. UV lamps used for tanning in tanning beds should be “ultraviolet lamps” and should be labeled with the words “Continuous exposure to UV rays can cause premature aging of the skin and skin cancer”. In addition, for users who are constantly exposed to these rays, a label that reads “regular medical check-ups are necessary for skin cancer” could serve as a warning. This would reduce the tendency to use ultraviolet products (black light lamps, mercury vapor lamps, high pressure xenon and xenon mercury arc lamps, plasma torches and arc sources, etc.), especially for young people/children under the age of 18 who are at risk of skin cancer and for those with a family history of skin cancer.
- Moles Moles on the body are benign tumors and occur not only at birth but also during childhood and adolescence. Most moles never cause any problems. However, people with a large number of moles have a higher risk of developing melanoma.
- Dysplastic Nevus: Dysplastic nevi (nevi is the plural form of nevus), also known as unusual nevi, often look a little like normal moles but have some features of melanoma. They are usually larger than other moles and have an unusual shape or color, and most do not develop into cancer.
- Congenital Melanocytic Nevus: Moles present at birth are called congenital melanocytic nevi. It is estimated that the risk of developing melanoma in such moles that are present at birth is between 0 and 0% depending on the size of the nevus. People with large congenital melanocytic nevi have a higher risk of developing melanoma. For example, if the congenital nevus is smaller than the palm of the hand, the risk of melanoma is lower. In contrast, the risk of melanoma increases significantly for congenital nevi that are large on the back or buttocks.
- Fair Skin, Freckles and Light Hair: The risk of melanoma is 10 times higher in people with white skin and light hair than in people with black skin. The risk of skin cancer increases in people with red and blonde hair, white skin, blue or green eyes or freckles.
- Age: Melanoma is most common in young people between the ages of 15 and 29, but it is most common in the 25-29 age group (especially in young women). However, it can also occur at older ages.
- Gender: Skin cancers are divided into malignant meianoma and non-melanoma skin cancers based on their incidence and biological differences. While it is the 4th most common type of cancer in young adults, i.e. men between the ages of 25-34, it is the most common type of cancer in women after breast and gynecologic cancers.
- Welding and Metalworking: Shown to increase the risk of melanoma of the eyes
- Phototherapy (light therapy): Exposure to UV rays due to the treatment applied to people with certain skin diseases such as psoriasis increases the risk of squamous cell skin cancer.
WHAT ARE THE GENETIC FACTORS IN SKIN CANCER?
People with melanoma skin cancer in one or more first-degree relatives (parents, siblings or children) are at higher risk. Approximately 10% of people with melanoma have the same disease in their family.
One reason for the increased risk may be frequent sun exposure due to similar family lifestyles, a predominance of susceptible fair-skinned family members, or both of these factors. In addition, gene mutation as a result of a change in genes in the family may be a factor in the risk of melanoma. Gene mutations are found in approximately 10-40% of people with high rates of melanoma in their families.
Xeroderma Pigmentosum (XP): It is an inherited condition caused by damage to enzymes normally responsible for repairing DNA and is rare. People with XP may develop many skin cancers, including melanoma, on sun-exposed areas of their skin because they have less ability to repair DNA damage caused by the sun.
Unusual sores, bumps, spots, blemishes, scratches or changes in the appearance of that area of skin can be a sign of melanoma or another type of skin cancer, or a warning that cancer may be developing.
Normal Moles: They are usually brown, tan or black dots on the skin. They can be flat or high and raised, round or oval and are usually smaller than 6 m. Moles can be congenital or develop during childhood and adolescence. New moles that appear on the body in adulthood should be checked by a doctor for possible skin cancer.
When a mole develops on the body, it will remain the same size, shape and color for years. Some moles will disappear spontaneously over time. Many people have moles and most of these moles are harmless. However, it is important to notice any change in the shape, size or color of a mole in case of a possible development of skin cancer.
IMPORTANCE OF EARLY DIAGNOSIS IN MELANOMA
Skin cancers are visible cancers. As with other types of cancer, skin cancer can be treated without spreading when changes in the skin are noticed at an early stage.
In addition, treatment-related side effects are minimized in skin cancer treated at an early stage.
ARE EARLY AGING WARNINGS ON THE SKIN A SIGN OF SKIN CANCER?
Prolonged exposure to the sun increases the risk of skin cancer and premature skin aging. This product does not protect you from skin cancer or premature skin aging, but only from sunburn.” The same warning should be written on sunscreens that are not “broad spectrum”.
A warning should be added to the labels of products with a low Sun Protection Factor. Sunscreens with a Sun Protection Factor lower than 15 must be labeled with a warning. “Water resistant” does not mean “waterproof”. No sunscreen is waterproof or “sweat resistant”. Manufacturers will no longer be able to claim this. If the label on the front of the product is labeled waterproof, it must state that the effect lasts for 40 minutes or 80 minutes when swimming or sweating. Products cannot promise more than they are. Sunscreens cannot promise instant protection or protection for more than 2 hours without reapplication. They cannot use the phrase “Sun Protection”. It is possible to prevent premature aging and skin cancer by protecting your skin from sun damage.
Early Detection Screening Recommended Age Range;
There is no specific recommended age range. Early detection of skin cancers (Men, women, young people, adults, everyone’s skin can be examined at all ages.
HOW IS SKIN CANCER DIAGNOSED?
The most important symptoms of skin cancer are a new spot on the skin or a change in the size, shape or color of the spot. Unusual and non-healing sores, bumps, blemishes, scratches or changes in the appearance of the skin, changes in the surface of the mole (bumps, bleeding or the appearance of nodules or lumps), itching, tenderness and pain may be a sign of melanoma or another type of skin cancer or a warning that cancer may be developing. When such symptoms are encountered, consulting a specialist doctor immediately will ensure that the early detected health problem is quickly resolved.
Skin Self-Examination in Skin Cancer: It is very important to check the skin twice a month. It is important to know the characteristics of moles, spots and freckles by looking at skin spot photos, and to recognize the body enough to notice a new mole or spot. Skin self-examination should be done in a well-lit room in front of a full-length mirror where the whole body can be observed. By using a hand mirror, it is easier to view the blind spots of the body such as the back and buttocks in the full-length mirror. In men, 1 in 3 melanomas is seen on the back. All parts of the body such as the back, palms, soles of the feet, scalp, eyes and nails should be checked.
Medical History and Physical Examination: The first physical examination for skin cancer should be done by a specialized dermatologist. Using a technique called dermatoscopy (also known as epiluminescence microscopy or surface microscopy), spots or moles on the skin are closely examined and, if desired, images can be taken and possible spread in the lymph nodes under the skin near the suspicious area can be observed. Some skin cancers spread to the lymph nodes. When this happens, the affected lymph nodes may become enlarged and harder than normal. This can be very effective in detecting skin cancer early. It is important for people who have dysplastic nevus syndrome, or who have a family history of melanoma to have regular skin examinations.
Dermatoscopy in Skin Cancer Diagnosis
Dermatoscopy is microscopy of the skin surface and is used to diagnose moles and other pigmented lesions. In this method, the lubricated skin surface is examined with a dermatoscope, which provides a lighted magnification. The dermatoscope is similar to the otoscope used in ear examinations and has been widely used for more than 10 years. Until a few years ago, mole tracking was achieved by taking photographs of dermatoscopic images. Then computer technology was added to this method and digital dermatoscopy was developed. With this method, a map of the moles in the body is created and their point localization is determined. Then, a dermatoscopic image is taken and recorded for each mole. Thus, a comparison with the image to be obtained in the next control is provided.
The Digital Dermatoscope also creates an index showing the risk of malignant melanoma by mathematically calculating the suspicious changes observed in the mole. This index is helpful in diagnosis and treatment planning. While the chance of early stage melanoma diagnosis with the naked eye is 60%, it increases to 90% with digital dermatoscopic examination.
Skin Biopsy If the suspicious area is thought to be skin cancer, a sample is taken from this area and examined in the laboratory. This is called a skin biopsy. Skin biopsy can be performed in many different ways. The type of biopsy will be decided according to the location and size of the suspicious area on the body and the type of skin cancer suspected. If the suspicious mole or spot is found to be cancerous or precancerous, your doctor may want to carry out further tests or treatment. If the suspicious mole or spot is small and localized, a larger biopsy (to remove more tissue) or some form of surgery may be performed. For disseminated skin cancers, imaging tests and treatment with immunotherapy, targeted therapy, chemotherapy and radiotherapy will be needed.
WHAT ARE THE TREATMENT OPTIONS FOR SKIN CANCER (MALIGNANT MELANOMA)?
Skin cancer treatment aims to remove all cancerous tissue without leaving any residue. Surgical treatment can achieve a very high rate of success. The cancerous tissue removed in sufficient depth and width prevents the cancer from reappearing. In the treatment of skin cancer, in addition to destroying the cancerous cell, it is important not to leave aesthetic scars and not to cause loss of function. For the burden area where skin cancer is most common, the patient’s age, general condition, tumor size, skin characteristics and the possibility of spreading to the lymph nodes become important.
In skin cancer, individualized treatment modalities are offered rather than a uniform treatment. In terms of surgery and radiotherapy, there is usually no problem in the treatment of small tumors. Another important point is that an experienced team performs tumor removal in skin cancer treatment.
Radiotherapy may be preferred as the primary treatment model if there is excess scarring after surgical treatment and the tumor can be controlled with radiation without serious side effects. Non-melanoma skin cancer on the cheek, forehead or back of the nose, especially if it is basal cell, is treated very successfully with radiotherapy. Cryosurgery may be preferred for the treatment of small tumors. In the treatment where liquid nitrogen is applied on the tumor, abnormal cells die. After thawing, the dead tissues are separated from the body. In the treatment method called curettage, the cancerous area is scraped with a spoon-shaped curette, bleeding is stopped with an electric current provided by a special device and cancer cells are killed. At the end of the procedure, a flat, white scar is left on the skin. Local chemotherapy in the form of cream or lotion is also considered as an option for superficial skin cancers.
WHAT ARE THE WAYS TO PREVENT SKIN CANCER?
Prevention can be possible by reducing the risk factors that cause skin cancer and UV exposure. So, what kind of precautions can be taken to protect from the sun?
- Cover up. If you are not sunbathing, cover up, wear a wide-brimmed hat and protect your skin as much as possible. You can protect your eyes by wearing sunglasses that block at least 99% of UV rays.
- Sit in the shade. Do not sunbathe between 10:00 and 16:00 when the sun’s rays are strongest. Limit your exposure to direct sunlight to the times specified by experts.
- Avoid tanning in a solarium. It can contribute to skin cancer and cause long-term damage to your skin.
- Pay attention to the expiration date of cosmetics.
- Use broad-spectrum sunscreens with a sun protection factor of at least 30. Make sure to apply sunscreen every 2 hours, after swimming and sweating.
The US Food and Drug Administration (FDA) has introduced sunscreens that protect not only from sunburn, but also from UVA rays that trigger skin cancer and premature aging. In addition, the labels of moisturizers, lip balms and cosmetics must also indicate the degree of protection factor, just like sunscreens.
HOW TO USE THE RIGHT SUNSCREEN TO PROTECT AGAINST SKIN CANCER?
“Broad Spectrum” backed by testing: The new rules will ensure that when consumers buy sunscreen, they can be sure that it is “broad spectrum”, protecting them from both UVB and UVA rays. All sunscreen products protect against UVB rays, which cause sunburn. Now they will also protect against UVA radiation, which is linked to skin cancer and premature skin aging. Only products that pass the tests can be labeled “broad spectrum”.
IS SKIN CANCER DANGEROUS? IS SKIN CANCER DEADLY?
Everyone should examine their whole body (from the scalp in the first place to the parts of the body that are not easily visible (such as the back) in front of a mirror). The moles on our body should be closely monitored with regular control and we should consult a specialist in case of changes or non-healing, bleeding skin wounds. Suspicious lesion or previously diagnosed skin cancer / examination with Dermatoscopy (surface microscopy) device is recommended.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS THROAT CANCER?
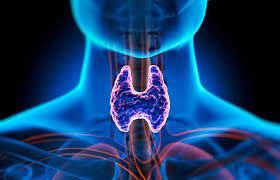
Laryngeal cancer, one of the head and neck cancers, occurs in the area of the throat between the root of the tongue and the windpipe, where the vocal cords are located. Also known as laryngeal or laryngeal cancer, laryngeal cancer is one of the most common types of cancer among head and neck cancers.
WHAT ARE THE SYMPTOMS OF LARYNGEAL CANCER?
- Hoarseness lasting more than 3 weeks: Hoarseness is one of the most common symptoms of laryngeal cancer. However, laryngeal cancer is not the only cause of hoarseness. Acute laryngitis, also known as inflammation of the larynx, shouting too much, smoking, reflux, runny nose, allergies, thyroid problems and old age can cause hoarseness. In addition to hoarseness, attention should also be paid to sudden changes in tone.
- Swallowing difficulties : Swallowing difficulties can be described in different ways. Swallowing problems can be described as a feeling of crumbs stuck in the throat, not being able to swallow food completely, pain or burning sensation during swallowing, feeling as if food is sticking to the throat.
Not all swallowing difficulties are a symptom of laryngeal cancer. Harmless narrowing of the esophagus known as stricture can also cause difficulty swallowing. However, it should not be forgotten that advanced laryngeal tumors can also cause difficulty in swallowing.
- Weight loss Uncontrolled weight loss can be a symptom of many cancers, not only laryngeal cancer. It is more common in advanced stages of laryngeal cancer. In cases of uncontrolled weight loss of 4-5 kg. in a short period of time, routine controls can be life-saving.
- Shortness of breath Shortness of breath or wheezing is also among the symptoms of laryngeal cancer. Especially in the case of progressive wheezing and shortness of breath, laryngeal cancer should be considered.
- Feeling of lump or swelling in the throat
- Fatigue
- Bad breath
- Ear pain
- Weight loss
Many of these symptoms can be caused by health problems other than cancer. Similar symptoms can occur especially in people who have smoked and consumed alcohol for many years.
These symptoms, which are signs of laryngeal cancer, can be caused by non-cancerous causes.
Chronic laryngitis, smoking, reflux, straining the voice, non-malignant benign tumors, tissue growths called laryngeal nodules on the vocal cords, wart-like growths in the larynx caused by HPV can be confused with laryngeal cancer symptoms. However, taking the symptoms into consideration and having the necessary controls can be life-saving.
What are the causes of laryngeal cancer?
There are risk factors that can cause laryngeal cancer to develop.
- Tobacco and alcohol use: Alcohol and tobacco use are among the most important risk factors that increase the risk of laryngeal cancer. The higher the amount of tobacco and alcohol use and the more years of use, the higher the risk factor. People who smoke more than 25 cigarettes a day or have smoked for more than 30 years are about 40 times more likely to develop laryngeal cancer than non-smokers. Likewise, long-term and regular alcohol users are 3 times more at risk than non-drinkers. Smoking is the cause of the majority of head and neck cancers, including laryngeal cancer. People who do not use cigarettes or tobacco products and are constantly exposed to their smoke are at increased risk of developing laryngeal cancer.
- Gender: Men are 4-5 times more likely to develop laryngeal cancer than women. However, the widespread use of cigarettes among women in recent years causes laryngeal cancer to be seen more frequently in women.
- Genetic factors: People with a family history of head and neck cancer or laryngeal cancer have a higher risk of developing laryngeal cancer than those without.
- Age: As with many types of cancer, advancing age is among the most important risk factors for laryngeal cancer. Laryngeal cancer is rare under the age of 40.
- Diet: People who eat a lot of red meat, processed foods or fried foods are at higher risk of developing laryngeal cancer. There are also studies showing that a diet deficient in vitamins A and E is also a cause of laryngeal cancer. Eating a diet based on fresh fruits and vegetables, known as the Mediterranean diet, and getting enough vitamins A and E can reduce the risk of laryngeal cancer.
- HPV virus There are scientific studies showing that the HPV (Human papilomavirus infection) virus, which is mostly sexually transmitted and causes genital warts, cervical and vaginal cancer in women, can cause laryngeal cancer. HPV is a common infection and most people can pass it on their own without causing any problems.
- Exposure to harmful substances: Long-term occupational exposure to certain harmful or chemical substances can cause laryngeal cancer.
- Sawdust
- Soot or coal dust
- Paint fumes
- Formaldehyde used in many industries such as paint production and cosmetics
- Nickel
- Isopropyl alcohol used as a cleaning solvent
- Sulfuric acid fog
- Asbestos
- Poor oral hygiene and reflux disease can also cause laryngeal cancer.
HOW IS LARYNGEAL CANCER DIAGNOSED?
Early diagnosis of laryngeal cancer provides significant advantages in treatment. It is vital that people with one or more of the symptoms visit a specialist ear, nose and throat doctor without delay.
- Doctor’s examination A doctor’s examination can give an idea about the disease when diagnosing laryngeal cancer. During the examination, the doctor evaluates lifestyle and occupational risk factors such as smoking and alcohol use. Since there may be a lump in the throat in laryngeal cancer, the doctor will perform a physical examination. During the physical examination, the doctor will examine the inside of the mouth, including the cheeks and lips for lumps or swelling, the floor of the mouth, the back of the throat, the nose and ears. A number of tests and imaging methods may be used to clarify the diagnosis of laryngeal cancer.
- Nasendoscopy: This is a type of endoscopy used by the doctor to get a better view of the larynx and throat. A flexible tube with a light and a small camera at the end is inserted through the patient’s nostrils to examine the larynx for abnormal structures. There is no need for preliminary preparation before the nasendoscopy procedure.
- Laryngoscopy Nasendoscopy is used when the larynx cannot be adequately examined or when a suspicious formation is detected. The endoscope used in laryngoscopy is longer and the procedure is performed through the mouth. The use of blood thinners can be discontinued before laryngoscopy. The procedure is usually performed under general anesthesia.
- Video Laryngostroboscopy: It can be used in patients who are not suitable for general anesthesia or to diagnose tumors in the vocal cords. The endoscope has a camera and a fiber optic flash light at the end. It can also be used to evaluate the vocal cords before, during and after treatment. The procedure takes about 30 minutes and can be performed under local anesthesia.
- Biopsy When a suspicious structure is seen in the areas examined during nasendoscopy or laryngoscopy, a tissue sample can be taken and sent to the laboratory. For biopsy, some or all of the tissue suspected of cancer can be surgically removed. Fine needle aspiration biopsy can also be performed in cases where there is a felt lump in the neck.
- Imaging methods can also be used to diagnose laryngeal cancer. Imaging modalities such as X-rays, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI) and PET can give an idea of the exact site and size of the cancer.
WHAT IS THE TREATMENT FOR LARYNGEAL CANCER?
Treatment of laryngeal cancer may vary depending on the exact site of the tumor, its stage, grade and the general health status of the patient. In general, surgery, radiation therapy (radiotherapy) and chemotherapy are applied in the treatment of laryngeal cancer. Sometimes only one of these options is used in the treatment, sometimes a combination of treatments can be applied.
Surgical Treatment of Larynx Cancer
Endoscopic resection (partial larynx removal with the method) (Endoscopic Laser Surgery)
- It is a surgical method mostly suitable for early stage laryngeal cancers and locally advanced laryngeal cancer patients.
- Endoscopic resection surgery, popularly known as intraoral laser surgery, does not involve any incision as it is performed through the mouth.
- Since a laser is used during the procedure, bleeding is less.
- The procedure is performed in the operating room under general anesthesia.
- The necessary surgical instruments and laser are passed through a tube from the mouth to the vocal cords. In the operation performed under a microscope, the surgeon sees the cancerous tumor clearly.
- Depending on the condition of the tumor, the surgeon can cut a part of it with a laser or destroy it completely with a high-energy laser.
- Before the endoscopic laser surgery procedure, it should be determined whether the patient is suitable for this surgery. Since laser surgery is performed through the mouth, the patient’s teeth and throat structure must be suitable for this procedure.
- The duration of hospitalization after laser surgery for the mouth may vary depending on the location and size of the tumor.
- Swelling after endoscopic laser surgery, which is usually performed on large tumors, can cause problems with breathing or feeding.
- Intraoral laser surgery usually does not cause permanent problems with speaking and swallowing. Speech may be restricted for a few days after surgery. For long-term speech problems, working with a speech therapist can give positive results.
Laryngeal Cancer Laryngectomy Surgery
- Depending on the size and location of the tumor, the affected part of the larynx or the entire larynx is surgically removed.
- Partial laryngectomy, in which only part of the larynx is removed, can be performed through a small incision in the neck or through the mouth without an incision.
- In partial laryngectomy operations, a small hole is made in the neck so that the patient can breathe. This hole is usually closed after surgery.
- After partial laryngectomy surgery, speech problems may occur temporarily. However, speech and breathing problems are usually not seen after the recovery period.
- In total laryngectomy surgeries, in which the entire larynx is removed, the windpipe is connected to the hole in the throat in order to breathe in and out.
- In total laryngectomy, i.e. surgery in which the entire larynx is removed, the hole in the throat is permanent.
- After total laryngectomy surgery, the patient loses his/her voice. The patient can communicate with voice prostheses produced as speech devices or voice devices.
- After total laryngectomy surgery, problems such as swallowing, taste and smell can be seen in addition to voice problems.
Neck Dissection Surgery
- Laryngeal cancer can sometimes spread to the lymph nodes in the neck. Usually the cancerous cells first spread to the lymph nodes. In the surgical treatment of laryngeal cancer, it is sometimes necessary to remove some or all of the lymph nodes.
- In neck dissection surgeries where lymph nodes are removed, muscles, nerves and nearby tissues can also be removed.
- Not all patients may undergo neck dissection surgery due to side effects.
- Although removal of lymph nodes is one of the most important measures to prevent the spread of cancer, it may cause side effects such as numbness in the ear, loss of movement in the lower lip, loss of movement and sensation in the tongue, loss of movement in the shoulder, loss of movement in the neck and arm, depending on the lymph nodes removed.
- Radiotherapy can be administered after neck dissection surgery.
- Any swelling, feeling of fullness or pressure, difficulty swallowing or changes in voice should be referred to a doctor.
Radiotherapy Treatment of Laryngeal Cancer
- Radiotherapy is the first choice for early stage laryngeal cancer. Radiotherapy, which uses high energy to destroy cancer cells, can be used alone or combined with surgery and chemotherapy depending on the location and size of the tumor.
- Radiotherapy treatment can sometimes be administered after laryngeal cancer surgery. To prevent the recurrence of laryngeal cancer, radiotherapy can be applied after surgery in cases where the entire tumor cannot be removed or in tumors growing along the laryngeal wall.
- In patients with advanced laryngeal cancer, radiotherapy can be applied together with chemotherapy to achieve better results.
- Radiotherapy for advanced stages of laryngeal cancer can reduce problems such as swallowing or breathing.
- During radiotherapy treatment, side effects such as fatigue, redness or darkening of the skin, sore throat, difficulty swallowing or swelling may occur.
Chemotherapy Treatment for Laryngeal Cancer
- Chemotherapy treatment for laryngeal cancer can be performed before and after surgery. It is usually applied together with radiotherapy.
- Preoperative chemotherapy can be used to reduce the size of the tumor to a level where it can be operated on.
- Chemotherapy can be used to prevent recurrence of laryngeal cancer.
- Targeted smart drugs have come to the forefront in chemotherapy treatment in recent years. Targeted smart drugs reduce the side effects of chemotherapy and increase the effectiveness of treatment.
FREQUENTLY ASKED QUESTIONS ABOUT GLANDULAR CANCER
Which Doctor Should I Go to in Laryngeal Cancer?
The larynx is part of the upper respiratory tract as well as a vocal organ. The first diagnosis and treatment of laryngeal cancer, also known as throat cancer or laryngeal cancer, is performed by Otorhinolaryngologists. When choosing an ear, nose and throat doctor for the treatment of laryngeal cancer, it is important to choose a doctor who specializes in head and neck surgery and a hospital with sufficient infrastructure in this field.
What are the Types of Larynx Cancer?
Laryngeal cancer is divided into types according to the cell type it starts.
- Squamous cell type laryngeal cancer: Almost 95% of laryngeal cancer is of this type. It starts in flat, flat cells in the thin, leaf-shaped flap at the top of the larynx called the epiglottis, or in cells with the same structure in other parts of the larynx.
Squamous cell type laryngeal cancer is also divided into types according to the area where it spreads.
- Glottic cancer – starts in the vocal cords
- Supraglottic cancer – starts at the top of the vocal cords
- Subglottic cancer – starts under the vocal cords
- Oropharyngeal cancer – starts just at the back of the mouth
- Nasopharyngeal cancer – starts in the back of the throat
- Adenocarcinoma is cancer of the larynx: Although its incidence has increased in recent years, it is much rarer than squamous cell type laryngeal cancer. It starts in mucus-producing adenomatous cells scattered on the surface of the larynx.
There are also very rare types of laryngeal cancer. There are rare types of laryngeal cancer such as small salivary gland tumors, sarcomas, melanoma, non-Hodgkin’s lymphoma or extramedullary plasmacytoma.
What are the Grades of Laryngeal Cancer?
The grade of laryngeal cancer is related to the appearance of the cancerous cells. It is generally divided into low-grade and high-grade laryngeal cancer.
- Low-grade laryngeal cancer; cancer cells look similar to the cells from which they originated. Low-grade laryngeal cancer cells usually grow slowly and are less likely to spread.
- High-grade laryngeal cancer; the differentiation of cancer cells is high. High-grade laryngeal cancer cells tend to multiply faster and are more likely to spread than low-grade cancer cells.
What are the Stages of Laryngeal Cancer?
After the diagnosis of laryngeal cancer, determining its stage is important for shaping the treatment. The stage of laryngeal cancer is determined by determining how far the cancer has spread. Laryngeal cancer is divided into stages according to the exact location of the tumor, spread to nearby lymph and metastasis to distant organs.
There are 5 stages in laryngeal cancer.
- Stage 0 is a very early stage when abnormal cancer cells have not spread to surrounding tissues. Cancer cells are only in the inner lining of the larynx.
- Stage 1 and Stage 2; Early stage laryngeal cancer. The tumor is small and does not extend beyond the larynx.
- Stage 3; The tumor is larger and can affect one of the vocal cords. In Stage 3 laryngeal cancer, the tumor may also grow into the thin, leaf-shaped epiglottis at the top of the larynx or into the thyroid gland.
- Stage 4 is the last stage of laryngeal cancer. The tumor may have spread beyond the larynx to the thyroid gland, trachea or esophagus.
Is Laryngeal Cancer Fatal?
Laryngeal cancer is a fatal disease. Life expectancy varies according to the type, location, size and spread of the laryngeal cancer tumor and the patient’s response to treatment.
In general studies, the 5-year survival times after appropriate treatment are as follows.
- stage laryngeal cancer 90%
- stage laryngeal cancer 70%
- stage laryngeal cancer 60%
- stage laryngeal cancer 40%
According to the results of the statistics, it is not possible to say the patient’s life expectancy.
Patients should see their doctor every three to six months for the first two years after treatment. 80-90% of cancers relapse within the first 3 years.
Where does laryngeal cancer metastasize?
Cancerous cells can spread from the site to other parts of the body. Laryngeal cancer first metastasizes to neighboring tissues. In advanced stages, metastasis may also occur to distant organs.
- Along the larynx
- Soft tissues in the neck
- Thyroid gland
- Vocal cords
- Tongue base
- Swallow
- Trachea (trachea)
- Tongue muscles and neck muscles
- Esophagus
- Lymph nodes
- It can metastasize to the lung, liver and bones.
Will I be able to speak after laryngeal cancer surgery?
- Vocal cords can be preserved in partial laryngeal cancer surgeries. Although there is difficulty in speaking immediately after these operations in which the vocal cords are preserved, the voice can be restored after a while.
- However, after surgeries in which the entire larynx is removed, the patient loses his/her voice.
- After these operations, different speech techniques or devices can be used depending on the patient’s condition. So-called esophageal speech can be achieved by moving air down the esophagus and then bringing it back into the mouth. This can be done by working with voice therapists.
- By holding a small device called an electronic larynx against the neck, it is possible for the patient to make a sound.
- Voice prostheses, also known as voice microphones, can be used to enable the patient to speak.
How Should Nutrition Be After Laryngeal Cancer?
During the treatment of laryngeal cancer, there may be problems such as difficulty swallowing, pain, taste, weight loss after radiotherapy or surgery.
Since solid food nutrition cannot be started immediately after laryngeal cancer surgery, a tube can be connected to the stomach through the nose, the hole in the throat or the abdominal wall. In this process, the patient receives liquid nutrients through this tube.
During the transition to normal nutrition, acidic and spicy foods should be avoided.
After some surgeries, patients may experience loss of taste. In order to overcome the loss of taste, strong sauces or herbs, garlic, lemon juice can be added to the food to add flavor.
Foods that are easier to chew and swallow should be preferred. If weight loss occurs despite this, additional vitamin supplements may be requested by consulting your doctor.
Can smoking cause laryngeal cancer?
Smoking is one of the main risk factors for laryngeal cancer. Laryngeal (laryngeal) cancer, which develops in approximately one in every 100,000 people in the society, can be seen mostly in male smokers, while the incidence of laryngeal cancer in women has recently increased with the increase in smoking. The most important symptom of laryngeal cancer is hoarseness, and an ear, nose and throat specialist should be examined, especially in hoarseness exceeding 2 weeks.
What Should Be Done to Avoid Laryngeal Cancer?
- There is no proven way to prevent laryngeal cancer. However, laryngeal cancer can be prevented by avoiding risk factors.
- The most important risk factor for laryngeal cancer is smoking. Quitting smoking significantly reduces the risk of laryngeal cancer.
- A diet based on fruits and vegetables is important. Make sure you get the necessary vitamins and antioxidants.
- Since HPV can cause laryngeal cancer, HPV vaccination should be done if necessary.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS A CHEST WALL TUMOR?
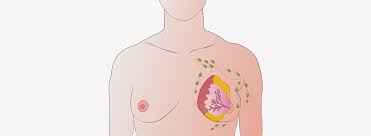
The chest wall is the structure that is adjacent to the vertebrae at the back, the ribs on the sides and the muscle layer that closes between the ribs, the sternum bone in front, popularly known as the bone of faith, the diaphragm muscle below and the clavicle (collarbone) above. The chest wall is the structure that provides the shape and strength of the rib cage. The muscular and bony structure of the rib cage contributes to breathing with the support of the abdominal muscles. The chest wall contains a wide variety of tumors involving the musculoskeletal system and connective tissue, and most of these tumors are malignant.
The classification of chest wall tumors is as follows
- Chest wall tumors are divided into primary and secondary tumors.
- It is often secondary to distant organ metastases (spread from other organs) and regional spread of tumors of neighboring organs such as lung, pleura, mediastinum and breast.
- Sarcomas are the most common malignant tumors arising from the chest wall itself, which we call primary. These tumors can be located in bone, cartilage and soft tissue. Of the chest wall tumors located in bone and cartilage, 50% are located in the costae (ribs), 30% in the scapula (shoulder blade), 20% in the sternum (sternum bone) and clavicle (collarbone).
WHAT ARE THE SIGNS AND SYMPTOMS OF CHEST WALL TUMORS?
Chest wall tumors can be asymptomatic, i.e. asymptomatic, or they can manifest themselves in different ways.
- Pain
- Subcutaneous swelling
- Symptoms such as infection can be seen in chest wall tumors.
While chest wall tumors of soft tissue origin usually grow painlessly, pain can be prominent in chest wall tumors of bone origin. For this reason, painful swelling may be the first sign of a chest wall tumor. In the event of an abnormal swelling in the body and pain symptoms that were not present before, it is useful to consult the thoracic surgery department without delay.
HOW ARE CHEST WALL TUMORS DIAGNOSED?
- Detailed history taking and physical examination is the first important method in the diagnosis of patients with suspected chest wall tumors.
- As for imaging, it is important to evaluate the chest radiograph first.
- If needed, advanced imaging methods such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) can be used.
- Computed Tomography (CT) better shows rib structures and intra-bone damage, while Magnetic Resonance Imaging (MRI) better reveals soft tissue tumors and their relationship with mediastinal organs and large vessels.
- Computed Tomography or Magnetic Resonance Imaging and PET-CT for whole body scanning after a suspected tumor is one of the advanced imaging methods used.
Which imaging method is preferred is decided according to the clinical condition of the patient.
WHAT IS THE TREATMENT OF CHEST WALL TUMOR?
- In the majority of chest wall tumors, the most effective treatment is the wide removal of the tumor with negative surgical margins (no tumor at the margins of the removed tissue).
- The areas to be removed by surgery are determined according to the cell type of the removed tumor and whether the tumor resembles a malignant tumor in type.
- Chemotherapy and radiotherapy are used for rapidly differentiating (high grade) tumors. In some cases, if there is a suspicion that a tumor remains in the removed chest wall, chemotherapy is also used to control this area.
- After surgery to remove a large chest wall tumor, special methods are used to close the cavity and allow the patient to breathe freely. Special materials or grafts from other parts of the body such as muscle, omentum or skin can be used for this purpose. The special materials used usually consist of materials that can be shaped during surgery according to the flexibility of the body. Which material will be used is decided before the operation depending on the patient’s condition and disease.
- After some surgeries, organs of the body such as muscles, skin, etc. can be used. This planning is done together with other branches such as plastic surgery and orthopedics as well as thoracic surgery.
FREQUENTLY ASKED QUESTIONS ABOUT CHEST WALL TUMOR
What is the duration of chest wall tumor surgery?
The duration of chest wall surgeries varies depending on the type of tumor, the size of the excised part and the additional procedures that may be required to close the cavity. While a simple soft tissue excision surgery can be completed in 30 minutes, surgeries requiring the removal of a large chest wall tumor can take 5-6 hours.
What is the process after chest wall tumor surgery?
After chest wall tumor surgeries, drainage tubes are often placed in the lung cavity, submuscular and subcutaneous surgical sites to drain the postoperative fluids produced by the body and these are monitored.
Patients can be taken directly to the inpatient ward, or they can be followed up in intensive care for a certain period of time after surgery, depending on the patient’s age, general condition, long-term disorders and the duration of anesthesia.
After the intensive care period, patients are followed up in the ward with chest X-rays and laboratory tests and are hospitalized for an average of 5-6 days.
What should be considered after chest wall tumor surgery?
After chest wall tumor surgery, the patient should rest for 1-2 weeks depending on the size of the surgery. The general well-being of the patient is evaluated and he/she is expected to be able to return to his/her social and working life after 1-2 weeks.
Is chest wall cancer a common type of cancer?
Chest wall cancers constitute 1-2% of all primary cancers and 5% of all thoracic cancers.
Is chest wall cancer a genetic disease?
There is a genetic predisposition in chest wall cancer. Especially in the sarcoma type, genetic factors have been clearly demonstrated in studies.
Who is more at risk of chest wall cancer?
Since most chest wall tumors are caused by metastases from other organs and regional spread to neighboring organs, people with a history of cancer should be more careful. However, chest wall cancers are 2 times more common in men than in women.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS EYE CANCER?

Eye cancer is a rare tumor that can affect the outer parts of the eye (such as the eyelid) or the inside of the eyeball (intraocular cancer). The most common intraocular cancers in adults are melanoma and lymphoma, while the most common in children is retinoblastoma, which starts in the retinal cells. Eye cancer develops when abnormal cells in the eye grow and divide uncontrollably. Regular eye examinations offer the chance to detect eye cancer at its earliest, most curable stage.
WHAT CAUSES EYE CANCER? WHAT ARE THE RISK FACTORS FOR EYE CANCER?
It is not known exactly why eye cancer develops, but there are some factors that can increase the risk of eye cancer, such as
- Having lighter colored eyes
- Advancing age (people over 50 years of age)
- Too many moles on the skin
- 1st degree relatives with eye cancer
- Weakened immune system
- Inherited conditions of pigment-producing cells, such as dysplastic nevus syndrome and oculodermal melanocytosis (also called nevus of Ota)
- Caucasian race: People of other races have a higher risk of eye melanoma.
Retinoblastoma in children is an inherited or genetically linked condition in about 25 percent to 30 percent of cases due to a mutation in the retinoblastoma gene (RB1). The inherited form of retinoblastoma tends to occur at a younger age and is more likely to affect both eyes than the non-hereditary form.
Ultraviolet (UV) radiation from sunlight has also been suggested as a possible risk factor for ocular melanoma, but this has not been proven. There is a known link between sun exposure and melanoma development. Although not yet proven, this may also include melanomas of the eye. This is why the American Cancer Society recommends wearing UV-protective sunglasses when outdoors, in addition to protective sunscreen and clothing.
WHAT ARE THE SYMPTOMS OF EYE CANCER?
People with eye cancer usually have no symptoms. Eye cancer is most often found during a routine eye exam. When symptoms do occur, painless vision loss is most common.
Any of the symptoms listed below can also be associated with other medical conditions, so any changes in vision or other eye problems should be referred to a healthcare professional.
Some symptoms of eye cancer include:
- Glaucoma (High intraocular pressure)
- Loss of field of vision
- Loss of vision
- Eye swelling Swelling of one or both eyes (proptosis)
- Seeing flashes of light
- Change in iris color
- Seeing dots, wavy lines or floating objects
- Mass visible in the anterior part of the eye
Children with retinoblastoma may have the following symptoms:
- Eyes seem to be looking in different directions
- Pain or redness in the eye
- Pupil appears white instead of red in flash photos
Although eye cancer is rare, it can cause life-threatening complications and death, especially if left undiagnosed and untreated. Anyone with visual symptoms such as difficulty seeing, loss of part of the field of vision or flashes of light, dark spots, dots, wavy lines or floating objects on the iris should seek medical attention immediately.
HOW IS EYE CANCER DIAGNOSED?
There is no widely recommended screening for eye cancer, but annual eye examinations (especially for those with identified risk factors) can play an important role in early detection. Eye cancers are often detected during routine examinations. Those diagnosed with primary eye cancer, where the cancer starts in the eye and has not spread, have a high survival rate.
If the doctor suspects eye cancer, he or she may order imaging tests or an eye ultrasound to help with the diagnosis.
Optical coherence tomography, also called eye tomography, is an imaging tool that illuminates the retinal layers to assess the subtle presence of fluid, a sign of tumor activity. Magnetic resonance imaging (MRI) can also be helpful for diagnosis. In some cases, the doctor may perform a fine needle biopsy to take a small sample of the tumor cells. The cytopathologist will analyze the sample to confirm the diagnosis within a few days.
The doctor may also order other tests to see if the cancer has spread to other parts of the body. Related tests may include:
- Blood tests to measure liver function
- Chest X-ray
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) scan
- Abdominal ultrasound
- Positron emission tomography (PET) scan
WHAT ARE THE TREATMENT OPTIONS FOR EYE CANCER?
After the diagnosis of eye cancer, the doctor will discuss the best options for treatment. The most appropriate treatment options for eye cancer depend on the following factors:
- Cancer type
- Places and extent of cancer
- Whether the cancer has spread to other areas (metastasis)
- Age and general health status of the patient
A small melanoma of the eye may not require urgent treatment. Radiotherapy uses high-powered energy such as protons or gamma rays to kill cancer cells. Radiotherapy is typically used for some small eye melanomas and for medium-sized eye melanomas. Treatment using a laser to kill melanoma cells may be an option in some cases. A type of laser treatment called thermotherapy uses an infrared laser (sometimes used in combination with radiation therapy).
For some small eye melanomas, cryotherapy can be used to destroy melanoma cells. Chemotherapy is rarely used for eye melanoma, but chemotherapy may be given for retinoblastoma and certain types of orbital lymphoma.
Surgical procedures in the treatment of eye cancer are as follows:
Eye-sparing surgery: This is usually performed for eyelid cancers, conjunctival cancers and orbital cancers.
Iridectomy: The iris (the colored part of the eye) is removed.
Iridotrabeculectomy: The iris and a small part of the outer part of the eyeball are removed.
Eye reconstructive surgery: Can often restore function after surgical removal of eyelid, conjunctiva or orbital cancer,
Enucleation: To treat some types of eye cancer, the entire eye must be removed. This is only done in advanced cases, for intraocular tumors such as uveal melanoma or retinoblastoma.
Orbital exenteration: This surgical procedure involves removing the eye, eyelids, surrounding skin, orbital muscles, fat and nerves. It is sometimes necessary for aggressive cancers of the orbit or sinuses, advanced or recurrent eyelid or conjunctival cancers.
*Page content is for informational purposes only. Always consult your doctor for diagnosis and treatment.
WHAT IS LYMPH CANCER (LYMPHOMA)?

Blood cancers is a synonym for all cancers that originate in the bone marrow, where blood is produced, or that originate in the blood. Lymphoma accounts for 50 percent of blood cancers. Lymphoma is divided into Hodgkin Lymphoma and Non Hodgkin Lymphoma. Non Hodgkin’s lymphoma is about 8 times more common than the other.
Both important types of lymphoma cancer have subtypes. Non Hodgkin’s lymphoma has at least 40-50 subtypes. There are 6-8 subtypes of Hodgkin’s lymphoma. The clinical course, response to treatment and the drugs used in their treatment are all different from each other. Therefore, after the diagnosis of lymphoma, it is necessary to accurately determine which subtype the disease is. Accordingly, the search for the best hospital for lymphoma treatment becomes very important. Hospitals with oncology centers with experienced and expert staff should be preferred.
WHAT CAUSES LYMPHOMA?
Although there is no clear answer to the question “What causes lymphoma?”, certain risk factors can be mentioned. As with all types of cancer, smoking and the use of other tobacco products are considered to be one of the most important causes. In addition, exposure to chemicals such as benzene and pesticides can also be mentioned as a cause of lymph cancer. In addition, the disease may be more common in rheumatic disorders and immunodeficiency conditions. Some virus infections that significantly affect the immune system are also an important cause of lymphoma. For example, lymphoma can be seen due to some infectious diseases such as hepatitis C, HTLV 1, HIV and AIDS.
Daily environmental factors are not at the forefront of lymphoma causes. However, lymphoma is slightly more common in agricultural workers, especially in greenhouse farmers. It is important to know that factors such as uncontrolled spraying, walking around in sprayed greenhouses without wearing masks and clothes, and inhaling the sprayed air in the greenhouse are effective. Otherwise, it should not be assumed that the pesticide on the vegetables at home is a factor. Workers in paint-producing industries also carry the same risk if the necessary precautions are not taken. In addition, it is not possible with current knowledge to point to household chemicals such as bleach, detergents, deodorants or cell phones as a cause. Anyone who leads an active life without gaining weight has an advantageous situation against many diseases. However, there is no information that obesity has a direct effect on lymphoma. It should not be forgotten that overweight is a risk factor for all types of cancer.
SYMPTOMS OF LYMPH CANCER (LYMPHOMA)
The first thing that comes to mind when we talk about lymphoma symptoms is that the patient usually notices a mass growing on their body. This mass can put pressure on certain areas. Lymphoma manifests itself as a clinical symptom mostly through the pathological enlargement of glands called “lymph nodes”. This is because it is mainly the lymph nodes where the tumor mass grows. Therefore, the majority of patients come to the hospital noticing enlarged lymph nodes in the neck, armpit and groin areas. One of the symptoms of lymphoma is that the patient may show flu-like symptoms because the immune system is not working adequately. Influenza is a disease that is expected to be cured within a maximum of one week from its onset. In addition, when sinusitis and lung infections occur, the duration may be longer. However, if the infection lasts for weeks and the infection picture worsens, a specialist opinion should be sought.
TYPES OF LYMPH CANCER (LYMPHOMA)
Significant advances have been made in hematologic cancers in recent years. These advances include a better understanding of the biological characteristics of blood cancers, improvements in diagnosis and success in treatment. A large number of drugs used in the treatment of many diseases in hematology have demonstrated their efficacy in new clinical trials, and among them, drugs with a very interesting mode of action and targeting cancer cells have come to the fore.
The most common cancers in hematology are lymphomas, which are cancers of the lymph nodes. We divide these diseases into two large groups: Hodgkin’s lymphoma and non-Hodgkin’s lymphoma (English: Non-Hodgkin’s lymphoma). Non-Hodgkin’s lymphomas constitute a basket of diseases with a large number of different biology and processes, and whose treatments have acquired completely different characteristics today.
Hodgkin Lymphoma
Hodgkin’s Lymphoma is characterized by enlarged lymph nodes. In some patients, symptoms of Hodgkin’s lymphoma include weight loss, night sweats and recurrent fever. Computerized tomography and a bone marrow biopsy are usually needed to determine the stage of the disease.
Hodgkin’s lymphoma is one of the cancer types with a high treatment success rate today. At every stage, treatment is aimed at completely eradicating the disease. There are a number of groups around the world working to improve the treatment of Hodgkin’s lymphoma, including the German Hodgkin’s Lymphoma Study Group (GHSG). So-called risk factors are important in the individualized treatment of the disease. In early-stage patients without bad risk factors, a short course of chemotherapy called ABVD and radiation therapy is sufficient. But if the disease is advanced, a much more effective treatment (escalated BEACOPP protocol) may be needed to completely eradicate the disease and prevent relapse. If there has been a relapse, high-dose chemotherapy and autologous stem cell transplantation are usually the best treatment option to completely eradicate the disease.
Non Hodgkin Lymphoma
Non-Hodgkin’s lymphomas are divided into 3 major groups: indolent (slowly progressing) lymphomas, aggressive (rapidly progressing) and very aggressive (very rapidly progressing) lymphomas. The prognosis and treatment of these diseases vary greatly. Non-Hodgkin’s lymphomas are also divided into 2 groups in terms of immunologic cell type: B-cell and T-cell lymphomas. Generally, T-cell lymphomas have a worse prognosis than B-cell lymphomas. For this reason, modern treatment of T-cell lymphomas is more intensive and effective. While in the past most Non Hodgkin’s lymphomas were treated with a chemotherapy protocol called CHOP, today more effective disease-specific treatments are used, depending on the subgroup of the disease. Some types of lymphoma can even be treated with antibiotic agents without chemotherapy. For example, some types and stages of lymphoma in the stomach or eye can be completely eliminated with antibiotic treatment. In order to choose the most appropriate treatment for the patient, the subgroup, stage and prognostic factors of the lymphoma must be known exactly. Choosing a fully equipped oncology center is very important in this sense.
Most Common Types of Non-Hodgkin’s Lymphomas
Slowly progressing lymphomas | Fast progressing lymphomas | Very rapidly progressing lymphomas |
Follicular lymphoma | Diffuse large B-cell lymphoma | Burkitt lymphoma |
Chronic lymphocytic leukemia | The majority of T lymphomas | Lymphoblastic B lymphoma |
Immunocytoma | Mantle cell lymphoma | Lymphoblastic T lymphoma |
Slowly Progressing (indolent) Lymphomas: The disease is usually diagnosed at stage III or IV. If the disease is diagnosed at stage I or II, treatment is aimed at eradicating the disease with radiation therapy. In advanced stages, chemotherapy is used in certain cases; if this is not necessary, the patient is monitored without treatment (“wait and see” in English), because in these cases it is not advantageous for the patient to start treatment earlier than necessary. In B-cell indolent lymphomas, a drug called Rituximab, which targets the CD20 molecule on B-lymphoma cells, increases the effect of chemotherapy and significantly affects response rates and response times.
Fast Progressing (aggressive) Lymphomas: Diffuse large B-cell lymphomas constitute a significant proportion of aggressive lymphomas. Treatment is aimed at eradicating the disease and consists of Rituximab and CHOP chemotherapy. In T-cell aggressive lymphomas, the addition of Etoposide to the CHOP protocol (CHOEP protocol) increases the success rate, as German and Scandinavian studies have shown. Since the prognosis is poor in most T-cell aggressive lymphomas, 6 cycles of chemotherapy followed by high-dose chemotherapy and autologous stem cell transplantation play an important role in the permanent control of the disease.
Mantle cell lymphoma, on the other hand, is an aggressive lymphoma that has made significant progress in recent years. In young patients, drug therapy is primarily prescribed. In young patients, stem cell collection, high dose therapy and stem cell transplantation give the best results. In elderly patients, maintenance therapy after chemotherapy prolongs life expectancy.
Very Fast Progressing Lymphomas: Another group is very aggressive lymphomas. The most important ones are Burkitt lymphoma and lymphoblastic lymphomas. These types of lymphoma are mostly seen in young patients. Burkitt lymphoma is the fastest progressing cancer type in humans. The goal of treatment in these diseases is to eliminate the disease. However, this goal cannot be achieved with simple treatments. The disease can be permanently eliminated with chemotherapies consisting of many drugs and reminiscent of leukemia treatment.
DIAGNOSIS AND TREATMENT OF LYMPHOMA
Treatment of lymphoma starts with a diagnosis of lymphoma. For this, a biopsy must first be taken. Lymphoma can be diagnosed by looking at these cells under a microscope. However, this morphological evaluation is not enough to subtype the disease. Different tests are required for a correct diagnosis. In addition, there are special tests that determine which type of lymphoma it is with special staining techniques.
Genetic Tests for Lymphoma Treatment
The genetic structure of the cells identified as lymphoma is also analyzed to accurately identify the subtype. This result is extremely important for the success of lymphoma treatment. After a definitive diagnosis is made, it should be investigated whether the disease has spread throughout the body. PET-CT is most commonly used for this. This test shows which part of the body is involved in the lymphoma.
Patients can consult a doctor at different stages for lymphoma treatment. In general, lymphoma is divided into 4 stages according to prevalence. Lymphoma stages 1 and 2 are called early, while stages 3 and 4 are called more advanced. After a definitive diagnosis of lymphoma is made, a special evaluation is carried out to determine the stage of the disease. In other words, it is possible to see to what extent the patient can respond to which treatment with this scoring technique. A number of factors such as the patient’s age, the level of LDH in the blood, whether the disease is at an advanced stage or not, whether there is involvement elsewhere other than the lymph node or not, are brought together and scored. Accordingly, patients fall into a low or high risk group. If the patient’s risk profile is high, they are less likely to benefit from standard lymphoma treatments. Therefore, these patient groups may have to receive more severe treatments. If the risk profile is low, more standard treatments are preferred.
Chemotherapy in Lymphoma Treatment
Chemotherapy plays an important role in the treatment of lymphoma. How and how chemotherapy will be administered varies according to the condition of the disease. In addition to standard, i.e. outpatient drug methods, high-dose chemotherapy is administered in inpatient follow-up in patients with rapid progression and high risk. Chemotherapy intervals in lymphoma treatment are usually 3 to 4 weeks and definitive results are expected after 6 cycles. During this period, the response is also monitored by interim evaluations. These follow-ups are carried out after the second or third cycle.
Chemotherapy is one of the most common treatments for blood cancers, especially lymphoma. Different drug combinations are used for each disease. The intensity of the drugs also increases when doses are higher than the standards and higher doses are administered. Since these drugs also damage healthy cells, problems that are seen in many conventional chemotherapies such as hair loss after treatment, disorders in the gastrointestinal system, sores in the mouth, loss of appetite, weight loss, weakness, and serious infections may occur. Since the complications that may occur in this type of treatment can be predicted in advance, necessary precautions are taken to ensure that the patient survives the treatment period in the most risk-free way. In addition to chemotherapy, radiotherapy is sometimes used as a support in the treatment of lymphoma. In cases where the disease is widespread, radiotherapy can be used to relieve the compression that can be caused by overgrown lymph in any area, even if it is not intended to treat the disease.
Immunotherapy Increases Lymphoma Treatment Success!
Apart from chemotherapy, immunotherapy is one of the treatments frequently used or applied together in the treatment of lymphoma. A number of drugs called “monoclonal antibodies” developed for cancer cells are frequently used in treatment. The special feature of these drugs is that they adhere to the lymphoma cells and then activate the immune system and destroy it through it. In the treatment of lymphoma, there are “monoclonal antibody” therapies that are used in combination with chemotherapy and differ according to the type of lymphoma. Such treatments increase the chances of success.
Lymphoma Medicines
There have been treatments for lymphoma for the last 10-20 years, but their acceleration and awareness have been increasing in the last 10 years. Targeted therapies are not limited to “monoclonal antibodies” today. A number of other drugs and molecules that are not monoclonal antibodies have also been developed. These are called “targeted” or “smart drugs”. With smart drugs, targeted molecules disrupt certain mechanisms that are present in cancer cells but not in healthy cells. Therefore, when the drugs are administered to the patient, the cancer cells are affected very intensely, while healthy cells are minimally affected. The side effects of drugs used in targeted therapies are never the same as the side effects of conventional chemotherapy drugs. Almost all patients do not experience problems such as hair loss, nausea, vomiting and loss of appetite. Mild and easily controlled side effects are also tolerated by patients.
The Most Effective Treatment Option in Lymphoma: Bone Marrow Transplant
Bone marrow or stem cell transplantation is frequently used in the treatment of lymphoma. There are two types of bone marrow transplants: autologous, which is made from the person’s own stem cells, and allogeneic, which is made using the stem cells of another person. The purposes of the two are different from each other. In general, the main purpose of bone marrow or stem cell transplantation is that bone marrow or stem cell transplantation is not an initial treatment. Bone marrow transplantation for lymphoma treatment cannot be performed as soon as the patient is diagnosed. In the treatment of lymphoma, chemotherapy, immunotherapy and radiotherapy are first used to eliminate or suppress the disease, and then transplantation is used when deemed necessary depending on the response. In some diseases, even if standard treatment is given at the initial stage and success is achieved, the disease is likely to recur after a while. In such patients, stem cell transplantation is performed to minimize the risk of recurrence.
Lymph Cancer Lymphoma Treatment: Autologous Stem Cell Transplant
Even if the disease is eradicated with standard treatment, microscopic cancer cells that are invisible to the eye are left behind and must be destroyed with very high doses of chemotherapy. This treatment also affects the bone marrow, which makes blood cells. For this reason, before the lymphoma treatment, the patient’s own stem cells are harvested by various methods and frozen and stored after undergoing special procedures. The patient is then given a very high dose of chemotherapy. After the treatment is over, the patient’s own bone marrow cells that were previously stored are transplanted back into the patient. These cells settle in the bone marrow and multiply there and start to produce blood. In other words, a bypass is performed and those cells are saved. However, autologous transplantation may not always be possible. Since the bone marrow of patients with bone marrow involvement cannot be taken from their own bone marrow, first of all, siblings or parents with a 25% chance of matching and, if necessary, a bone marrow bank are consulted.
MORALE IS VERY IMPORTANT IN LYMPH CANCER
Morale is also important for the doctor, as the patient’s positive outlook and belief in recovery will help the treatment of lymphoma. Although morale alone is not effective in defeating lymphoma, it ensures the patient’s compliance with the treatment process. The more the patient complies with the lymphoma treatment and the more he/she believes that he/she will recover and survive, the higher the chances of success naturally increase.
FREQUENTLY ASKED QUESTIONS ABOUT LYMPHOMA CANCER
Is weight loss and night sweats a sign of lymphoma?
Swollen lymph nodes, one of the symptoms of lymphoma, can also be seen in the chest or abdominal cavity.
It may not be directly noticeable how much the mass here has grown. However, the pressure created by this may cause complaints in the patient. Lymph enlargement in the chest can cause chest pain, dry cough and shortness of breath. A mass growing in the abdominal region negatively affects the functioning of the gastrointestinal system. Abdominal pain, diarrhea, constipation and digestive disorders are also symptoms of lymphoma. Some patients may also have complaints related to the systemic effects of cancer such as fever, weight loss and night sweats. If lymphoma is clinically suspected when the patient presents with these symptoms, the patient is examined to determine the presence of a growing and detectable mass. In addition, imaging methods should be used to check for any masses or lesions in the patient’s body. However, lymphoma is not only characterized by enlarged lymph nodes. It can also involve the liver, spleen, gastrointestinal system and lungs. Organ involvement may occur. Bone marrow can also be involved by these diseases. Because every tissue in the body has the potential to be involved by lymphoma.
Symptoms of lymphoma can also be manifested as allergic cough, asthma attacks and sinusitis. This is because none of the symptoms and signs of lymphoma are unique to the disease. Many other diseases can also have the same symptoms. Sometimes the symptoms of lymphoma can also be similar to those of rheumatic diseases. The patient may present to the hospital with complaints of rheumatic disease and the condition may be revealed by investigations. In short, lymphoma can mimic any disease. Therefore, symptoms of lymphoma should be taken into consideration.
One of the symptoms of lymph cancer is the enlargement of one of the tonsils rather than swelling of both tonsils. An asymmetrical enlargement is more likely to be lymphoma. The tonsil is actually a lymphoid tissue. Like the lymph gland, it is a lymphoid tissue located in the inner part of the mouth, in the throat and an organ of this system. It can hold that area and cause growth. Since the enlargement of the tonsils primarily suggests an infection, the patient is given treatment for infection. If no improvement is seen despite the use of medication over an expected period of, for example, 10 days, then other underlying causes should be investigated.
Can the patient’s body reject someone else’s stem cells?
Allogeneic transplantation, i.e. transplantation of stem cells taken from someone else, has some advantages and disadvantages. Although the basic philosophy seems to be the same compared to autologous transplantation, when the cells of a foreign person are transplanted, it may damage the patient’s own tissues and organs due to undetected tissue incompatibilities, even if the tissue compatibility is complete. The transplanted donor-derived defense cells may perceive the patient’s tissues as foreign and damage their organs. This can threaten the patient’s life. To prevent this, immunosuppressive drugs must be used for a long time. Patients also have to deal with the side effects of these drugs. The good thing about bone marrow cells from another person is that those lymphoid cells can also detect cancer cells in the patient and destroy them. Therefore, in allogeneic transplants, some fine-tuning is done with those cells and drugs to ensure that the transplanted cells destroy the patient’s cancer cells, but also to prevent the damaging effects on the patient as much as possible. Achieving this balance well reduces the chance of recurrence of the disease with a very successful allogeneic transplant.
What is the Life Expectancy of Lymphoma?
The clinical course of lymphomas is divided into two as fast and slow. Lymphomas with a rapid course appear in a very short time. The mass can grow in a very short time and manifest itself within months or even weeks. In those with a slow course, the growth rate of the mass is quite slow. It can cover a period of months or even years. Lymphoma life expectancy is also variable. When fast progressing lymphomas are left untreated, the patient may die within months or weeks. In cases with a slow course, regular follow-up is often sufficient.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS BREAST CANCER?
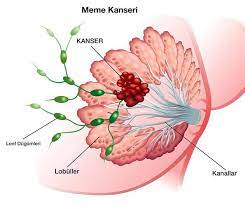
Breast cancer is caused by the uncontrolled proliferation of milk-forming cells that form the milk duct in the breast tissue. Breast cancer accounts for 33% of all cancers in women. It threatens 20% of all cancer patients. Today, 1 out of every 8 women lives with the risk of breast cancer throughout her life.
Breast cancer is cancer cells that form in the milk ducts within the breast tissue. Invasive ductal carcinoma accounts for 80 percent of breast cancers. Invasive ductal carcinoma indicates that breast cancer occurs in the milk ducts. Another 20 percent of breast cancer is invasive lobular carcinoma. In this type, breast cancer develops in the milk glands, not in the milk ducts. The cells that cause breast cancer take a long time to multiply and grow. Only after they have multiplied can the cells spread to other organs of the body through the lymph and blood. The most important thing in breast cancer is to diagnose the cancer before it spreads to other organs through the blood and lymph. The treatment rate is very high with a diagnosis made at this stage. Therefore, early diagnosis is very important in breast cancer.
In breast cancer, where early diagnosis ensures the continuity of a healthy life, it is very important to determine whether breast cancer cells have spread to the lymph nodes. Lymph nodes, which are an important criterion affecting the course of this disease, are caused by the spread of a cancerous cell in the structure of the breast. This spread may result in the spread of cancerous cells to different internal organs and the severity of the disease may result in negative twitching.
WHAT CAUSES BREAST CANCER?
Breast cancer is very rare in men compared to women. However, when the disease develops, its course can be faster and worse than breast cancer in women. One out of every 100 breast cancers is seen in men. Although the cause of breast cancer is not known exactly, many factors such as heredity, diet, socioeconomic status, menstrual status, births, birth control pills can be mentioned.
The incidence of breast cancer increases with age. The risk of breast cancer, which is most common in the 50-70 age range, increases when there is a family history of breast cancer. The risk of the disease increases 3 times when a mother or sister has breast cancer. For this reason, people with a family history of breast cancer should have frequent check-ups, especially after the age of 40. People with mutations in BRCA1 and BRCA2 genes have a high risk of developing both breast and ovarian cancer. Using hormone medication for more than 5 years during menopause is also one of the factors that increase the risk of breast cancer.
WHAT ARE THE RISK FACTORS FOR BREAST CANCER? WHO GETS BREAST CANCER?
The most important risk factors for breast cancer are those that we cannot change. In particular, having a family history of breast cancer is one of the leading risk factors for breast cancer. Breast cancer in a first-degree relative before the age of 50 increases the risk of developing breast cancer by 3 times. Breast cancer in 2nd degree relatives is also an important breast cancer risk factor. In addition, the more people in the family have had breast cancer and the earlier the age at which they were diagnosed, the higher the risk. Another important risk factor for breast cancer is dense breast tissue. People with less fat in their breast tissue have a higher risk of breast cancer. The density of breast tissue can be measured by mammographic and sonographic methods. Radiotherapy, especially in lymphoma patients, is also among the risk factors for breast cancer because it is applied close to the chest area. For this reason, it is recommended that patients who receive radiotherapy treatment, especially lymphoma patients, should have frequent lifelong check-ups after treatment.
Early menstruation, which is considered a risk factor for breast cancer in women, should also be taken into consideration. Especially those who menstruate before the age of 11 and those who enter menopause late are considered to be at higher risk of developing breast cancer. Not breastfeeding or having a first pregnancy after the age of 30, excessive alcohol consumption and being overweight are also risk factors for breast cancer. In addition, the hormone estrogen, which is used to reduce the effects of menopause, especially after menopause, increases the risk of breast cancer by 1.5 times.
Other breast cancer risk factors can be listed as follows:
- Being a woman is a primary risk factor for breast cancer.
- People with a family history of breast cancer have a higher risk of developing breast cancer than other people.
- The risk of breast cancer increases with age.
- White-skinned women are 20% more at risk than dark-skinned women.
- 5-10% of breast cancer cases are genetic. It is caused by defective genes (mutations) passed down through the family. The most common cause of genetic breast cancer is a genetic mutation in the BRCA1 and BRCA2 genes. The risk for family members with BRCA mutations is 80%.
- Receiving radiotherapy before the age of 15 increases the risk of developing breast cancer after the age of 40 to 35%.
- 2/3 of women aged 55 and over have breast cancer that has spread.
- Factors such as ageing or lifestyle can change the risk of breast cancer over time.
- Long-term heavy smoking has been found to increase the risk of breast cancer.
- A sedentary life away from physical activity and regular sports increases the risk of breast cancer.
- Obesity doubles the risk of breast cancer in women of childbearing age.
- In those with a family history of breast cancer, the use of birth control pills can increase the risk of cancer by 3 times.
WHAT CAN BE DONE TO PREVENT BREAST CANCER?
Breast cancer cannot be completely prevented. The incidence can be reduced with modifiable factors such as avoiding smoking and alcohol, eating a healthy diet and exercising.
WHAT ARE THE TYPES OF BREAST CANCER?
The types of breast cancer are determined by pathology examination of tissue taken by biopsy. Although there are many types of breast cancer, they are generally evaluated under two different headings:
- Ductal carcinoma, which occurs in the cells that form the breast ducts
- Lobular carcinoma of the milk glands of the breast
Ductal and lobular carcinomas are divided into non-invasive/in situ tumors that do not spread and invasive tumors that spread.
What are the differences between noninvasive and invasive cancer types?
Cancer is classified in two ways. Cancers classified as invasive and noninvasive differ within themselves. Cancer types that remain in the tissue where they are formed in the initial stage and do not spread throughout the body are defined as noninvasive cancer. Invasive cancer, on the contrary to noninvasive cancer, does not remain fixed in the tissue where it was formed in the initial stage and spreads. Breast cancer often develops in the milk-producing glands or milk ducts. Cancer is considered to be non-invasive if no spread is observed in the lobules, milk glands or milk ducts. Even if noinvasive cancer does not spread in the initial stage, it may develop into invasive cancer over time. At the same time, noinvasive cancer, which has a high chance of recurrence, requires long-term control and observation. Invasive cancers do not stay in the tissue where they develop and spread to large areas, causing the cancer to metastasize and increasing the risk of life-threatening. Once the cancer cells have spread, they may adhere to a site other than the original tumor site, resulting in the formation of a secondary tumor. As with all types of cancer, early diagnosis is very important in breast cancer. Starting at the age of 20, regular monthly breast check-ups for all women reduce the risk of negative consequences of breast cancer in the future. Thanks to early diagnosis, the course of the cancer is determined and treatment methods are applied individually by specialist physicians. Methods such as immunotherapy, chemotherapy, hormone therapy, radiation, surgery and targeted drug therapy offer options against noinvasive and invasive cancer types.
Ductal Carcinoma In Situ
It is a type of cancer that cannot be detected on palpation and manifests itself with irregular structure and calcifications on mammography. People with this disease may also have nipple discharge.
Lobular Carcinoma In Situ
It is an important condition that increases the risk of cancer in both breasts 8-10 times. Patients with this condition are kept under regular control and close follow-up. Patients are also given preventive medications.
In some patients, procedures such as removal of both breasts and evacuation of the breast tissue can be performed for preventive purposes. Surgical procedures such as prosthesis and breast reconstruction, which are performed to prevent any cosmetic problems, also contribute positively to the social lives of patients. Until 10 years ago, breast cancer could only be classified in 2 groups, but today it is categorized in 4 different subgroups. In addition, different treatment strategies and tumor-specific treatment methods have been developed. Until 10 years ago, breast cancer could only be classified in 2 groups, but today, breast cancer is categorized in 4 different subgroups. In addition, different treatment strategies and individual and tumor-specific treatment methods have been developed.
Invasive Carcinoma
Invasive cancer occurs when the cancer spreads further than the top layer of the cell where it started. Most breast cancers are invasive carcinomas. Among invasive cancers, ductal carcinoma, which arises from the cells that form the breast ducts, is the most common type of breast cancer.
Inflammatory Breast Cancer
It is known as the fastest and worst type of breast cancer. Its symptoms are similar to those of inflammatory diseases that completely envelop the breast. It does not give mass symptoms and sometimes it may only occur with symptoms such as redness and stiffness. In breast diseases that do not improve despite antibiotic treatment, it should be investigated whether there is an underlying cancer, and the necessary examinations and examinations should be performed, considering that the patient has cancer until proven otherwise.
WHAT ARE THE SYMPTOMS OF BREAST CANCER?
Knowing the symptoms of breast cancer is very important for catching breast cancer at an early stage and for successful treatment. The most prominent symptom of breast cancer is a palpable mass in the breast. The palpable mass can be in the armpit as well as the breast. If the lump is enlarged, nipple retraction is also a symptom of breast cancer. Although very rare, bloody or bloodless discharge from the nipple may also indicate breast cancer. If the tumor causing breast cancer becomes very large, the skin of the breast may swell and swell. Redness and orange appearance are also common symptoms of breast cancer. If breast cancer has spread, complaints about the area where it has spread can also be seen. Awareness of breast cancer symptoms is very important in order to prevent breast cancer from progressing. For this reason, it is necessary to recognize one’s own breast structure and know the risk factors. In order to recognize the symptoms of breast cancer, every woman should start doing breast self-examination after the age of 20. Breast self-examination should be done 5-7 days after the end of menstruation; women who do not menstruate should be examined once a month.
The symptoms of breast cancer are listed as follows:
- Palpable swellings in the breast, usually painless, firm, movable or immovable, with a structure and character that can grow over time.
- Visible change in breast size or shape, breast deformity,
- Redness, bruising, sores, vasodilation, inward depression, diffuse small bumps, punctate indentations on the breast skin, such as the appearance of orange peel.
- Changes in the color and shape of the nipple and its surroundings, enlargement, flattening, collapse, change in direction, crusting, cracks and sores on the nipple.
- Bloody or bloodless discharge from the nipple, nipple discharge,
- Painful or painless swellings that can be seen in the armpit and can be palpated.
However, remember that having a risk factor does not mean that you will develop the disease.
BREAST CANCER DIAGNOSIS
Early diagnosis of breast cancer is very important. Every woman should get to know her breast from the age of 20, have regular monthly check-ups and follow-up mammography from the age of 40. 8 out of every 10 masses in the breast are benign; in other words, they are not cancerous
Breast cancer diagnosed early is both very easy to treat and has a very high chance of success. For example, in breast cancer caught at Stage 0, the chance of success and the probability of the disease not recurring is 96%. In Stage I, the success rate is 93%, and 85% in Stage II. The earlier it is diagnosed, the higher the chance of success. For early diagnosis, every woman should perform breast self-examination in front of a mirror once a month from the age of 20. Between the ages of 35 and 40, women should have their first breast ultrasound and after the age of 40, they should have a mammogram once a year.
Eight out of every 10 masses seen in breast cancer diagnosis are benign. Most of these are non-cancerous masses called fibroadenomas or cysts seen in young ages and fibrocystic masses seen in middle ages. Whether the mass in the breast is painful or painless does not necessarily mean cancer. However, it is absolutely necessary to clarify what a different structure or mass that is palpable in the breast is and to consult a doctor when the mass is noticed. In recent years, social responsibility campaigns and awareness-raising programs to raise awareness about breast cancer in the society point to the importance of breast self-examination for early diagnosis of breast cancer.
MAMMOGRAPHY AND TOMOSYNTHESIS MAMMOGRAPHY: Digital mammography and tomosynthesis devices are used in breast cancer diagnosis and screening programs. Tomosynthesis is a technology that uses low dose X-rays and high resolution images. Thanks to mammography technologies, breast cancer can be diagnosed at an early stage and treatment planning can be done accordingly.
USG It is defined as an imaging system with advanced technological infrastructure that performs breast tissue examination through sound waves to detect cancerous cells in the breast. This system, which does not require preliminary preparation before ultrasound, is also radiation-free. This system, which is used for breast cancer detection, also shows whether the mass is solid or liquid. It is also known as the imaging system that is frequently used in all age ranges to examine anomalies in breast tissues. The results are available shortly after the scan.
MRI: Magnetic Resonance or MRI is one of the preferred imaging techniques in breast cancer examinations. In soft tissue examinations, drug-guided imaging is performed. This imaging technique is not used for renal patients because of the medication accompaniment. After the device is placed in the center, the breasts are placed in an area called coil, which is defined as a kind of wire made of platinum. This device, which has a strong magnetic substructure, may require comfortable clothing before MRI. Necklaces, earrings, bracelets, watches, etc. should be removed before imaging. The ideal time frame for breast tissue examinations for women is 7 to 10 days before the menstrual cycle. These images can take approximately 40 minutes or 1 hour. After imaging, it is recommended to consume plenty of water as MRI is performed with medication. With water consumption, the effect of the medication should be broken and these substances should be removed from the body. The results can be given in a short time depending on the intensity of the health institutions. Memorial Health Group hospitals use 1.5 Tesla MRI and 3 Tesla MRI.
PET-CT: PET-CT, which is one of the advanced technological imaging methods, can be described as the most valuable radiological method used in cancer stage such as detecting cancer cells and determining treatment methods. It is also necessary to determine whether the mass causing cancer is benign or malignant. Tumor size facilitates the spread of cancer throughout the body. This is very important in terms of determining the risk ratio and detecting the prevalence of the disease.
Some preparations are required before PET-CT scanning. At the beginning of these preparations, food consumption should be terminated for a period of 6 to 8 hours before the scan.
Breast Scintigraphy Scintigraphy is a painless, safe and safe method of examination with minimal side effects and allergies. Small amounts of radioactive substances are administered orally, intravenously, etc. It is possible to evaluate the spread of cancerous foci to different organs with scintigraphic methods. In breast cancers, it is guiding the detection of guard lymph nodes and the removal of these nodes. Medications used for different diseases before scintigraphy can be discontinued with the approval of the doctor. Shooting should be performed with a fasting state of at least 6 hours. It is important to stay still during these shots, which will take about 30 minutes. Gown, clothes, etc. No change of clothes is required.
EARLY DIAGNOSIS METHODS IN BREAST CANCER
- Breast self-checks
- Annual mammography
- Doctor examination
- Genetic tests
Breast examination is very important to prevent breast cancer and to catch breast cancer at an early stage. When breast cancer is intervened when it is a small mass in the breast, it can be treated with nearly 100% success. Another feature that distinguishes breast cancer from other cancers is that it can be evaluated within “cancer screening programs”. For this reason, women who have no complaints or masses related to the breast should pay attention to screening methods.
HOW IS BREAST SELF-EXAMINATION PERFORMED?
It is practical for women to regularly examine their own breasts in front of a mirror every month. Breast self-examination should be performed 4-5 days after the end of menstruation each month. Menopausal women and women who have had uterine or ovarian surgery should periodically perform breast examinations once a month, coinciding with the same days. In the breast examination, attention should be paid to the symmetry of the breast, whether there is a discharge from the nipple, the presence of any deformity, skin changes, and whether a mass has come to the hand.
BREAST EXAMINATION IN 3 STEPS
Examination in Front of a Mirror
Raise your arms upwards. Check both breasts for any irregularities, skin pulls or depressions, nipple sores, scabs, nipple retraction, changes in the breast. Put your hands on your waist and press down strongly. At the same time, contract your chest muscles well. Check your breast skin in the mirror for shrinkage. You may find that your breasts are not equal to each other. This is normal and should not be seen as a sign of illness. However, if there is a suspicious formation, you should definitely see a doctor.
Examination while showering
When examining your left breast while standing, hold your left hand above your head. With your right hand, examine your left breast by pressing from top to bottom and from bottom to top. With your right hand, examine your left breast by pressing from the outer side of your left breast towards the nipple in a radial or circular pattern.
*Do the same for your right breast using your left hand. If there is a different hardness in the breast the size of a hazelnut or walnut, inform your doctor.
Examination while lying on your back
When examining your right breast, place a pillow under your right shoulder and place your right hand behind your head. With your left hand, examine your right breast by pressing from top to bottom and from bottom to top. With your left hand, examine the outer side of your right breast by pressing in a radial or circular pattern towards the nipple.
*Do the same for your left breast using your right hand. Tell your doctor if there is a different hardness inside the breast, about the size of a hazelnut or walnut.
Gently squeeze the nipples of both breasts. Check for nipple discharge; if so, check whether it is light colored or bloody. Tell your doctor about any swelling, thickening or discharge you notice.
Mammography
For early detection of breast cancer, every woman over the age of 40 who does not notice any changes in her breast should have an annual mammogram. This way, it is possible to catch breast cancer before it reaches a palpable size. However, it is recommended to have at least one mammogram in the 30s and keep the film as a reference for future mammograms. Those with no family history of breast cancer should have their first ultrasound after the age of 35, while those with a family history of cancer and those at genetic risk of breast cancer should have their first ultrasound after the age of 25. These people should be under regular ultrasound follow-up every year from the age of their first ultrasound.
Doctor Examination
Regular medical follow-up is very important to detect and diagnose breast cancer at an early stage. Even if they have no complaints, all women after the age of 40 should consult a doctor and be examined. “Which doctor should I go to for breast cancer diagnosis?” is one of the most frequently researched topics. Breast cancer diagnosis and treatment process is carried out by general surgeons specialized in breast cancer. Your doctor who carries out your routine follow-ups on women’s health or general health may also request the necessary tests for early diagnosis of breast cancer.
HOW OFTEN SHOULD BREAST SCREENING BE DONE?
You should have a mammogram and ultrasound scan once between the ages of 35 and 40. This is called a “baseline mammogram”. After the age of 40, you should have routine screening mammography.
BREAST CANCER STAGES
Breast cancer is a type of cancer that progresses slowly. The tumor, which reaches a size of 1 cm within 5-7 years, can spread first to the lymph ducts and axillary lymph nodes and then to distant organs such as the liver and bones through the blood. Staging is performed to find out at what stage the tumor is and where it has spread, and treatment is decided accordingly. A system called TNM is used for staging in breast cancer. According to this system, T indicates the tumor diameter, N indicates the number of diseased axillary lymph nodes and M indicates distant spread (metastasis). There are 4 stages of breast cancer. Stage I, II and some stage III tumors are considered early stage breast cancer. Some stage III tumors and stage IV tumors are called advanced breast cancer. When staging breast cancer, the size of the tumor and whether it has spread to the surrounding lymph nodes are taken into consideration. Accordingly, we can define the stages of breast cancer as follows;
Stage 0 – DCIS
Stage I: The tumor is smaller than 2 cm and has not yet spread to the lymph nodes.
Stage II : The tumor is between 2 and 5 cm in size and may or may not have spread to the surrounding lymph nodes.
Stage III: It means it has spread more to the surrounding lymph nodes.
Stage IV: It means metastasized to other organs (bone, liver, brain, lung) or bone, distant lymph nodes.
BREAST CANCER DIAGNOSIS AND TREATMENT
In recent years, significant advances in the treatment of breast cancer and new treatment options have made it easier and more successful to diagnose and treat the disease.
Today, the diagnosis and treatment of the disease has become easier and more successful thanks to the significant advances in breast cancer treatment and new treatment options. The priority in breast cancer treatment is treatment and applications aimed at protecting the breast. In breast cancer caught at an early stage, the spread of the disease can be detected in advance with advanced techniques and measures can be taken and the tumor can be intervened directly without breast loss. In advanced breast cancer, breast reconstruction (a new breast) can be performed with plastic surgery techniques in cases where surgical removal of the breast is in question. Breast cancer can be treated at a rate close to 100% thanks to early diagnosis.
Breast cancer treatment depends on the stage of the patient. In stage 0, postoperative chemotherapy treatment is not needed. Radiotherapy is often added to the treatment. In stages I and II, since the mass is small, it is decided whether to perform surgery first and then chemotherapy. In stage III, chemotherapy is administered first and then the patient undergoes surgery. In stage IV, surgery can be considered if the cancer has not spread to too many parts of the body. However, if the cancer has spread too much, surgery alone is not recommended. Only chemotherapy and sometimes radiotherapy treatment is applied. Breast cancer-specific vaccines are also expected to be used in the treatment in the near future.
Surgical Methods
The primary goal of breast cancer surgery is to remove the tumor in such a way that it is not left behind and, in cases of spread to the armpit, to completely remove the lymph nodes.
Mastectomy
Simple mastectomy: This procedure is also called a total mastectomy. The entire breast, including the nipples, is removed, but the underarm lymph nodes or muscle tissues under the breast are not removed. It is a method that is not preferred today.
Skin-sparing mastectomy: In some female patients, the breast can be reconstructed during surgery. This procedure is called skin-sparing mastectomy. Most of the skin over the breast (including the areola and nipple) is left intact.
Radical Mastectomy: In this large-scale operation, the entire breast, axillary glands and the pectoral (chest wall) muscles under the breast are removed. Radical mastectomy has been used quite frequently in the past.
Breast conserving surgery
When breast cancer is detected early, the affected part of the breast is usually removed. However, the part to be removed depends on the size and location of the tumor and other factors. In a lumpectomy, only the lump in the breast and the surrounding tissues are removed. Radiotherapy is a treatment method applied after lumpectomy. If the patient will also receive adjuvant chemotherapy, radiotherapy is usually delayed until the chemotherapy treatment is completed. In a quadrantectomy, a quarter of the breast is removed. Radiotherapy is usually given after surgery. Again, if chemotherapy is to be given, radiotherapy is delayed.
Lymph node surgery
To determine the spread of breast cancer to the axillary lymph nodes, one or more lymph nodes are removed and examined under a microscope. This examination is important for staging the cancer and determining the treatment and outcome. If cancer cells are found in the lymph nodes, there is a high chance that the cancer has spread to other parts of the body through the bloodstream. The presence of cancer cells in the axillary lymph nodes plays an important role in deciding what kind of treatment, if any, is needed after surgery.
Radiotherapy treatment
Radiotherapy in breast cancer aims to destroy cancer cells that are likely to remain with the radiation given to the armpit and breast area after surgery. Radiotherapy in breast cancer treatment is applied to protect the remaining tissue of the breast, especially in patients with a high risk of regeneration and in patients who have undergone breast-conserving surgery. TrueBeam STx and Elekta Versa devices play an important role as radiation technology in the fight against breast cancer.
Thanks to these technologies, radiation oncology applications in the field of breast cancer focus only on cancerous cells and prevent damage to healthy cells.
Drug Treatments
Chemotherapy
In breast cancer, chemotherapy is usually administered after surgery. Although no cancerous cells remain after surgery, chemotherapy treatment may continue for a while as a preventive measure.
Hormonotherapy
The aim of hormone therapy is to reduce the amount of hormones a cancer patient has in cases of breast cancer that are sensitive to female hormones. Some cancer cells that are sensitive to the hormone estrogen grow and multiply faster. This treatment method prevents the cancer from developing by eliminating the estrogen effect.
Smart Medicines
Breast cancer is a disease that requires individual and tumor-specific treatment with different treatment strategies. While in the past years there were no options other than classical chemotherapy drugs and hormone therapies, today, the combination of newer and more effective chemotherapy drugs, targeted smart drugs that can be taken intravenously and orally in pill form, and new hormonal therapy drugs bring successful results.
WHAT CAN BE DONE TO REDUCE THE RISK OF DEVELOPING BREAST CANCER?
There is increasing evidence that physical activity in the form of exercise reduces the risk of breast cancer. Brisk walks of at least 1.25 – 2.5 hours per week reduce the risk of breast cancer in women by 18%. If this walking is 10 hours a week, the risk is slightly lower.
Some studies suggest that prolonged breastfeeding may slightly reduce the risk of breast cancer. Studies show that women who use the contraceptive pill have a slightly lower risk of breast cancer than women who do not use the pill. When the pill is stopped, the risk returns to normal. Women who have had many pregnancies and women who become pregnant at a young age have a reduced risk of breast cancer. This is due to the menstrual cycle stopping during pregnancy. Knowing which subgroup of breast cancer you are dealing with is very important for the success of the treatment.
LIFE AFTER BREAST CANCER
It is very important to plan a treatment model focused on the patient’s physical quality of life. In most patients, shoulder restriction and sometimes lymph edema occur after surgery (removal of axillary lymph nodes). Thanks to exercise and rehabilitation programs planned correctly and in the early period, these problems are eliminated. Thanks to lifelong follow-up programs, the possibility of permanent shoulder limitations and lymph edema can be greatly reduced.
Sexual and psychological problems, which are observed in almost 70% of breast cancer survivors, can be managed by specialists and problems that may develop in this direction can be eliminated. Exercises that have been continued throughout the disease should be resumed shortly after surgery and continued regularly. Most breast cancer recurrences occur within the first 3 years. For this reason, it is important for patients to follow up their health checks in detail for 3 years after the end of treatment. Since the recurrence rate of breast cancer is 30% at the surgical site and 70% in distant organs, it should not be neglected. Exercises that were continued throughout the disease should be restarted shortly after surgery and continued regularly.
During follow-up examinations, patients’ complaints are questioned and the patient is examined in detail. Patients with no complaints or suspicious findings do not require any examination. However, in patients with suspicious findings, detailed examinations are performed to clarify them.
With the treatment of breast cancer, patients should first of all open a new page for themselves and live without worry. During breast cancer treatment, shoulder shoulder restriction and sometimes lymph edema may occur due to the removal of the axillary lymph nodes. Thanks to exercise and rehabilitation programs planned in the right and early period, these problems can be eliminated.
Specialist help should be sought for sexual problems seen in 70% of breast cancer survivors. Sports such as exercise, yoga and walking should be continued after breast cancer surgery. There is a risk of recurrence of breast cancer within the first 3 years. For this reason, health checks should not be interrupted after overcoming the disease. Since the recurrence rate of breast cancer is 30% in the surgical field and 70% in distant organs, it should not be neglected.
FREQUENTLY ASKED QUESTIONS ABOUT BREAST CANCER
Breast Cancer Statistics
- In 2012, there were 1.7 million new cases of breast cancer worldwide.
- The top 3 countries with the highest incidence of breast cancer are Belgium, Denmark and France.
- Turkey ranks outside the top 20 countries with the highest incidence of breast cancer.
- Breast cancer accounts for 12% of all cancers.
- Breast cancer accounts for 25% of all cancers in women.
What is a Mass and Cyst in the Breast?
A palpable mass in the breast may be a cyst or a solid mass. Especially fibroadenomas and fibrocysts are very common masses in the breast. Coin-shaped breast masses are benign tumors that do not turn into cancer. Women cannot understand whether these masses they notice during breast self-examination are breast cancer or a harmless fibroadenoma mass. Fibroadenomas are very common especially in women under the age of 30 due to hormonal changes. The character of the mass in the breast can be understood by breast ultrasound. Therefore, women should see a specialist as soon as possible when they notice a change or a mass in their breasts. Breast ultrasound and, if necessary, mammography can provide an idea of the mass in the breast.
What does breast pain indicate?
Pain in the breast, especially if it is felt in both breasts, primarily indicates hormonal changes and the menstrual cycle. Fibroadenomas and fibro cysts can also cause pain in the breast. Pregnant women may experience breast pain due to hormonal changes, while breastfeeding women may develop breast pain due to breastfeeding. In advanced stages of breast cancer, edema and then pain in the breast may occur due to the growth of the tumor. However, pain in the breast is not considered a sign of breast cancer.
What to do when a mass is detected in the breast?
When a difference and change is felt in the breast during breast self-examination, it is necessary to consult a specialist doctor immediately. The diagnosis should be made by investigating what this mass is.
Is Every Mass Detected in the Breast Cancer?
Eight out of every 10 masses seen in breast cancer diagnosis may be benign. There may be non-cancerous masses called cysts seen at a young age, fibroadenoma and fibrocystic masses that can be seen in middle age. The fact that every mass in the breast is painful or painless does not mean that it is cancer.
How should nutrition be during breast cancer?
Diet during breast cancer has a positive effect on breast cancer treatment. After the diagnosis of breast cancer, breast cancer patients expect a nutrition list from the physician to prevent them from getting cancer again or to heal immediately and strengthen their defense system, and are disappointed when such a list is not given. Patients expect their physicians to recommend certain herbs and prescribe individual foods and their ratios under the misleading information created by false news reports, some private organizations marketing alternative medicine products and individuals.
According to research, special supplements for nutrition after a cancer diagnosis only cause the patient’s appetite to decrease, inadequate nutrition and weight loss. In addition, the dietary model recommended by nutritionists for all individuals, which emphasizes vegetables and fruits and increases the proportion of white meat and decreases the proportion of red meat, is sufficient for many cancer patients who are in good general condition and can eat well. Studies have shown that special nutritional supplements after a cancer diagnosis can only lead to a decrease in appetite, inadequate nutrition and weight loss.
In cases such as weight loss due to treatment and disease during breast cancer treatment, inability to take food by mouth, mouth sores, prolonged diarrhea, prolonged nausea and vomiting, and vitamin deficiency, special foods and vitamins and supplements should be administered intravenously or orally by special nutrition teams. Cancer patients should avoid overeating and salty foods! Early-stage breast cancer patients should avoid overeating and salty foods, especially during their treatment, and should be careful against the appetite-increasing, weight and edema-forming effects of cortisone, which is used to reduce allergic side effects before treatment.
In addition, high-calorie foods such as honey and molasses, which are consumed during this period in order not to be weak and weak, may cause excessive weight gain in patients, which is undesirable and extremely difficult to lose later. In the treatment of both breast cancer and all other cancers, there is no herbal product that has managed to enter the oncology literature as a scientific evidence other than the proven benefit of using Ginger 0.5-1mg orally as a pill for nausea and vomiting. Herbal products can harm patients. The use of vitamins, which have been popular in the last 20 years, has found an intensive area of use with the assumption that they will “keep us young, keep our skin smooth and protect us from side effects during cancer treatments” with their antioxidant properties. However, as a result of comprehensive studies conducted in the last 5 years, it has been determined that vitamins used unnecessarily and without the recommendation of a physician cause more harm than good to the body and even cause an increase in some types of cancer. As a result, the alternative medicine market and marketers in the world and in our country have turned their targets to herbal products. However, the undesirable interactions of these seemingly natural products, especially with chemotherapy and other medical treatments, put many patients and physicians in a difficult situation.
Can physical activity reduce the risk of breast cancer?
Exercise strengthens the immune system and helps keep your weight under control. A woman who exercises as little as three hours a week or about 30 minutes a day can reduce her risk of breast cancer.
Does eating too much sugar and sugary foods cause breast cancer?
Sugar is not directly linked to breast cancer. In order to prevent breast cancer, it is enough to pay attention to being at our ideal weight.
Should I stay away from crowded places during breast cancer treatment?
During breast cancer treatment, instead of avoiding crowded environments, you should be in environments where you are more likely to socialize and find morale. It is not possible to catch germs from crowded environments during the treatment process.
Do perfume, deodorant, laser epilation, permanent makeup cause breast cancer?
Laser epilation, permanent make-up, perfume, deodorant do not cause breast cancer.
When is the best time for a breast examination?
Breast examination should be done 4-5 days after the end of the menstrual period.
I have a family history of breast cancer. When should I have my first check-up?
You should have your annual routine ultrasound follow-up after the age of 25-26. In genetic breast cancers, the age for the first mammogram is 26. If you are at risk of familial breast cancer, you should be followed up with mammography after the age of 32-34.
Does mammography have an effect on cancer formation?
The benefits of mammography far outweigh the harm. Therefore, the radiation given off by mammography should never be considered as a harm to the body. In the 1960s, it was found that the harm of mammography was much lower than the benefit of mammography in patients who were followed up with mammography for 30 years in technologies with very high radiation rates. Mammograms give 10 times less radiation than the technologies of that period. Since there is no radiation in MRI, it does not have any side effects on the patient.
Is breast cancer contagious?
No cancer is contagious. The fact that many members of a family have cancer may be the reason for this misconception. One person cannot transmit cancer to another person. However, some cancers such as cervical cancer and liver cancer are caused by viruses.
Does a healthy and balanced diet reduce the risk of breast cancer?
You should take care to consume fresh fruits and vegetables rich in vitamins A and C, avoid animal fats and prefer more pulp foods, avoid smoked, salty and canned foods, avoid smoking and alcohol, and avoid excess weight gain. It is possible to reduce the risk of breast cancer by doing sports, using preventive medication in women with a high risk of breast cancer, evacuating both breasts in those with high risk factors, making breasts with silicone or from one’s own tissue, and not using tablets, creams and gels sold in the market under the name of ‘breast enlargement’.
Is it useful to do sports to reduce the risk of developing breast cancer?
You should prefer sports that are suitable for you in your daily life. For many people, the best sport is regular and brisk walking. In addition, you can choose exercises such as swimming, cycling, pilates, yoga, which you can do with a group or alone.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS NASOPHARYNX?
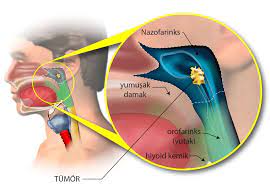
The transition area connecting the nasal cavity and the oral cavity is called the nasopharynx. It is the space that opens to the middle ear from both sides with the Eustachian tube. Since it is not a region that can be seen with the naked eye through the nose, it is visualized with an endoscope device through the nose. Or it can be seen through the mouth with a device called a mirror. Adenoid, which is common in children, also occurs in the nasopharynx region. Adenoids are benign lymphoid tissues that are formed as a defense mechanism of the body and are common in every child. Adenoid tissue seen in children up to a certain age is not expected in adulthood, and if lymphoid tissue is observed in the nasopharynx in an adult, a biopsy should be taken and sent for pathologic examination.
WHAT IS NASOPHARYNGEAL CANCER?
Cancers that occur in the nasopharyngeal region are called nasopharyngeal cancer. It is among the common types of cancer. Benign (benign) tumors and malignant (malignant) tumors can occur in the nasopharynx. If the patient is an adult, adenoid formation is not expected in this area. If an adult patient has a lesion or mass in the nasopharyngeal region, an examination should be performed. Nasopharyngeal carcinomas are frequently seen in the adult group. In addition, lymphoma and leukemia may also be frequently involved in this region in adults. Unlike adults, soft tissue (raptomyosarcoma) cancer or benign angiofibroma or plasmacytoma can also be seen in the nasopharynx region in children.
There are 3 types of nasopharyngeal cancer.
Type 1 Squamous cell nasopharyngeal carcinoma (SCC)
Type 2 Non-keratinized well-differentiated nasopharyngeal carcinoma
Type 3 Indifferentiated nasopharyngeal carcinoma
Nasopharyngeal cancer type 3 responds most quickly to treatment. It is unlikely to recur after treatment. Type 1 squamous cell nasopharyngeal carcinoma may recur after treatment.
Leukemia and lymphoma cancers can also be frequently involved in the nasopharynx region. For this reason, suspicious tissues seen in the nasopharyngeal region should be sampled and pathologically examined to determine whether the tissue is benign or a tissue with cancer risk.
WHAT ARE THE CAUSES OF NASOPHARYNGEAL CANCER?
Multiple factors may play a role in nasopharyngeal cancers. Environmental factors (air pollution, exposure to chemical vapors) genetic predisposition and viruses are among these factors.
Nasopharyngeal cancer, which is most commonly seen in adolescence at an average age of 40-50, affects men more.
A family history of nasopharyngeal cancer also increases the risk.
Epstein Barr virus (EBV) is closely associated with nasopharyngeal cancer. A nasopharyngeal examination should be performed in EBV positive people.
The incidence of nasopharyngeal cancer is also higher in smokers.
Dietary habits are also among the causes of nasopharyngeal cancer. Poor eating habits, excessive consumption of smoked foods, cooking on wood fire increase the likelihood of this disease.
WHAT ARE THE SYMPTOMS OF NASOPHARYNGEAL CANCER?
Masses in the neck are among the most common symptoms. Unilateral middle ear infections are also among the most common symptoms in adults. The Eustachian tube opens to the nasopharynx from both sides. When the mass closes any of these areas, unilateral otitis media may occur because ear ventilation is impaired. In unilateral ear infections in adults, the nasopharynx should be examined and the presence of a mass in this area should be checked. In general, patients have nasopharyngeal cancer;
Lymph node, mass in the neck
Nasal congestion
Nosebleeds
Persistent middle ear infection
Ear buzzing and ear congestion
Patients may consult a doctor with complaints of visual problems and pain due to cranial nerve involvement.
HOW IS NASOPHARYNGEAL CANCER DIAGNOSED?
In case of a suspicious condition in the nasopharyngeal region, physical examination is performed first. Then, if necessary, imaging techniques such as tomography, MRI and Pet CT are utilized.
The nasopharyngeal region can be seen through the nose with an endoscope device or through the oral cavity with a mirror. Normally the nasopharynx region has a flat structure. If there is a mass, swelling or difference in this area, the otolaryngologist should take a biopsy from this area. Nasopharyngeal cancer can sometimes involve the neck. These involvements can be clearly determined by medicated tomography or PET CT. The definitive diagnosis of nasopharyngeal cancer is made by biopsy. The type of the mass is determined in the biopsy. Treatment in nasopharyngeal masses is determined according to the type of mass; benign tumors can be surgically removed or followed up, if the result is nasopharyngeal cancer, the treatment option is primarily radiotherapy + chemotherapy.
WHAT IS THE TREATMENT OF NASOPHARYNGEAL CANCER?
The treatment of the mass whose type is determined as a result of the biopsy is carried out accordingly. Treatment of nasopharyngeal cancer is usually performed with radiotherapy + chemotherapy. Especially Type 3 Indifferentiated carcinoma is a type that responds quickly to radiotherapy. Treatment is successful with early diagnosis and regular follow-up.
Lymphoma and leukemia diseases can also involve the nasopharyngeal region. Radiotherapy and chemotherapy are also used in the treatment of these diseases.
If nasopharyngeal cancer is not caught and treated at an early stage, it can metastasize in the late stages. Since the nasopharynx region is close to the brain, skull base and nerve involvement can be seen frequently. It can especially involve the 6th, 3rd, 4th and 5th nerves. When it metastasizes to the skull base and nerves, the patient may experience double vision or fall.
The age and gender of the patient are among the factors that affect the course of treatment. In nasopharyngeal cancer, which affects men more, advanced age, lymph node involvement in the neck region, nerve involvement in the head region and cancer types not caused by Epstein Bar virus can adversely affect the course of treatment.
FREQUENTLY ASKED QUESTIONS ABOUT NASOPHARYNGEAL CANCER
How long does nasopharynx treatment take?
Nasopharyngeal treatment depends on the type of mass, whether it is a benign or malignant tumor, and is treated with surgery, radiotherapy or chemotherapy. The treatment is decided by otolaryngologists and oncologists. After these treatments, the patient should be followed up regularly by otolaryngologists and oncologists. The first 5 years after treatment are very important.
What is the nasal (nasopharynx) area?
The transition area connecting the nasal cavity and the oral cavity is called the nasopharynx. It is the space that opens to the middle ear from both sides with the Eustachian tube.
What is adenoid?
Adenoid occurs in the nasopharynx and is common in children. The benign, lymphoid tissues that form as the body’s defense mechanism are called adenoids. These tissues seen in children up to a certain age are considered normal tissues.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS A SPINE AND SPINAL CORD TUMOR?

After exiting the skull, the spinal cord runs through the bones of the spine until it reaches the coccyx. Benign or malignant tumors can develop in the spinal cord itself or in the surrounding membrane. Questions such as “What is a tumor in the spinal cord?”, “What is a tumor of the spinal cord bulb?”, “What is a tumor in the spinal nerve?” are among the topics that patients are curious about. Unlike spinal and spinal cord tumors, spinal bulb tumors are tumors that develop inside the brain. Tumors in the spine and spinal cord can be benign or malignant tumors. Most of the tumors that appear in the spine surrounding the spinal cord are the result of metastasis. Breast cancer, lung cancer and prostate cancer are the most common cancers that metastasize to the spine.
WHAT ARE THE SYMPTOMS OF SPINE AND SPINAL CORD TUMORS?
Questions such as “What are the symptoms of spine and spinal cord cancer?”, “How do the effects of spine and spinal cord tumors appear?”, “What are the first symptoms of spine and spinal cord tumors?”, “How to understand the symptoms of spine and spinal cord tumors?”, “How to understand the tumor in the back?”, “How to understand the tumor in the waist?” are among the topics that patients are curious about.
Symptoms of tumors originating from the spine and spinal cord may have a sudden onset or may progress slowly.
- The first symptom of a tumor of the spine and spinal cord can be weakness in the legs. In tumors that develop in the spinal cord itself or in the form of metastases in the spine, weakness in the legs occurs to a great extent due to compression of the spinal cord. This weakness may progress in untreated patients.
- The symptom of a sudden onset of a tumor of the spine and spinal cord is a sudden feeling of weakness. Symptoms such as paralysis and leg weakness can occur very quickly.
- Toilet problems such as incontinence of urine and large bowel movements can be a sign of a tumor of the spine and spinal cord. The first symptoms of a tumor of the spine and spinal cord can often be overlooked because they are similar to those of a herniated disc.
- Pain is a prominent symptom of slowly progressing tumors of the spine and spinal cord. Pain in the patient’s lower back can progress day by day. Spine or spinal cord tumors may be missed in poorly examined low back pain.
- In cases where the symptoms of spine and spinal cord tumors progress slowly, the tumor may even date back 5 years.
- In addition to these symptoms, symptoms related to the main focus of the cancer can also be experienced with metastatic tumors, which are usually seen on the spine. Symptoms such as weight loss, nausea, vomiting and loss of appetite may vary depending on the cancer causing the metastasis.
- In the presence of bone involvement in spinal tumors, symptoms such as pain and weakness may occur due to impaired strength of the spine.
- A feeling of numbness due to tumor pressure on the spinal cord can be a symptom of a tumor of the spine and spinal cord.
Symptoms of spine and spinal cord tumors in children are generally as follows:
Complaints such as pain and weakness should be taken into consideration, as children are not able to express their complaints more clearly than adults. Although not every pain or weakness reported by children should be considered as a spine or spinal cord tumor;
- If a toilet-trained child starts wetting the bed again, it is important to perform the necessary tests as a sign of spine and spinal cord tumor.
- When a child who walks, runs and plays normally starts to fall and walks with a wobble, it can also be a sign of a spine and spinal cord tumor.
Pain in children can be confused with growing pains.
WHAT CAUSES SPINE AND SPINAL CORD TUMORS?
Questions such as “Why do spinal and spinal cord tumors occur?”, “Why do spinal and spinal cord tumors occur?”, “What are the causes of spinal and spinal cord tumors?”, “How do spinal and spinal cord tumors occur?” are among the curious topics. The causes of spinal cord tumors are not known exactly. Although their physiopathology is not fully known, it is thought that they may be caused by genetic reasons. The majority of spinal tumors are metastatic tumors. The most common metastases are lung and breast cancer.
HOW ARE SPINE AND SPINAL CORD TUMORS DIAGNOSED?
“How to recognize a tumor of the spine and spinal cord?” is among the questions asked by patients. In general, spine and spinal cord tumors are diagnosed by radiological imaging and biochemical blood tests.
For the diagnosis of spine and spinal cord tumors, the doctor may order some radiological imaging after the examination,
- Radiography, i.e. X-ray
- Bone scan scintigraphy
- Computed Tomography (CT)
- Magnetic Resonance (MRI)
- In cases where the tumor is close to the surface, needle aspiration can be performed to determine which tissues it originates from or whether there are metastases. The piece taken with this method can be sent to pathology and the treatment can be shaped.
- Patients with symptoms of a tumor of the spine and spinal cord undergo blood tests to detect the presence of another tumor.
Radiological examinations using a special drug called contrast medium can reveal the location of the tumor as well as its size and the nerves it compresses.
Sedation or general anesthesia should be used to diagnose spine and spinal cord tumors in children. This method is preferred because it is difficult for children to remain still during Magnetic Resonance Imaging (MRI) or Computer Tomography (CT).
HOW IS SPINE AND SPINAL CORD TUMOR TREATMENT PERFORMED?
Questions such as “Can spine and spinal cord cancer be cured?”, “How is the treatment of spine and spinal cord tumor?”, “What are the treatments for spine and spinal cord tumor?”, “Is there a cure for spine and spinal cord cancer?” are among the curious topics.
- Surgery, radiotherapy and chemotherapy are generally used in the treatment of spine and spinal cord tumors. The treatment options and the order of treatment may vary depending on the patient, the type of tumor and its location. Planning is very important before starting treatment. Treatment can be shaped according to the patient’s condition, the size of the tumor and its location. In some patients, radiotherapy and chemotherapy are applied first, while in others surgical treatment comes to the fore.
- The treatment of spine and spinal cord tumors is carried out in a multidisciplinary approach consisting of different branches including medical oncology, radiation oncology, neurosurgery, interventional radiology and anesthesiologists experienced in neurosurgery.
- When starting treatment for a tumor of the spine and spinal cord, the patient’s spinal integrity should be assessed. The tumor may cause fractures in the spine and both the tumor tissue and the fracture may put pressure on the spinal cord. First of all, the patient’s spine structure must be stabilized. In order to stabilize the spine and to enable the patient to lead a social life as smoothly as possible, screw surgery, commonly known as platinum, which is actually titanium, can be applied.
- In the case of metastasized spinal tumors, it should be assessed whether the patient’s primary cancer is under control. If the patient has a long life expectancy, more effective treatments for tumors arising in the spine and spinal cord may be considered.
- In a small group of spinal tumors, which usually present as metastases, the entire tumor can be removed. In metastatic spinal tumors that cannot be completely removed, methods such as radiotherapy and chemotherapy can be used to make the patient’s social life more comfortable.
- For tumors originating from the spinal cord itself, the location is more important than how aggressive the tumor is. There is a big difference between surgery for a spinal cord tumor located in the neck and surgery for a spinal cord tumor located in the coccyx. Surgeries close to the neck have serious risks such as respiratory paralysis.
- In the treatment of tumors of the spine and spinal cord, high-tech radiotherapy devices can be used before or after surgery. Generally, positive results can be obtained in slowing the growth of benign tumors, stopping their growth and regressing them.
- Surgery of spine and spinal cord tumors is very delicate. Since it is a region where the nerves that run the whole body are located, advanced technology must be used in the surgery of spinal cord tumors. Neuromonitoring used in such risky surgeries can minimize possible complications.
- It is not always possible to remove the entire tumor in spine and spinal cord tumor surgery. If removal of the entire tumor would harm the patient, removal of the entire tumor should be avoided. Options such as radiotherapy and chemotherapy should be considered by removing the tumor to the maximum extent.
FREQUENTLY ASKED QUESTIONS ABOUT SPINE AND SPINAL CORD TUMORS
What are the types of spine and spinal cord tumors?
Tumors of the spine and spinal cord can be classified according to the tissues they originate from.
- Tumors originating from neurons, i.e. nerves, are tumors originating from the spinal cord itself.
- Tumors arising from the tissues and membranes surrounding the spinal cord.
- There may be tumors originating from the spine, i.e. the bone structure.
Tumors originating from the spinal cord itself are generally divided into two categories
- Astrocytoma
- Ependymoma
Where do tumors of the spine and spinal cord originate?
After exiting the brain, the spinal cord runs along the spine until it reaches the coccyx. Tumors of the spine and spinal cord can occur anywhere along this axis. Spine and spinal cord tumors can occur in the cervical spine or cervical spinal cord, the vertebrae surrounding the rib cage and the spinal nerves in this region, as well as in the lumbar region up to the coccyx. Most of the tumors on the spine are the result of metastasis. Some of the spinal cord tumors are more common in certain regions. Some types of spinal cord tumors seen in adults are more common in the neck region, while in children they can be seen in the spinal cord in the thoracic and lumbar regions.
How is spine and spinal cord tumor surgery performed?
- Spine and spinal cord tumor surgeries are performed as open surgery using microsurgery. Endoscopic method is not preferred in spine and spinal cord tumor surgery. Since two-dimensional images are obtained in endoscopic surgeries and a very small area is intervened, open surgery gives more successful results in spine and spinal cord tumor surgeries.
- First of all, if the spine or spinal cord tumor is in an accessible area, a needle aspiration biopsy is performed. This provides information about the type of tumor.
- The strength of the spine is checked. Any pressure on the spinal cord is assessed. If necessary, a method called spinal screwing is used to ensure the stability of the spine.
- The biggest problem for patients with spinal tumor metastases is pain. In some patients, it may not be possible to operate on the tumor. In these cases, surgical methods can be applied to relieve the patient’s pain.
- For tumors originating from the spinal cord itself, the tumor is removed by open surgery using microsurgical methods. In spine and spinal cord tumor surgery, the risks that may occur should be minimized by using the most advanced technology possible. The neuromonitoring device used in these operations warns the neurosurgeon about risky areas during the operation.
- The tissues removed during surgery for tumors of the spine and spinal cord are sent to pathology to shape the treatment.
How many hours does spine and spinal cord tumor surgery take?
Spinal cord tumor surgery takes approximately 4-5 hours. In some tumors, surgical methods such as removing the spine and re-stabilizing it can be applied. Depending on the location, size and type of the tumor, the operation may take up to 12-15 hours. Depending on the location and size of the tumor, neurosurgeons may be accompanied by cardiac surgeons, general surgeons or urologists.
What are the risks of spine and spinal cord tumor surgery?
- Tumors of the spine and spinal cord are prone to bleeding. In some cases, interventional radiology specialists may perform vascular procedures before surgery to reduce bleeding during the surgical procedure. .
- As with all surgeries, there is a risk of infection in spine and spinal cord tumor surgeries.
- Especially in the case of extensive tumors, there is a risk of internal organ damage, damage to large vessels, injury to the kidneys or urinary tract.
- Paralysis is among the risks of spine and spinal cord tumor surgeries. However, this risk is minimized with the advanced technology used in surgeries.
- As a result of the nerves being affected, problems such as urinary incontinence and incontinence can be seen.
Is there pain after spine and spinal cord tumor surgery?
Patients may experience severe pain after spine and spinal cord tumor surgery. However, this is taken into consideration before surgery and the use of strong painkillers is planned.
What happens if spine and spinal cord tumor surgery is not performed?
Not undergoing spine and spinal cord tumor surgery or postponing other treatments will cause the tumor to progress. The symptoms of a tumor of the spine and spinal cord progress day by day. At first, the tumor may cause pain in one leg, but later it may also affect the other leg. Tumor-related complaints begin to appear sequentially and the process can progress to paralysis. Depending on the location of the tumor, paralysis can affect the neck or lower back.
Is there a herbal treatment for spine and spinal cord tumors?
There is no scientifically proven herbal or natural treatment for spine and spinal cord tumors.
What should be considered after spine and spinal cord tumor surgery?
- Omurga ve omurilik tümörün ameliyatından sonra yapılacak patolojik işlemle tümörün cinsi belirlenmeli ve hastaya buna göre bir tedavi protokolü uygulanmalıdır. Cerrahi işlemden sonra kontrollerin ihmal edilmemesi önemlidir.
- Medication should not be neglected.
- In terms of nutrition, a balanced diet in terms of protein, carbohydrates and fats should be taken care of.
- Wound care and keeping the wound clean is important for infection risk.
Which department should I go to for spine and spinal cord tumor surgery?
Patients are also curious about which department to go to for spine and spinal cord tumor surgery. Symptoms of spine and spinal cord tumors can often be confused with herniated discs. For this reason, patients go to the neurosurgery department because of the symptoms that have already appeared. This is the same department that should be visited for spine and spinal cord tumor surgery. In order to minimize the problems that may occur both during and after spinal and spinal cord tumor surgeries, it is necessary to prefer well-equipped hospitals.
How long does it take to recover after spinal cord tumor surgery?
Recovery after spine and spinal cord tumor surgery may vary depending on the type of tumor, its location and the patient’s response to the treatment. In general, patients can return to their social life approximately 3 weeks after spine and spinal cord tumor surgery.
What is the treatment of benign spinal cord tumor?
Chemotherapy and radiotherapy are not used in the treatment of benign spinal cord tumors. Most benign spinal cord tumors can be completely removed surgically. In these patients, they can continue their normal lives after surgery without the need for any other treatment. However, in spinal and spinal cord tumors caused by some genetic diseases, multiple tumors may occur. In such cases, the number of tumors may increase over the years. Even if the tumor is surgically removed, it may recur after a certain period of time.
Are tumors of the spine and spinal cord dangerous?
Questions such as “Is a tumor of the spine and spinal cord fatal?”, “Is there a risk of death from a tumor of the spine and spinal cord?”, “How many years does a tumor of the spine and spinal cord live?”, “Does a tumor of the spine and spinal cord kill?”, “How long does a tumor of the spine and spinal cord live?”, “What is the life expectancy of a tumor of the spine and spinal cord?” are among the topics that patients are curious about.
Spinal tumors are usually metastatic tumors originating from a different cancer. In these patients, there are situations that differ from patient to patient depending on the response to treatment.
In cases of rapid spread in brain tumors, it is possible to lose the patient, but spinal cord tumors differ from other tumors in this respect. If the spinal cord tumor is located close to the brain, heart or respiratory center, there is a risk of death. However, other than this, spinal cord tumors may not cause the patient’s death, but may cause paralysis over time if left untreated. The patient can continue his/her life even if he/she has a spinal cord tumor, but if he/she does not receive the necessary treatments, he/she faces the risk of not being able to use his/her limbs over time and paralysis from the neck or waist down, depending on the location of the tumor.
Does a spinal cord tumor metastasize?
Tumors that develop in the spinal cord usually do not metastasize. If some childhood brain tumors are in the cerebrospinal fluid circulation pathway, there may be tumor flow towards the spinal cord. However, tumors originating from the spinal cord itself usually do not metastasize.
Do spine and spinal cord tumors cause leg pain?
The first symptom of a tumor of the spine and spinal cord is usually leg pain or weakness in the legs. In the absence of the necessary treatment, the problem may spread to both legs over time.
Does a tumor of the spine and spinal cord cause headaches?
The symptoms caused by tumors of the spine and spinal cord are usually related to the area of involvement. Therefore, tumors of the spine and spinal cord do not cause headaches.
What are the stages of spinal cord cancer?
The staging of spine and spinal cord tumors is generally in 4 stages, as in other cancers.
Can spine and spinal cord tumors cause paralysis?
Spine and spinal cord tumors can cause paralysis. Spine and spinal cord tumors, especially those that are left untreated or delayed in treatment, can cause paralysis over time, or they can develop suddenly and cause paralysis. Depending on the location of the spine and spinal cord tumor, paralysis may develop from the neck down or from the waist down.
Is physical therapy applied for spine and spinal cord tumors?
Physical therapy can be used to support the treatment of spine and spinal cord tumors. If patients have experienced loss of function in their hands or feet after surgery, positive results can be obtained with physical therapy.
Is radiotherapy applied for spine and spinal cord tumors?
Radiotherapy can be used in the treatment of spine and spinal cord tumors. This may vary depending on the condition of the patient and the tumor. In some patients, radiotherapy may be used before surgery, while in others it may be preferred after surgery. Positive results can be obtained with advanced technology radiotherapy devices.
Is spine and spinal cord tumor medication used?
It is possible to use medication in two ways in the treatment of spine and spinal cord tumors. If chemotherapy is to be applied in the treatment planning, medication can be used for the pain experienced as well as the medications prescribed by a specialist oncologist.
Can spine and spinal cord tumors be detected by blood tests?
Spinal tumors, which are usually caused by metastases, can be detected by blood tests, but tumors originating from the spinal cord itself cannot be detected by blood tests. Radiological methods such as Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) are used to diagnose these tumors.
Do tumors of the spine and spinal cord recur?
Some benign spinal cord tumors with a genetic predisposition can recur. Malignant tumors can also recur in the same area.
What can be done for pain in patients with spine and spinal cord tumors?
Spine and spinal cord tumors are controlled with strong painkillers both before and after surgery. However, in some patients, surgical procedures based on cutting the nerve causing the pain can be applied for pain that cannot be relieved with painkillers. In this case, the patient can continue his/her normal life but does not feel the pain.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS ESOPHAGEAL CANCER?

Cancers that occur in the esophagus, which is about 25-30 cm long and extends from the neck to the stomach, are called esophageal cancer or esophageal cancer.
WHAT ARE THE SYMPTOMS OF ESOPHAGEAL CANCER?
The most important symptom of esophageal cancer is difficulty swallowing. Symptoms of esophageal cancer include a feeling of getting stuck and painful swallowing. In cases where the tumor does not cover 60-70% of the esophagus, it usually does not cause symptoms. Since esophageal cancer symptoms appear very late, the tumor can be detected in advanced stages in most patients. In elderly people, drooling on the pillow at night and pain when swallowing may be the first symptoms of esophageal cancer.
The symptoms of esophageal cancer may differ depending on the site of the tumor.
Difficulty swallowing is a common symptom of esophageal cancers in all regions
- Another symptom of esophageal cancer that occurs close to the neck area may be hoarseness.
- A cough can be a symptom of esophageal cancer that occurs in the middle of the chest.
- The symptom of esophageal cancer that occurs in the lower region close to the stomach can be severe reflux.
Among the symptoms of esophageal cancer, bleeding can sometimes be seen, although very rarely. This bleeding is seen as intestinal bleeding rather than blood from the mouth.
Esophageal cancer can give different symptoms according to its stages.
- Stage 1 esophageal cancer may be asymptomatic. Detection of esophageal cancer at Stage 1 is usually by chance or as a result of scans.
- The symptom of stage 2 esophageal cancer may be difficulty swallowing. Although rare, symptoms of esophageal cancer at this stage may include a feeling of sticking and intestinal bleeding.
- In stage 3 esophageal cancer, the symptom is severe difficulty swallowing. The patient becomes unable to eat solid food. Salivation may occur mostly in older people.
- The symptoms of stage 4 esophageal cancer may differ depending on the site of metastasis. In stage 4 esophageal cancer, severe weight loss is among the first symptoms. Cough may occur if the tumor has invaded the trachea. If it has spread to the liver, side pains may occur. If it has spread to the bones, bone pain may occur.
WHAT ARE THE CAUSES OF ESOPHAGEAL CANCER?
The causes of esophageal cancer vary according to the cell type.
Squamous cell (squamous) is among the causes of esophageal cancer;
- Alcohol and smoking
- Consuming excessively hot drinks
- Consumption of burnt and smoked foods.
Adenocarcinoma esophageal cancers are usually caused by reflux. About 20% of the population has reflux, but not all reflux patients will develop esophageal cancer. Long-term reflux (acid and bile), combined with alcohol and smoking, can cause Barrett’s esophagus (BARRETT). Barrett’s esophagus is an important risk factor for esophageal cancer.
A significant part of the causes of esophageal cancer are preventable factors. Apart from this, some diseases and genetic factors are very rare.
Eating a meat-heavy diet and consuming a lot of burnt foods prepared on barbecue are among the risk factors for esophageal cancer, as in stomach and colon cancer.
DIAGNOSIS OF ESOPHAGEAL CANCER
How to recognize esophageal cancer?
Esophageal cancer is diagnosed by endoscopic control. With endoscopic imaging, it may be sufficient for the doctor to see the inside of the esophagus for diagnosis. However, in order to confirm the diagnosis of esophageal cancer, a pathological examination of the taken piece is required.
Endoscopic ultrasound imaging method called EUS is used to determine the stage of esophageal cancer, i.e. how far it has progressed in the esophageal wall. EUS provides important information to determine the stage of esophageal cancer.
In addition, every patient who will undergo treatment or esophageal cancer surgery should have Computed Tomography and Pet CT examinations.
WHAT IS ESOPHAGEAL CANCER TREATMENT?
The treatment of esophageal cancer varies according to its stage and location.
In adenocarcinoma or squamous cell (squamous) stage 3 esophageal cancers, a treatment called chemoradiotherapy, which combines chemotherapy with a not very high dose of radiotherapy, is primarily applied. Significant responses are obtained from this treatment. Esophageal cancer surgery is performed in patients who become suitable for surgery with chemoradiotherapy treatment.
In stage 4 esophageal cancers, surgery is usually not possible. This patient group is treated with chemotherapy and radiotherapy.
In stage 1-2-3 esophageal cancers, treatment is planned for the area where the tumor is located.
Treatment of esophageal cancers in the neck region
When cancer is located in the neck region of the esophagus, patients are usually not treated with surgery. Studies have shown that there is no difference between surgery or chemoradiotherapy treatment for esophageal cancers in the neck region. In esophageal cancers that occur in the neck region, chemoradiotherapy method achieves significant success in a significant proportion of patients.
However, surgery is preferred in cases where chemotherapy and radiotherapy are not sufficient.
Since the tumors in the neck region of the esophagus are behind the voice box, the larynx, thyroid, part of the pharynx and part of the trachea are also removed in these operations, and the patients have to breathe through their neck for the rest of their lives.
In esophageal cancer surgery, only a part of the esophagus is removed and an esophagus can be made from the small or large intestine so that the patient can feed through his mouth. Sometimes the esophagus can be completely removed and an esophagus can be made from the stomach to the root of the tongue.
Treatment of esophageal cancers in the chest
In the treatment of tumors that occur in the thoracic region, that is, in the middle of the esophagus, the treatment varies depending on whether the tumor is above or below the area where the trachea is divided into two. If the tumor is above the trachea, chemoradiotherapy treatment is preferred. When the tumor is below the trachea, surgery is preferred.
In esophageal cancer surgery in the thoracic region, the entire esophagus is removed along with the lymph nodes (at least 16). Afterwards, an esophagus can be made from the stomach and the patient can be fed through the mouth.
Treatment of esophageal cancers close to the stomach
In esophageal cancers in the lower esophagus, i.e. in areas close to the stomach, treatment is planned according to the spread of the tumor to the stomach.
In cases where the tumor has spread 2 cm or more into the stomach, a significant part of the esophagus and the entire stomach must be removed. These patients need to have a new esophagus made from the small or large intestine. These patients need to follow a special dietary regimen and consume less and less food. However, it is possible for them to eat almost everything.
FREQUENTLY ASKED QUESTIONS ABOUT ESOPHAGEAL CANCER
Who is more likely to get esophageal cancer?
Esophageal cancer ranks 7th among the most common cancers. While 30-40 thousand new patients emerge in our country every year in the most common lung cancer, 4-5 thousand new patients are seen in esophageal cancer every year.
In Turkey, squamous type esophageal cancer, also known as squamous cell esophageal cancer, is more common in Eastern regions such as Erzurum, Ağrı, Kars, Van, Bitlis and Muş due to dietary habits. Drinking very hot tea and eating a meat-based diet poor in vegetables play an important role in the incidence of esophageal cancer in this region. Squamous cell esophageal cancer is more common in the region starting from the east of Turkey and extending all the way to China, including the Turkic Republics. Since the region is mountainous and cold, excessive consumption of hot drinks is an important factor. When smoking and alcohol are added to the consumption of hot drinks, the incidence of esophageal cancer increases.
Generally, esophageal cancer is a disease over the age of 60, it is less common under this age. Although it is more common in men, it can occur at almost the same rate in women in our Eastern provinces due to hot tea drinking. Esophageal cancer, which is rare in the young population, can be seen more frequently in people with a family history of esophageal cancer and colon cancer.
What are the Types of Esophageal Cancer?
Esophageal cancer is classified according to the cell type it originates from and the region where it occurs. Esophageal cancer is generally divided into squamous cell (squamous) and adenocarcinoma esophageal cancer.
- Squamous cell esophageal cancer: Cancer that originates from the thin membrane tissue made of flat cells lining the inside of the esophagus. Squamous cell esophageal cancer is more common in Turkey.
- Adenocarcinoma is cancer of the esophagus: When the mucosa (i.e. the inner membrane layer) in the lower part of the esophagus is exposed to stomach acid and bile, it changes shape and begins to resemble glands and the inner lining of the stomach. It is cancer caused by cells that change into this shape. In Western countries, adenocarcinoma type esophageal cancer is more common than squamous esophageal cancer.
Apart from these two types of esophageal cancer, different types originating from muscle tissue are very rare.
In addition to differentiating esophageal cancer according to the cells it originates from, it is also possible to differentiate it according to its location in the esophagus.
- On the neck
- Intra-thoracic Esophagus
- Lower end – Stomach Inlet
Because the damage from stomach acid and bile reflux is close to the stomach, adenocarcinoma esophageal cancer usually occurs at the entrance to the stomach or in the lower part of the esophagus. Squamous esophageal cancer, on the other hand, occurs in the upper or middle part.
Can esophageal cancer be detected by a blood test?
Esophageal cancer is not detected by a blood test.
What should be done for early diagnosis of esophageal cancer?
There is no screening program for early diagnosis of esophageal cancer in Turkey. However, one of the most important measures that can be taken personally is to have endoscopic controls.
In patients with Barrett’s esophagus (BARRETT), which develops due to reflux, it is important to follow up with annual endoscopy for early diagnosis of esophageal cancer that may develop.
In Eastern provinces where squamous cell esophageal cancer is common, routine endoscopic controls are vital for early diagnosis.
What are the Stages of Esophageal Cancer?
Esophageal cancer consists of 4 stages.
- Esophageal cancer stage 1: Stage 1 esophageal cancer is very difficult to diagnose because the symptoms of esophageal cancer appear very late. The disease is only in the inner lining of the esophagus. It has not reached the muscle structure. In the treatment of stage 1 esophageal cancers, it is possible to remove only the diseased membrane by entering the mouth with an endoscope instead of completely removing the esophagus.
- Esophageal cancer at home 2: In stage 2 of esophageal cancer, the disease has crossed the membrane and reached the muscle tissue.
- Esophageal cancer stage 3: The tumor is not very small. The disease is in the esophagus but has also spread to the surrounding lymph nodes. In the treatment of stage 3 esophageal cancer, chemotherapy and radiotherapy are applied first. The aim is to regress the tumor and the disease in the lymph nodes. If regression is achieved, the tumor must be removed for surgery.
- Esophageal cancer stage 4: In stage 4 esophageal cancer, the tumor has metastasized to distant parts of the body. Esophageal cancer most commonly spreads to the liver, bone, lung and lymph nodes at the entrance of the stomach. At this stage, there is little chance of surgery. Treatment with chemotherapy is applied.
Which Department and Doctor Should I Visit for Esophageal Cancer?
A significant number of esophageal cancer patients undergo a treatment process in which many departments act in cooperation. In esophageal cancers that require a multidisciplinary treatment approach, besides thoracic and esophageal surgery; gastroenterology, medical oncology, radiation oncology and general surgery can work together. The support of the diet and nutrition department is very important in this process. In cases requiring specialized microsurgery (for example, making an esophagus from the small intestine), support from the Aesthetic, Plastic and Reconstructive Surgery Department is also received. Since there are very specialized surgical approaches in the treatment of esophageal cancer, it is important to choose hospitals with experienced doctors and adequate infrastructure.
How is esophageal cancer surgery performed?
As in intestinal surgeries, a part of the esophagus cannot be cut and combined with the rest of the esophagus. A new esophagus must be made instead of the esophagus removed by surgery. The main purpose is to ensure intestinal continuity. When the esophagus is removed, cancer of the stomach, small and large intestine or, in rare cases, esophageal cancer through the skin can be performed.
Very rarely, in cases where the tumor is not removed, the continuity of the intestine can be ensured from the side and the patient can eat through his mouth. Thanks to the developing technology, this situation can now be resolved by stenting.
In cases where a completely obstructed tumor cannot be removed and a stent cannot be placed, a tube (gastrostomy) can be inserted into the stomach to provide nutrition and food can be fed directly into the stomach.
How is Closed Esophageal Cancer Surgery Performed?
In our Esophageal Diseases Center, the majority of esophageal cancer surgeries (80-90%) are performed closed. Worldwide, closed esophageal cancer surgeries are performed through 6 holes in the chest and 4 holes in the abdomen. At Memorial Ataşehir Hospital Esophageal Diseases Center, closed esophageal cancer surgery can be performed through 3 holes in the abdomen and a single hole in the chest. The abdominal part of the surgery takes 45 minutes-1 hour and the chest part 1-1.5 hours. Closed esophageal cancer surgery reduces the amount of bleeding, duration of surgery and trauma and reduces complications that may develop.
What are the Risks of Esophageal Cancer Surgery?
Esophageal cancer surgery is one of the most important operations of the body. The most important risk is leakage in the junction area between the esophagus and the stomach or the intestine, which is the new esophagus. There is also a risk of hoarseness in esophageal cancer surgery. However, this risk is less than 10% and hoarseness is usually temporary. In long-term hoarseness, hoarseness can be relieved with a small procedure. As a result of a major surgery, pneumonia, heart rhythm disturbances and lymph leakage may occur.
Does Esophageal Cancer Kill?
Cancer evokes death in people’s minds. Therefore, doctors often encounter the question “Does esophageal cancer kill?”. A significant portion of stage 1, stage 2 and some stage 3 patients who can be operated have a chance to recover from the disease. However, esophageal cancer is a disease that progresses without symptoms. Symptoms become apparent only in Stage 4.
There is no general answer to the question of whether esophageal cancer kills. Each disease has individualized conditions. Life expectancy varies according to many criteria such as the type of tumor, the stage of the tumor and the location of the tumor, as well as the age of the patient and the presence of concomitant diseases.
In studies conducted independently of these, 5-year survival rates in esophageal cancer are as follows;
Stage 1 esophageal cancer 80-90
Stage 2 esophageal cancer 50-60 percent
Stage 3 esophageal cancer 30-40
Stage 4 esophageal cancer 5
If the disease does not return in the first 2-3 years, it usually does not recur. Therefore, the first 2-3 years after treatment are very important.
Is there a herbal treatment for esophageal cancer?
There is no herbal treatment for esophageal cancer. However, it is very important to eat a vegetable-based diet and consuming foods such as onion garlic and turmeric, which are anti-inflammatory plants, can provide support in the fight against cancer.
Sugar-heavy foods such as molasses, honey, sugary sweeteners, sherbet desserts should be avoided. Instead, it is important to consume protein and vegetable-based foods.
Things to Consider After Esophageal Cancer Surgery
After esophageal cancer surgery, patients should pay attention to the foods they consume. While consuming anti-inflammatory foods and avoiding sugar, quality sleep, exercise and regular health checks should not be neglected.
Acidic drinks should be avoided after esophageal cancer. Patients should use gastric protection medication for life.
Since the postoperative food enters directly into the stomach, patients experience 10% weight loss due to problems in absorption and sometimes sudden diarrhea depending on the type of food. To avoid problems, patients should avoid foods such as honey molasses and syrupy desserts. It is necessary to eat little and often. Patients are usually restricted not in terms of food but in terms of quantity.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS PENILE CANCER?
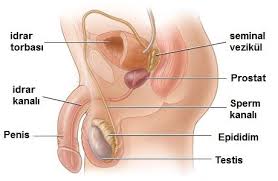
WHAT IS A PENIS AND WHAT IS IT FOR?
The penis is part of the male reproductive and urinary systems. The main structures of the male reproductive system are the testes, epididymis, seminal vesicles, prostate and penis. The inner parts of the male reproductive system are located in the lower pelvic cavity between the hip bones. The penis hangs in front of the skin sac (scrotum) where the testes are located. The penis has three main parts: the root, the shaft and the glans, which is the cone-shaped end of the penis. The glans is covered with a layer of skin called the foreskin. When the penis is stimulated, the penile arteries dilate and the muscles contract. This causes an erection, which is necessary for sexual intercourse. The urethra is also part of the urinary system. It carries urine from the bladder to the outside of the body. There is a valve (sphincter) at the root of the penis that, when relaxed, allows urine to flow out of the urethra and out of the body.
WHAT IS PENIS CANCER?
Cancer that starts in the cells in the penis is called penile cancer. The vast majority of penile cancer cases (about 95 percent) are squamous cell carcinoma. This means that the cancer starts in the squamous cells of the penis. Most squamous cell carcinoma of the penis starts on the foreskin or the tip of the penis (glans). Squamous cell penile cancer typically grows slowly. Treatment has a high success rate when detected early. Other types of penile cancer include basal cell carcinomas, sarcomas, melanomas or urethral carcinoma. Penile cancer, one of the rarest types of cancer, usually occurs in uncircumcised men, mostly in Africa, South East Asia and South America.
WHAT ARE THE RISK FACTORS FOR PENILE CANCER?
Risk factors associated with penile cancers generally include the following:
- Not being circumcised Penile cancer is more common in uncircumcised men than in circumcised men. Neonatal circumcision can almost completely eliminate the risk of penile cancer.
- Age: The majority of cases of penile cancer occur in men aged 50-70 years. About a third occur in men under the age of 50.
- Smoking-Tobacco use
- Human papillomavirus (HPV): HPV 16 and HPV 18 are linked to penile cancer.
- Phimosis Phimosis is a factor that makes it difficult to retract the foreskin. This means that the foreskin cannot be pulled back to the head of the penis (glans). This can lead to a buildup of body fat, bacteria and other debris known as smegma.
- UV light therapy for psoriasis: UV light therapy for some skin diseases, such as psoriasis, can increase the risk of developing penile cancer.
- AIDS (acquired immune deficiency syndrome)
WHAT ARE THE SYMPTOMS OF PENILE CANCER?
The most common symptoms of penile cancer include changes in the color or thickness of the skin, unusual discharge, ulcers, pain and swelling at the tip of the penis. While symptoms of penile cancer can vary from person to person, general symptoms include the following in summary:
- Changes in the skin of the penis, pain at the tip of the penis
- Painful or painless wart-like growth or lesion
- Open wound that does not heal
- Bleeding under the foreskin
- Reddish rash
- Small tubers
- Flat, bluish-brown growth
- Persistent, odorous discharge under the foreskin
- Swollen lymph nodes in the groin when the cancer has spread
HOW IS PENIS CANCER DIAGNOSED?
If the doctor suspects penile cancer, he/she will order a biopsy. Because the definitive diagnosis of penile cancer is made with a biopsy. A biopsy involves removing some tissue from the penis or lymph nodes and examining it in a laboratory.
There are three types of biopsy procedures that can be performed;
Incisional biopsy involves removing only part of the abnormal tissue. It is usually performed for larger lesions, wounds, ulcerations and lesions that appear to be deepening into the tissue.
An excisional biopsy removes the entire lesion or abnormal growth. Excisional biopsy is usually done when the abnormal area is small.
Lymph node biopsy is usually done when penile cancer has invaded tissues inside the penis. It will help the doctor find out if the cancer has spread beyond the penis tissue. Usually, a lymph node biopsy is done by fine needle aspiration (FNA), a procedure in which the doctor inserts a thin needle into the lymph node(s) and pulls out cells and fluid to find out if there is cancer in the lymph node(s). In some cases, all lymph nodes are surgically removed to check for cancer.
Imaging tests can also help doctors diagnose and stage penile cancer. Here are some of the imaging tests used to diagnose and stage penile cancer:
- CT scan (computed tomography scan)
- MRI (Magnetic resonance imaging)
- Ultrasound
WHAT IS THE STAGING OF PENILE CANCER?
Staging of penile cancer is as follows:
Stage 0
Only the top layer of the skin of the penis shows signs of cancer. In other words, it is superficial and does not spread.
Stage 1
The cancer has grown into the tissue under the top layer of skin on the penis. However, there is no involvement of the lymph and blood vessels.
Stage 2
At this stage, the cancer continues to spread beyond the skin and tissue of the penis. It is present in the nerves, lymph vessels or blood vessels.
Stage 3
In stage 3, the cancer may have spread to the spongy erectile tissue of the penis. The cancer may also have spread to the lymph nodes in the groin.
Stage 4
At this stage, the cancer may have spread to the scrotum, prostate, pubic bone and other structures in the groin. Cancer may also be present in the lymph nodes.
WHAT ARE THE TREATMENT METHODS FOR PENIS CANCER?
Treatment methods for penile cancer usually include surgical procedure, radiotherapy and chemotherapy. These treatment methods can be applied alone or in combination, depending on the stage of the disease, the type of cancer and the general health of the patient.
Surgical procedure
The main treatment for penile cancer is surgery. In the surgical procedure, the tumor and some surrounding healthy tissue (margin) will be removed. The extent and type of surgery depends on the location, type and stage of the tumor. In most cases, any physical changes to the penis that occur following the surgical procedure can be corrected with reconstructive surgery.
Photodynamic therapy (PDT)
Photodynamic therapy uses special drugs called photosensitizing agents in combination with light to kill cancer cells. The drugs only work after they have been activated or turned on by light.
Cryosurgery
Cryosurgery uses liquid nitrogen to freeze and kill cancer cells.
Radiotherapy
Radiotherapy uses high-energy x-rays to destroy cancer cells. The advantage of radiotherapy is that it preserves the anatomical structure of the penis. The disadvantage is that penile cancers are relatively resistant to radiotherapy and can cause many complications such as fistula, edema, skin necrosis and pain.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells or slow their growth. Chemotherapy has a limited role in the treatment of penile cancer: Chemotherapy is mostly used when the cancer has spread to the lymph nodes and other tissues. In patients with fixed inguinal metastases, about 50 percent of which can be resected, primary neoadjuvant chemotherapy may have a role.
On the other hand, circumcision and laser surgery may be therapeutic for very small foreskin lesions. Although laser therapy offers the advantage of preserving the penis, the depth of laser penetration is shallow.
FREQUENTLY ASKED QUESTIONS ABOUT PENILE CANCER
How does penile cancer affect a man’s sexuality?
A man diagnosed with penile cancer may have a partial (removal of some intact penile tissue along with cancerous tissue in the penis) or complete penectomy (removal of the entire penis). The side effects of a surgical procedure to treat penile cancer can be difficult to cope with. A man may need psychological support to cope with the loss of part or all of his penis.
Does circumcision prevent penile cancer?
Penile cancer is almost never seen in men circumcised as newborns. The incidence of penile cancer is higher when circumcision is delayed until after puberty. Adult circumcision does not protect against penile cancer.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS SALIVA AND SALIVARY GLAND?
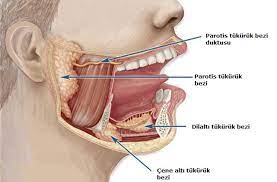
Saliva is a type of fluid produced in the mouth and is important for our body because it contains substances with important functions such as water, sodium, chloride, calcium, potassium, bicarbonate, immune globulin A, albumin, ptyalin and mucin. Saliva keeps the mouth constantly moist, lubricates the food in the mouth and dissolves some molecules in the food so that they reach the taste buds. It facilitates swallowing and also facilitates speech by freeing the movements of the tongue and lips. It keeps the teeth and the inside of the mouth clean by constantly washing them.
Saliva secretion is made by salivary glands. In addition to the 400-600 minor salivary glands located in the oral cavity, nose, sinuses, pharynx, larynx, trachea and bronchial mucosa, we also have large salivary glands located on each side of our face and connected to the oral cavity by small ducts. These are 6 in total, one in front of each ear (Parotid gland), one under each chin (Submandibular gland) and one under each tongue (Sublingual gland).
WHAT DOES THE SALIVARY GLAND DO?
Salivary glands produce saliva secretion. It is known that a healthy person produces 1000-1500 cc of saliva daily. Salivary glands ensure the cleanliness in the mouth, the acid and the transportation of food to the stomach. Saliva, which has many functions from bad breath to digestion, is very important for health.
WHAT IS SALIVARY GLAND CANCER?
Salivary gland cancer is a condition that occurs as a result of cancerization of one of the salivary glands, which we call large (three pairs) and small (about a thousand), that secrete saliva in our mouth.
WHAT ARE THE TYPES OF SALIVARY GLAND TUMORS?
Tumors are divided into benign (benign) and malignant (malignant). Benign tumors grow more slowly and do not metastasize (spread) to surrounding or distant organs. Malignant tumors, on the other hand, grow faster and have the potential to metastasize (spread) to regional lymph nodes and distant organs (lung, liver, brain, bone, etc.).
WHAT ARE THE SYMPTOMS OF SALIVARY GLAND CANCER?
Slower growing benign tumors are often surrounded by a thin, membranous sheath called a capsule and do not invade surrounding tissues. They usually grow by pushing the surrounding tissues and making room for themselves. This growth occurs over months or even years. Benign tumors do not cause pain and patients rarely complain of pain. Pain is usually due to indirect causes rather than the tumor itself.
Malignant tumors grow faster and have the potential to metastasize (spread) to regional lymph nodes and distant organs (lung, liver, brain, bone, etc.). They spread to surrounding tissues and develop by disrupting their function. For example, when they reach the nerves adjacent to their location, they disrupt their function. Malignant tumors also start to cause pain after they reach a certain size. This pain may occur due to the tumor invading structures such as bones and jaw joints, or it may occur directly in the head and face or by reaching the nerves that carry pain sensation.
WHAT ARE THE CAUSES OF SALIVARY GLAND CANCER?
Although the causes of salivary gland cancers are unknown, some conditions are thought to increase this risk. The most important of these is when benign tumors remain in the salivary gland for a long time. Therefore, even if the tumor is known to be benign, it is preferred to remove it from the salivary gland. Radiation exposure is also one of the reasons that increase the possibility of salivary cancer. Smoking increases the likelihood of salivary gland cancer, as it increases the likelihood of most cancers.
HOW IS SALIVARY GLAND CANCER DIAGNOSED?
Early diagnosis of salivary gland cancers is usually based on the complaints of the patient. The disease can be diagnosed with detailed examinations made as a result of consulting a doctor with complaints such as swelling or pain in the head-neck region.
After a detailed anamnesis, the patient is examined. In the physical examination, it is checked whether there is swelling and enlargement in the salivary glands, and if there is growth and swelling, the size and boundaries of the swelling are examined. Bilateral, that is, bilateral examinations should be compared with bilateral examinations.
Imaging methods are also used in salivary gland cancers. Especially Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are used to examine tumor tissue and surrounding tissues. Histopathologic examination is performed for definitive diagnosis in salivary gland cancers. The diagnosis is made by biopsy, that is, taking a sample from the tissue and examining it. After the diagnosis of salivary gland cancer, MRI is also useful for staging the cancer.
HOW IS SALIVARY GLAND CANCER TREATED?
The treatment plan is drawn according to the stage of the disease. In the staging of the disease, conditions such as the diameter of the tumor, whether it has spread to surrounding tissues, lymph node spread, histological type of the tumor are effective. A treatment plan is created with the staging determined as a result of these. Treatment options include surgery, radiotherapy and chemotherapy. In most patients, these treatment methods are applied together.
FREQUENTLY ASKED QUESTIONS ABOUT SALIVARY GLAND CANCER
Are salivary gland tumors dangerous?
Salivary gland tumors are usually benign. Parotid gland tumors are the most common tumors in the salivary glands. These tumors are benign. They do not progress aggressively and spread to another region is rare. In untreated cases of benign tumors, there is a very small possibility of malignancy, i.e. cancer. Therefore, it is important to evaluate the tumor formations in the salivary gland and start treatment with the appropriate treatment option. In malignant salivary gland cancers with a malignant course, the success of the treatment is greatly increased with early diagnosis and early initiation of treatment. For this reason, it is very important to apply to the hospital at the earliest period, especially in complaints such as swelling in the anterior region of the ear, under the jaw, difficulty swallowing, facial numbness, numbness.
Does salivary gland cancer kill?
Salivary gland tumors are usually benign. The survival rate of these tumors after treatment is 95 percent. In malignant salivary gland cancers with poor prognosis, late or untreated malignant salivary gland cancers, the success rate is around 50 percent.
Which salivary gland cancers are most common?
The most common benign tumor of the major and minor salivary glands is pleomorphic adenoma, which accounts for 50 percent of all salivary gland tumors and 65 percent of all parotid tumors. The most common malignant tumor of the major and minor salivary glands is mucoepidermoid carcinoma, which accounts for 10 percent of all salivary gland tumors and 35 percent of all malignant salivary gland tumors. This tumor most commonly occurs in the parotid gland.
Is every tumor in the salivary glands cancer?
Not every tumor in the salivary gland is cancerous. Not every swelling may be malignant. A considerable number of them, especially those in the salivary glands in front of the ear (parotid gland), are benign swellings. Therefore, the important issue is whether the swelling is benign or malignant.
What are the risk factors for salivary gland cancer?
Exposure to ionizing radiation is the most commonly blamed etiological factor in salivary gland cancers. The secondary risk is also increased in rubber industry workers, miners exposed to asbestos, plumbers and people working in timber.
What does benign salivary gland tumor mean?
Salivary gland tumors usually appear as slow-growing masses at the age of 50-70 years. In addition to examination and radiological examinations, fine needle biopsy plays an important role in the diagnosis. With the needle biopsy, the tumor is differentiated as benign or malignant and the treatment plan is shaped accordingly.
The majority of benign salivary gland tumors are mixed tumors or pleomorphic adenomas, which are more common in women between the ages of 30-60. In general, surgical treatment is performed for all benign tumors. During this surgery, the salivary gland where the tumor is located is removed as a whole. In benign parotid tumors, if the deep lobe is not involved by the tumor, only the superficial lobe is removed during surgery.
What does malignant salivary gland tumor mean?
Malignant tumors are grouped into low, intermediate and high grade according to the clinical behavior of the tumor, the rate of spread and the degree of structural change. High-grade tumors are more aggressive, tend to spread to surrounding tissues and neck lymph nodes, and have a high risk of distant metastasis. The first option in the treatment of malignant salivary gland tumors is surgery. During surgery, the tumor should be removed extensively, including normal tissue around the tumor that has not spread. Important nerves such as the facial nerve and the nerve that senses the tongue passing through the operation area should be preserved as long as there is no involvement by the tumor. In tumors with tumor spread detected in the neck lymph nodes and a high risk of metastasis to the neck lymph nodes even if there is no obvious involvement, the adjacent lymph nodes are also removed during surgery (neck dissection surgery). Radiotherapy is rarely the main treatment of choice for small tumors. For large tumors with a high risk of spreading, radiotherapy is given to the surgical site after surgery to prevent tumor recurrence in the same area.
Drug treatment (chemotherapy) may be preferred in patients who are not suitable for surgery due to other health problems and in patients with advanced regional spread and/or distant metastasis of the tumor.
What is the incidence of salivary gland cancer?
Malignant salivary gland tumors constitute 3-4 percent of malignant tumors in the head and neck region. Malignant salivary gland tumors are most frequently observed in the parotid gland in 75-80 percent, in the submandibular salivary gland in 20 percent and rarely in the sublingual or minor glands. The majority of patients with malignant salivary gland tumors are between the ages of 60-70. It is more common in men.
Does salivary gland cancer cause facial paralysis?
The facial nerve, the nerve that runs our facial muscles, runs in the parotid gland, our large salivary gland. If malignant tumors of the parotid gland spread to the cool lobe and involve the facial nerve, facial paralysis may occur.
Which doctor should be consulted in suspected salivary gland cancer?
The patient should consult an otorhinolaryngology specialist.
How is a biopsy performed in salivary gland cancer?
This can be done by open biopsy, fine needle aspiration biopsy (FNAB), core biopsy and frozen section biopsy. Today, FNAB is the most common biopsy method for masses in the parotid and submandibular glands. In minor salivary glands, open biopsy (incisional) with forceps is preferred.
Does fine needle aspiration biopsy in salivary gland cancer lead to tumor spread?
Needle biopsy is a diagnostic method that has been used in millions of patients all over the world for many years and is still used today. So far, there is no scientific evidence that it causes tumor spread. Therefore, it is safely practiced by physicians.
Can salivary gland cancer be prevented?
Unfortunately, the causes of salivary gland cancer are not yet known. Therefore, nothing can be said about how it can be prevented. While there is a cause and effect relationship between smoking and laryngeal cancer or lung cancer and therefore prevention is possible, there is no such relationship for salivary gland cancer. The only measure that can be taken for salivary gland cancers is to remove the tumor in the salivary gland from the body with a surgical procedure without delay.
Can salivary gland cancer be detected early?
The diagnostic process will begin when the patient who notices a swelling or mass in front of the ear, under the jaw or in the mouth and throat, applies to a physician after a while. If the physician suspects a salivary gland tumor on examination, he/she will usually resort to radiological imaging tools such as ultrasound, MRI (magnetic resonance imaging) or CT (computed tomography). This will be the second step after the examination in strengthening the tumor diagnosis. Then, sometimes a needle biopsy to take a sample of cells or tissue from the mass will be necessary to confirm the diagnosis and to make the most accurate pre-treatment plans.
Does salivary gland cancer metastasize?
Malignant tumors (malignant, malignant) grow faster and have the potential to metastasize (spread) to regional lymph nodes and distant organs (lung, liver, brain, bone, etc.). They invade surrounding tissues and develop by disrupting their function.
Will there be a scar on the face after salivary gland cancer surgery?
In parotid gland surgeries, an incision is made starting in front of the ear and extending from the back of the jaw to under the chin. At the end of the surgery, this incision is closed with subcutaneous sutures, which we call aesthetic sutures, and healing is observed with a minimal scar. By placing this incision behind the ear, the possibility of scarring can be greatly reduced. Similarly, in submandibular gland surgeries, an incision of approximately 3 cm is made under the chin and closed with subcutaneous sutures. The scar left after healing is negligible.
What are the consequences of removing the salivary glands after salivary gland surgery?
Unilateral removal of the parotid and submandibular glands does not cause problems such as salivation and dry mouth. The salivary glands and microscopic salivary glands on the other side of the face take over the function of the missing gland. In the late period of salivary gland surgery, functions such as nutrition and speech are not affected.
How long does salivary gland cancer surgery take?
When approaching salivary gland cancers and tumors, we first look at where the cancerous tissue is located. Secondly, it is tried to distinguish whether this tumor is benign or malignant. After these stages, the treatment options are discussed and the most appropriate treatment that will cause the least loss for the patient is found. This treatment should be a treatment that will cause the patient the least loss of organs, the least loss of labor and the least distress, in short, a treatment that will minimally affect the quality of life.
The next step is to determine how far the tumor has spread in the area where it is located and whether it has spread to the surrounding area, especially the neck lymph nodes, or to any other part of the body. Once this information is obtained, a treatment plan is drawn up taking into account the general condition of the patient.
How long is the hospitalization period for salivary gland cancer surgery?
Depending on the nature of the surgery, the average hospitalization period is usually 2-4 days.
What should be considered after the surgery?
After the operation, a tube called a drain is inserted to drain blood and fluid from the surgical site. The drain is usually removed after 24 to 48 hours. However, a bandaged dressing will remain for 3-4 days to prevent accumulation in the field. If there are stitches on the skin, they are removed on the 5th to 7th day, depending on the physician’s preference.
During this period, a total of 3 or 4 dressings are sufficient. If the skin incision is closed discreetly with special self-melting threads, the stitches will not need to be removed. The patient can take a bath most of the time during the week of the operation. It may be appropriate to give antibiotics for 3-4 days in case of infection.
After waking up from the surgery, the patient is not given any food or liquid by mouth for 3-4 hours until the anesthesia wears off. Later on the day of surgery, the patient is usually fed with soft, liquid foods, and most of the time, he/she can start eating normal foods from the next day onwards. However, especially after extensive surgeries for malignant tumors, it may take longer for the patient to recover and return to his/her old diet.
In general, in surgeries performed in the face and neck region, the planning of the incision and the postoperative suturing and closure are performed with special care, taking into account cosmetic concerns. However, patients are asked not to expose the incision site to the sun for up to one year to avoid scarring (scar tissue) that may occur in the late period. When they go out in the open air, they are advised to protect themselves with high protection factor creams or accessories such as scarves and scarves. It is also possible that some creams and gels can make the scar tissue less prominent.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Gastrointestinal Oncologic Surgery

- Esophageal diseases (esophageal cancer, reflux, hiatal hernia, achalasia, esophageal diverticulum diseases…)
- Gastric and duodenal diseases (gastric and duodenal cancer, morbid obesity, metabolic obesity surgery, tumors…), small and large intestine diseases (ulcerative colitis, Crohn’s disease, colon cancers…)
- Anus and anal canal diseases (anal fissure, anal fistula, hemorrhoids, anal polyps, anal incontinence, anal prolapse, anal abscess and anal cancers…)
- Liver diseases (cancer, giant hemangioma, hydatid cyst, metastases…)
- Pancreatic diseases (cancer, pancreatic pseudocysts and cysts),
- Gallbladder and biliary tract diseases (gallbladder and biliary tract stones, gallbladder cancers)
- Peritoneal cancer and metastases (peritoneal surgery)
Advanced Laparoscopic – Robotic applications
- Laparoscopic- Robotic obesity surgeries
Surgical operations for the rapid treatment of obesity include metabolic and diabetes surgeries such as sleeve gastrectomy, gastric bypass (mini gastric bypass and Roux n Y gastric bypass), transit bipartition, SADI-S, SAGI-S, duodenal switch, biliopancreatic diversion, ileal interposition, jejunoileal bypass. These surgical interventions are performed with laparoscopic and robotic methods, thus providing a comfortable operation process for both the surgeon and the patient. The patient can return to work and social life in a short time after these surgeries.
- Laparoscopic – Robotic gastroesophageal reflux, achalasia and hiatal hernia surgeries
Reflux, which develops when the structure between the esophagus and stomach in the digestive system is disrupted and stomach contents escape into the esophagus, achalasia, which causes food to get stuck in the esophagus, and hernias that can form in the diaphragm muscle (hiatal hernia) are treated with advanced laparoscopic-robotic applications of gastroenterology surgery.
- Laparoscopic- Robotic colectomy in large bowel cancers – TKME, anterior and low anterior in rectal cancers – Ta-TME – intersphincteric – Cecil surgeries – Natural surgical techniques such as NOSE
In inflammatory bowel diseases (Crohn’s disease or ulcerative colitis), surgical removal of the intestines may be necessary in cases where complications develop or no response to treatment is obtained. In these cases, laparoscopic-robotic small intestine-large intestine resection, total proctocolectomy and other surgeries provide a much faster recovery compared to open surgical procedures.
- Laparoscopic- Robotic splenectomy (spleen diseases surgery)
Removal of the spleen as a result of hematologic diseases or injuries is called splenectomy. In splenectomies performed with advanced laparoscopic-robotic applications, a much smaller incision is applied compared to open operations and the hospitalization period is shortened.
- Laparoscopic appendectomy
Appendicitis, a common and acute disease, requires urgent surgery. Appendectomy, which was previously performed as an open surgery, is now performed by laparoscopy and closed method, and patients can return to their daily life within 1-2 days.
- Laparoscopic-Robotic adrenalectomy (surgery for adrenal gland diseases)
Adrenal glands are glands located above the kidney. Benign and malignant tumors and hormone-secreting tumoral lesions in the adrenal glands can be removed by closed method with an operation called laparoscopic adrenalectomy.
- Laparoscopic – Robotic cholecystectomy (gallbladder disease surgery)
In cases such as sand and stones in the gallbladder and related inflammation, obstruction and jaundice, the only and definitive solution is a cholecystectomy operation. Cholecystectomy, in which the gallbladder is removed, can now be performed quickly by opening small incisions with the Laparoscopic-Robotic method.
Multidisciplinary applications
At our clinic, diagnosis and treatment of all digestive system organs diseases are carried out with multidisciplinary approaches.
GASTROINTESTINAL ONCOLOGIC SURGERY
- Gastroenterology surgery unit
- Gynecology -Oncologic Surgery department
- Radiology, Interventional radiology department
- Gastroenterology department and Advanced Gastroenterology interventions unit
- Pathology -Cytology center
- Medical oncology department
- Department of radiation oncology
- Nuclear medicine center
- Endocrinology department
- Department of Psychiatry
- Dietitian unit
- Psychology treatment unit
- Nutritional support unit
Services are provided in cooperation with specialists and teams. Our experienced and specialized academic staff performs open, laparoscopic and robotic surgeries in the fields of esophageal and gastric surgery, hepato-pancreato-biliary surgery, colon and rectal surgery, obesity and metabolic surgery. In addition, all types of cancer such as stomach, colon, rectum, pancreas, liver, esophagus, gallbladder, small intestine, peritoneal and intra-abdominal cancers are treated.
Diseases treated at the Gastrointestinal Oncological Surgery Center:
- Benign and malignant tumors of the esophagus
While tumors that form in the esophagus can be benign or malignant, in most cases they need to be removed by surgical operations due to the danger they pose. This procedure is performed by specialists in our Advanced Oncological Surgery Department.
- Benign and malignant tumors of the stomach
Tumors that form in the gastric mucosa can be benign or malignant. After investigating the type, size and whether there is a tendency to cancer, stomach tumors are removed by our team in the Advanced Oncological Surgery Department.
- Surgical procedures for diaphragmatic hernia and reflux disease
Diaphragmatic hernias and gastroesophageal reflux diseases, which can be observed in all age groups, can be completely eliminated or their effects can be minimized with the help of surgical operations.
- Surgical diseases of the small intestine
Surgical operations are used in the treatment of small intestinal obstruction, adhesions, ulcer formation, tumors, fistulas, diverticula and hernias. Surgery for these diseases is performed by doctors in the Department of Advanced Oncologic Surgery.
- Robotic – Laparoscopic and open surgeries for colon and rectal cancers
Benign tumors detected in the large intestine and rectum are usually surgically removed according to the physician’s recommendation, taking into account their size. Malignant tumors are removed with the help of surgical interventions regardless of their size. After the procedure, it is also examined whether it has spread to any other tissue and additional treatments are applied if necessary.
- Surgical procedures for inflammatory bowel diseases (Crohn’s disease and Ulcerative colitis)
In inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, the direction of treatment is determined by evaluating many factors such as the location of the disease, the patient’s symptoms and the patient’s age. In some cases, it may be necessary to remove part of the small intestine and the entire large intestine. Laparoscopic and robotic methods are used in surgical procedures for this purpose.
- Treatment of hemorrhoids, anal fissures, anal fistula and pilonidal sinus
Pilonidal sinus, also known as ingrown hair, anal fistula that develops between the last part of the large intestine and the skin, anal fissure, which is defined as a crack in the anus, and hemorrhoids, also known as hemorrhoids among the people, are diseases that fall within the field of the Advanced Oncological Surgery Department and can be treated with the help of surgical operations.
- Surgery of pancreatic cysts and tumors
A wide variety of cysts and tumors can occur in the pancreas. In some cases, these cysts can be kept under follow-up if they do not pose any danger to patients. However, the vast majority of these cysts and tumors are lesions that need to be surgically removed.
- Treatment of acute to chronic pancreatitis and its complications
In acute and chronic pancreatitis, surgical operations may be needed in addition to endoscopic methods in the treatment of the disease and its complications.
- Surgical treatment for all types of liver tumors
Liver tumors are common formations that in some cases do not cause any problems in the patient, but in some cases they can become cancerous and cause serious problems. These tumors are removed with the help of surgical operation when deemed necessary, taking into account their size and whether they are malignant or not.
- Surgical procedures for cystic diseases of the liver
Parasitic (infectious) cysts and non-parasitic (structural or cancer-related) cysts in the liver are removed surgically if they pose a danger or are deemed necessary by the physician.
- Surgical treatment of stones and tumors of the gallbladder and ducts
Stones in the gallbladder can cause inflammation in the gallbladder and bile ducts, blocking the bile ducts and causing infections. Tumors can also develop in the gallbladder and bile ducts. Surgical operations are performed by the specialists of the Advanced Oncological Surgery Department for tumors in the gallbladder or biliary tract and diseases caused by stones.
- Surgical treatment of hematologic, cystic and tumoral diseases of the spleen
Hematological diseases, cystic and tumoral problems are among the diseases that can be seen in the spleen. In these diseases, surgical procedures are performed in the Advanced Oncologic Surgery Department if deemed necessary. The most common of these procedures is splenectomy, the removal of the spleen.
- Robotic-Laparoscopic surgery for abdominal wall and surgical site hernias
Gastroenterology surgery applications are used in the treatment of adhesions and similar problems in the abdominal wall and surgical hernias. For these procedures, robotic surgery and laparoscopy techniques can be utilized if the patient’s health condition and disease allows.
ENDOSCOPY APPLICATIONS
- Diagnostic gastroscopy and colonoscopy
Gastroscopy and colonoscopy are needed in the diagnosis and treatment of certain diseases. Gastroscopy is preferred for examining stomach diseases and endoscopic applications called colonoscopy are preferred for examining colorectal diseases.
- Percutaneous endoscopic gastrostomy (PEG), jejunostomy (PEJ)
A percutaneous endoscopic gastrostomy (PEG) or percutaneous endoscopic jejunostomy (PEJ) is performed in the Gastroenterology Surgery Department to ensure healthy and adequate nutrition for patients who cannot eat and should not be fed by mouth, and a feeding tube that reaches directly into the stomach is placed.
- Endoscopic stent placement
In diseases involving stenosis of the gastrointestinal tract, a stent can be placed in the affected area using endoscopic methods to eliminate the stenosis. This procedure can be performed in the Advanced Oncologic Surgery Department under appropriate conditions.
HYPEC (HOT CHEMOTHERAPY) AND PIPAC (AEROSOL PRESSURE CHEMOTHERAPY)
HIPEC (Hyperthermic Intraperitoneal Chemotherapy) is a form of treatment called “Hyperthermic Intraperitoneal Chemotherapy”, which has been frequently mentioned in cancer treatment in recent years.
Today, many different methods are used in cancer treatment and significant successes are achieved. The intra-abdominal hot chemotherapy application called HIPEC is one of the most important steps taken in this field in terms of both prolonging the patient’s life expectancy and improving the quality of life.
In some cancers originating from intra-abdominal organs, systemic chemotherapy given intravenously before (neoadjuvant treatment) or after (adjuvant treatment) or both before and after surgical treatment may not give the expected response. In this case, when the desired response to the treatments is not achieved, the disease progresses gradually and eventually the patient’s life may be endangered.
Treatment option for advanced intra-abdominal cancers: HIPEC
At the point where the desired response cannot be obtained from cancer treatment, the “intra-abdominal hot chemotherapy – HIPEC” treatment option comes to the agenda, which is a method that will both prolong the patient’s life expectancy and improve their comfort. Intra-abdominal chemotherapy aims to The intra-abdominal organs and abdomen are covered by a layer called “peritoneum”. This structure covers both the surface of the intra-abdominal organs and the inner surface of the abdominal wall. This thin layer lining the abdomen provides lubrication for the organs with the small amount of fluid it secretes. While cancer continues to develop in the organ where it originated, it can spread to other organs and areas as the disease progresses.
How is HIPEC treatment applied?
Cancer can spread through blood, lymph nodes and spillage into the abdominal cavity. Therefore, in advanced stages of intra-abdominal cancers, the tumor can also spread to the peritoneum. In this situation, which occurs in the last stage of the cancer, the drugs administered intravenously to the patient may not reach the peritoneum at the desired level and the treatment will be inadequate. However, the peritoneum, which is densely covered with tumor, should philosophically be considered as an organ, and the intra-abdominal cavity should be made as tumor-free as possible microscopically by washing the peritoneum and the involved organ or organs. This procedure is called “SRC (cytoreductive surgery+peritonectomy)”. Following these procedures, tumor destroying drugs with a temperature of 42-43 degrees are administered into the abdomen with a special apparatus. The intra-abdominal washing process is completed between 60 and 90 minutes. During this time, it is aimed to destroy tumor cells at microscopic level.
Why are chemotherapy drugs given by heating?
Anticancer drugs are given into the abdomen by heating;
- Heat facilitates the penetration of the drug into the tissue and enhances the cancer cell killing effect of the selected chemotherapeutic agent.
- The heat itself has an anti-tumor effect and the heat contributes to the even distribution of the drug to all surfaces in the abdomen.
- During HIPEC, tumor cells are mechanically removed from the surface of the small intestine and from the clot-fibrin layers.
In which diseases is HIPEC applied?
In patients with peritoneal involvement in advanced stages of cancer, fluid (ascites) begins to collect in the abdomen. This fluid may cause the patient’s abdomen to swell gradually, and the respiration and circulation may become problematic with the pressure and tension it creates. Sometimes it becomes so widespread that it even prevents the patient from lying down. It can also cause cancer cells to spread to other areas of the abdomen. Although it is possible to drain the fluid through the cannula for the patient’s relief, there will be fluid collection again as the pathology continues. Patients with advanced cancer are those who have left all treatment options behind, and in such cases, HIPEC treatment comes to the fore, which will prolong the patient’s life and provide comfort of life. With this procedure, successful results are obtained in cancers of the peritoneum itself, appendix cancer and ovarian cancer in women. In addition to these, it has also started to be applied in colon, stomach and recently pancreatic cancers.
Some components should not be ignored while performing such treatments. It makes sense when all stages of treatment are carried out together.
In which cases is HIPEC treatment not applicable?
HIPEC is not performed in cases where there is involvement outside the abdomen. Brain, bones, lung metastases…). If there are three or fewer metastatic foci in the liver, HIPEC can be applied by removing them. However, HIPEC is also not indicated in cases of extensive liver metastases. Another important organ is the small intestine. Since the small intestines are the organs of nutrient absorption in the digestive system, extensive small bowel resections are not compatible with life. Therefore, it does not make much sense to perform HIPEC in patients with extensive small bowel involvement. The majority of these patients are patients with advanced cancer and their life expectancy is limited to months. This important detail should not be ignored and it should be taken into consideration that the disease cannot be completely cured and eliminated, but life comfort and life expectancy can be prolonged.
PIPAC – PRESSURIZED AEROSOL CHEMOTHERAPY
PIPAC era in the treatment of abdominal cancers
The PIPAC method is a “pressurized aerosol chemotherapy” application used in peritoneal cancers that eliminates the problem of intravenous chemotherapy drugs not reaching the natural folds of the body. With this method, the tumor can be controlled in the ideal patient group and the patient’s life expectancy and quality of life can be increased.
What is the definition of intra-abdominal cancer?
The “peritoneal layer”, which completely surrounds the abdominal wall and covers the intra-abdominal organs, is considered an organ in itself. Cancers in this region are tumors originating from the peritoneum itself, as well as metastases of cancers of the colon and rectum, ovary, uterus and stomach. As a result of the progression of these existing cancers, cancerous cells can metastasize through the blood or lymph in the environment where they are located, and a disease that extensively involves the intra-abdominal organs can occur. After intra-abdominal metastasis, there is fluid collection in this area, which is defined as ascites. A picture that shows that the patient cannot benefit from any treatment constitutes the group of advanced cancer cases. In such cases, the patient is given intravenous chemotherapy, defined as systemic chemotherapy. Radiotherapy may also be used, but sometimes chemotherapy does not go beyond a certain point. The drug reaches the peritoneum, but cannot penetrate it. Because this membrane, which has no vessels of its own, is fed by diffusion. Therefore, the scattering in the peritoneum cannot be eliminated with treatment. The tumor spreads like a handful of bulgur.
How is the PIPAC method applied in intra-abdominal cancers?
SRC (peritonectomy and cytoreductive surgery) performed in patients whose tumor has metastasized means reducing the reduction. Certain criteria are taken into consideration when selecting the patient group to receive this treatment. In a patient with colon cancer, the peritoneal membrane is completely peeled away when the tumor spread does not reach the liver but is widely distributed in the peritoneum. The surgeon destroys all accessible tumors surgically or by cauterization. After the cleaning, the drug is administered into the abdomen at a dose level of 1/10 with a pressurized hot chemotherapy method called PIPAC. In other words, if the patient is given 10 grams of drug intravenously in systemic chemotherapy, the same success can be achieved with 1 gram of drug in PIPAC. In this way, the cytotoxic effect of cancer-killing drugs on the patient’s healthy cells is reduced and a high level of effectiveness is achieved.
Which patient group is the procedure suitable for?
Patients can be discharged within one day after the PIPAC procedure. If the patient’s treatment yields positive results, the procedure can be repeated four weeks later. This procedure provides an important advantage and gives hope to patients who are told that “nothing can be done”.
What is the contribution of the PIPAC procedure to the patient’s life expectancy and quality?
With the laparoscopic PIPAC treatment, the abdomen is entered through two incisions, one 1 cm and the other 0.5 cm. The drug to be administered is selected according to the type of organ from which the tumor originates. The high-pressure heated chemotherapeutic drug, which is administered through a pen-like apparatus through the trocars entering the abdomen, is spread all over. With this method, the drug can reach all areas. During the procedure, triangulation marks are placed in certain places so that the treatment can be repeated after four weeks if necessary. This treatment, which can be repeated after four weeks if necessary, can be done seven to eight or even up to 10 times. By the third or fourth treatment, almost complete disappearance of the tumor can be seen in the marked spots. The life expectancy of one to two months can sometimes be increased up to 10 times. However, the patient’s general health condition, cell structure, tumor type and genetic structure are of great importance for this.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Interventional Neuroradiology

What are the areas where Interventional Neuroradiology is used?
Brain and spinal angiography;
Angiography of the vessels of the brain and neck is the gold standard procedure. It is performed by injecting a radiopaque contrast agent into the blood vessel. A fluoroscopy (angiography) device is used to view and record the image during contrast injection. The procedure begins with local anesthesia at the entry site of the appropriate vessel. A sheath is inserted into the vein. A catheter is inserted into the vessels to be entered and the anatomy and pathologies of that vessel are visualized. Especially vascular bubbles and tangles are visualized and treatment planning is made.
Aneurysm (Bubble) Embolization;
An aneurysm is an abnormal focal enlargement of an artery caused by weakening of the inner muscle layer (intima) of a blood vessel wall. It is most common between the ages of 35-45. This enlargement can thin and rupture without warning. In case of rupture, there is a risk of stroke because blood flow is reduced or completely blocked. The ruptured bubble can also cause bleeding between the membranes around the brain (subarachnoid). The majority of aneurysms are under 2.5 cm in size, above this they are called giant. Giant aneurysms are more likely to rupture and are more difficult to treat.
Risk factors: Hypertension, smoking, genetic defects (Ehler-danlos, tuberous sclerosis, FMD, Kleinfelter’s disease, alpha 1 antitirpsin deficiency), alcohol consumption, drug use, trauma and infections can cause brain aneurysms. It is more common in the presence of family history, female gender and older age.
Types: Saccular (bubble) type are dome-shaped protrusions that occur in the branching areas of the vessel. They may have a narrow or wide neck. Fusiform aneurysms are enlargement of a short segment of the vessel. Blister type are rose thorn-shaped aneurysms.
A brain aneurysm is rarely symptomatic unless it ruptures. Very large ones can cause compression symptoms. Loss of vision, double vision, pain above the eye, numbness on one side of the face may develop due to compression. When an aneurysm ruptures, severe headache (a headache described as never experienced before), nausea, vomiting, inability to look at light, loss of consciousness, seizures, and unilateral weakness, which is a sign of stroke, may develop. The most important feature of these symptoms is their sudden onset.
Diagnosis: Brain aneurysms are usually detected on CT or MRI scans taken after rupture. Angiography, which is the gold standard in diagnosis, is performed in patients with suspected aneurysm. Here, the structure of the aneurysm is evaluated and a treatment plan is made. With new developments in tomography, images close to angiography can be obtained. In addition, problems that may develop in angiography are not seen. MRI also helps to locate and diagnose an aneurysm.
Treatment Endovascular aneurysm treatment is a viable option for cerebral aneurysms. Endovascular treatment is now considered the first line of treatment for aneurysms. Treatments vary for bleeding or non-bleeding aneurysms. With the treatment process, filling the inside of the bubble with coils, stents are used on the web.
AVM Embolization
They are abnormal tangles of blood vessels in the brain or spinal cord. The cause of AVMs is not clear. Most people are born with them, but they can also form later in life. AVMs occur in some people with hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome. HHT affects the way blood vessels form in various parts of the body, including the brain.
What happens in the presence of AVM?
The heart sends oxygen-rich blood to the brain and spinal cord through arteries. The arteries become thinner down to the smallest blood vessels (capillaries) and their flow rate slows down. They release oxygenated blood to the brain cells. In an AVM, on the other hand, the AVM is devoid of capillaries and the incoming blood quickly returns to the heart, which disrupts the brain’s nutrition there.
People with brain AVM may experience headaches or seizures. In some people, it is detected in brain scans for other reasons or in brain imaging after bleeding. Once a brain AVM is diagnosed, it must be treated to prevent complications such as brain damage or stroke. The risk of brain AVM bleeding ranges from about 2% to 3% each year. The risk of bleeding may be higher for some types of AVM or in people with a previous AVM rupture. Brain hemorrhage is caused by the thinning of the walls of the affected arteries and thin veins due to excessive pressure, causing them to rupture. These hemorrhages sometimes go undetected because they do not cause brain damage and signs or symptoms. In these patients, potentially life-threatening bleeding episodes occur.
Treatment is planned depending on whether the AVM is bleeding or not, its high risk of bleeding, its proximity to important structures and its size. During the procedure, these vascular tangles are entered and occlusive drugs are administered.
AVF Embolization
An arteriovenous fistula (AVF) is an abnormal connection between an artery (artery) and a vein (vein). The connection between a high-pressure artery and a low-pressure vein can increase blood flow in the area, often widening both the artery and the vein. AVFs are sometimes present at birth (congenital) or develop after birth and are sometimes the result of an injury (acquired).
Arteriovenous fistulas in the face or neck cause swelling and an abnormal pulse or murmur. In extreme cases among infants, it can overload the heart. They rarely cause serious problems with brain development. Sometimes we see symptoms at birth, sometimes the condition does not become apparent until late childhood. Large fistulas can cause heart failure at birth. Smaller ones can cause increased pressure in the vessels inside the head, leading to hydrocephalus or enlargement of the cerebral ventricles (the spaces in the brain that hold fluid). Fistulas in the spinal cord can compress the spinal cord, causing numbness and/or weakness.
Diagnosis: The first step for fistula diagnosis is MRI and MRA. In case of doubt, CTA or classical angiography procedures are performed.
Treatment: Endovascular embolization is the most common form of treatment for an AVF. This is usually performed by inserting a catheter into the feeding artery or fistulized vein. Various types of vascular plugs such as coils, detachable balloons, embolization glue, embolization particles, embolization material (called Onyx), and various types of devices are used to stop the blood flow. After closing the connection between the artery and vein, the AVF heals and usually does not recur. Another treatment option is to close the fistula surgically.
Carotid artery stenting: Carotid artery stenosis is a serious condition that causes stroke. Stenoses over 70% without complaints and stenoses over 50% with recurrent stroke require treatment. Stent procedures are applied especially in cases with high risks of surgical jugular vein treatment and in cases where stenosis persists after surgery. The procedures are usually performed awake and using mild sedatives. After local anesthesia in the groin, the artery is punctured with a needle and the carotid (jugular) artery is accessed with thin tubes (catheter) inserted through it. Fluoroscopy (angiography) is used to guide the procedure and contrast material is injected into the vein to take images. The stenosis in the carotid artery is crossed with thin wires, and a filter is placed beyond the stenosis to prevent clots during the procedure. The stenosis is widened with a balloon over the filter wire. A stent is placed in the stenosis and the balloon and stent are adhered to the wall. The procedure is finalized after controls are taken. Risks of the procedure include bleeding in the groin, false aneurysm or clot in the brain vessel. These occur in less than 5% of cases.
Stroke treatment : Stroke is one of the most common causes of death and disability in the world. It is a sudden interruption of blood flow to any part of the brain. Endovascular treatment of stroke is the removal of the clot that develops in the vessel within the first 6 hours after the stroke (thrombectomy). If the blood clot cannot be removed, dissolving drugs are given (thrombolysis). If there is stenosis in the vessels, a stent may also be placed.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
Medical Oncology

CEMOTHERAPY
What is chemotherapy?
Chemotherapy is the treatment of a tumor with medication. It is a very important part of tumor treatment along with surgery and radiotherapy. Chemotherapy is used to kill tumor cells or stop the tumor from growing. Sometimes a single drug, sometimes several drugs are administered in various ways.
Who Administers Chemotherapy?
The branch of science that deals with chemotherapy is called “Medical Oncology” or “Medical Oncology” and the doctor working in this field is called “Medical Oncologist”. Medical oncology is a separate specialty; a medical oncologist is an internal medicine specialist who specializes in tumor treatment. Tumor treatment is a team work and must be performed in centers where all members of this team are present. This team should include a surgeon specialized in tumor surgery, a radiation oncologist for radiotherapy, and a medical oncologist for chemotherapy and patient care (supportive care).
What is the purpose of chemotherapy?
Chemotherapy may be administered for different reasons, depending on the type of tumor and the characteristics of the patient.
- To completely destroy the tumor and cure the patient,
- To prevent the tumor from spreading,
- To stop or slow the growth of the tumor,
- Chemotherapy is used to relieve the symptoms caused by the tumor.
Although it is an effective treatment method, in some cases it cannot completely destroy the tumor, it can only improve the symptoms and provide a comfortable life. For some tumors, chemotherapy is the only treatment. In others, chemotherapy is administered in tandem or simultaneously with other treatments (surgery and radiotherapy). For example, chemotherapy may be given before surgery to shrink the tumor and after surgery to prevent its spread. The same applications can be performed before and after radiotherapy, or chemotherapy can be administered simultaneously with radiotherapy using various methods.
What is the frequency and duration of chemotherapy?
The duration and frequency of treatment depends on the chemotherapy scheme that is specifically selected according to the disease and the patient’s condition. The duration and frequency can be changed by the doctor according to the response obtained with the treatment and the side effects that occur. Generally, the most common intervals are 3 or 4 weeks, but some treatment schemes also include weekly or biweekly treatments. The most important, even vital, point about the timing of chemotherapy is that the treatment should be as regular as possible and as timely as side effects allow. If treatment intervals are unnecessarily prolonged, the tumor is at risk of recovering and becoming resistant to the drugs, thus becoming stronger. In this way, the tumor continues to grow and spread, and the chance of treatment success decreases. Patients should never go beyond the recommendations of their doctor regarding chemotherapy appointments.
Before discontinuing treatment for any reason, talk to your doctor, explain your problems and ask for help.
Make sure to follow the treatment schedule. Never change your treatment day on your own initiative on the grounds that you are not feeling well.
Make sure you take the medicines you have to use at home.
Otherwise, you may face treatment failures due to incomplete treatment.
Where is chemotherapy administered?
Chemotherapy must be administered in centers where people trained in this field work. It should never be administered in a hospital or at home by a healthcare professional who has no experience in chemotherapy without the knowledge and permission of the doctor.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS LEUKEMIA (BLOOD CANCER)? WHAT IS LEUKEMIA?
Leukemia, known as one of the types of blood cancer in the community, is when one of the blood-producing stem cells, which originates from the bone marrow, pauses at a stage of its development due to a combination of various factors and begins to proliferate uncontrollably. Leukemia (blood cancer), also known as leukemia, first invades the bone marrow and then all organs. Blood cancer, which affects the bone marrow and lymphatic system, the body’s blood production system, is one of the malignant cancers that show a progressive course if left untreated. If leukemia is caused by an uncontrolled increase in mature white blood cells, it has a chronic and slow course. Those that develop due to the uncontrolled increase in immature white blood cells are defined as acute, i.e. with a rapid course. Blood cancers with a rapid course often show a sudden onset and give clinical signs and symptoms especially within 1-2 months. Therefore, the diagnosis should be made in a short time and treatment should be started as soon as possible.
Although the exact cause of leukemia is unknown, it is known that exposure to radiation, chemicals such as benzene and pesticides increases the risk of leukemia. Leukemia, one of the most common blood cancers, can be successfully treated with targeted smart drugs as well as patient-specific stem cell transplantation options.
WHAT ARE THE TYPES OF LEUKEMIA (BLOOD CANCER)?
Leukemia is classified into two groups: acute (sudden onset, rapidly progressing) and chronic (slow progression, chronic). Acute leukemia is divided into acute lymphoblastic leukemia (ALL) and acute myeloblastic leukemia (AML). Chronic leukemias are further subdivided into Chronic Lymphocytic Leukemia (CLL) and Chronic Myeloid Leukemia (CML).
Among the types of leukemia, acute leukemia is a highly aggressive and rapidly progressing type of disease. If acute leukemia is not diagnosed and treated in time, it can cause the patient to die within days or weeks. Chronic leukemia, on the other hand, can remain silent for a long time in a very slow course and may progress over years.
WHAT IS ACUTE LEUKEMIA?
The incidence rate of acute leukemia among blood cancers is 15-20%. Acute leukemia is the most common type of cancer in children and progresses very rapidly. Acute leukemia can be seen at any age and the incidence rate increases with advancing age. Acute leukemia, which manifests itself in a very short time with its symptoms and signs, occurs when stem cells in the bone marrow, which are responsible for the production of blood cells, become cancerous and multiply uncontrollably and rapidly. In acute leukemia, cancer cells spread very rapidly first to the bone marrow and then to the whole body. Since white blood cells called leukocytes cannot be made in patients with acute leukemia, severe infections can often occur. Since platelet cells, which are responsible for blood clotting, cannot be produced, skin bleeding, bleeding from the gastrointestinal tract or serious bleeding in vital organs may occur. Anemia, the most prominent symptom of acute leukemia, is one of the easiest symptoms for patients to recognize. It can also appear as a disorder in any organ as it spreads to other organs in the body.
Acute leukemia is divided into two main groups: acute myeloblastic leukemia (AML) and acute lymphoblastic leukemia (ALL), which have many subtypes. Early diagnosis, typing and rapid treatment of these tumor types, each of which progresses very rapidly, is very important. When symptoms appear, diagnosis should be made by specialist doctors in specialized oncology centers and appropriate treatment should be planned.
WHAT IS CHRONIC LEUKEMIA?
Chronic leukemia is a type of leukemia that progresses more slowly than acute leukemia. However, chronic leukemia gives better results. There are two main subgroups of chronic leukemia, chronic lymphocytic leukemia (CLL) and chronic myelocytic leukemia (CML), which occur when mature cells do not fulfill the tasks they should perform and proliferate abnormally.
WHAT IS LYMPHOCYTIC LEUKEMIA (CLL)?
Lymphocytic leukemia (CLL) occurs when leukemic cells, which resemble mature normal lymphocytes and protect the body against infections, but cannot perform their functions, multiply in the bone marrow. CLL cells settle in the bone marrow, lymph nodes and blood, resulting in swollen lymph nodes and enlarged spleen. Mostly seen in the 60-70 age group, CLL accounts for 30% of all leukemias. Since the disease progresses very slowly, patients can live for a long time without being diagnosed. After diagnosis, some patients do not need treatment unless CLL causes problems. CLL is diagnosed by detecting a genetic change specific to the disease with special methods. In the past, this disease was very difficult to treat with chemotherapy and bone marrow transplantation, but today it can be treated very simply.
WHAT CAUSES LEUKEMIA (BLOOD CANCER)?
Although the exact cause of leukemia is unknown, scientists believe that viral, genetic, environmental or immunological factors play a role. Some of these are as follows;
- Exposure to high levels of radiation
- Exposure to industrial chemicals such as benzene and formaldehyde
- Some of the chemotherapy drugs
- Some genetic diseases (Down syndrome etc.)
- Viruses
However, these risk factors explain only a small proportion of leukemia. In the majority of patients who get leukemia, no risk factor has been shown.
Other causes of leukemia;
- Long hours of use of technological devices such as tablets and cell phones by children
- Air pollution
- Additives in foodstuffs
- Chemical substances
- Rotten foods
WHAT ARE THE SYMPTOMS OF LEUKEMIA (BLOOD CANCER)?
The symptoms of leukemia vary depending on the type. Symptoms of blood cancer may have common features with some findings observed in other blood cancers. Due to anemia;
- Pallor
- Fatigue
- Get tired quickly,
- Symptoms such as shortness of breath during exertion are observed.
Symptoms of leukemia (blood cancer) include unexpected bleeding under the gums, nose, gums and skin, bruising and pinhead-sized red rashes that do not fade with pressure as a result of infections caused by a weakened immune system. These are the symptoms of acute leukemia;
- Pallor, weakness,
- Loss of appetite, weight loss,
- Night sweats
- Frequent recurrent fever and infections that cannot be controlled with appropriate treatment,
- Bone pain
- Bleeding under the skin (red rashes as small as a pinhead, bruising that occurs easily)
- Nosebleeds and bleeding gums, swollen neck and axillary lymph nodes, swollen abdomen, swollen gums.
Symptoms of blood cancer can be similar to those of many other diseases. Leukemia, which can spread to all organs of the body, can have similar symptoms with rheumatic diseases, infectious diseases, hemorrhagic diseases, lymphoma, myeloma and other blood cancers.
WHAT ARE THE SYMPTOMS OF LEUKEMIA IN CHILDREN?
When all childhood cancers are considered, leukemia accounts for approximately 30 percent. Childhood cancers and leukemia are frequently seen between the ages of 2-5 years or 5-10 years. Although leukemia in children has very comprehensive clinical findings, some symptoms should be suspected. We can list them as follows;
- Rapid weight loss
- Loss of appetite
- Discoloration of color
- Bruises or unexpected glands on the body persist for a long time or gradually increase in size
- Abdominal swelling
- Joint pain
- Persistent fever that persists for a long time and lasts more than 5 days
Newborn babies can maintain the immune system they receive from their mother for 6-8 months. After that, it builds its own immune system until the age of 2. Until this period, they can have 5 infections per year. It should not be forgotten that viral infections can trigger leukemia cancers.
One of the causes of leukemia in children is vitamin D deficiency. There are many studies showing that rickets at an early age and the resulting vitamin D deficiency are effective on cancer. For this reason, it is very important that children see the sun in appropriate weather conditions and at the hours recommended by experts. The importance of genetic factors in leukemia should not be ignored.
HOW IS LEUKEMIA (BLOOD CANCER) DIAGNOSED? WHAT ARE THE DIAGNOSTIC METHODS?
Early diagnosis is very important in leukemia. Leukemia, which affects the reproduction and function of blood cells, matures the cells in the bone marrow and transforms them into erythrocytes, leukocytes or platelets. In leukemia, leukemic cells (blasts) multiply uncontrollably and suppress the growth of normal blood cells. Blood and bone marrow tissue samples are taken and examined for diagnosis in line with serious complaints such as infection and bleeding caused by the inability to produce blood. A simple blood count and microscopic examination of the cells in the blood are usually sufficient for diagnosis. However, the definitive diagnosis is made by bone marrow biopsy.
Approximately 95% of leukemias are acute leukemias. Acute leukemias are 85% acute lymphoblastic and 15% myeloblastic leukemia. Among these, acute lymphoblastic leukemias respond more favorably to treatment. Since the life expectancy is longer in children, early diagnosis and treatment is of great importance as the success rates are higher compared to adult cancers.
In order to diagnose leukemia (blood cancer), the patient’s history should be listened to. In addition to the examination, advanced diagnostic methods and examinations should be performed.
Examination
The person with suspected leukemia (blood cancer) should first have a good physical examination (lymph nodes should be evaluated for swelling, liver, spleen size).
Appropriate blood tests:
Blood count and necessary biochemical tests
Bone marrow biopsy:
Bone marrow from the hip bone should be examined. Bone marrow biopsy and pathologic examination of bone marrow fluid spread on glass.
Genetic examinations:
Genetic analysis of leukemia cells from bone marrow or blood samples
HOW IS ACUTE LEUKEMIA DIAGNOSED?
Diagnosing acute leukemia is not very difficult. Acute leukemia can be diagnosed with a simple complete blood count. In a complete blood count, leukemia can be easily diagnosed by detecting a decrease in the number of normal blood cells and an increase in the number of cancer cells called “blasts”. A biopsy of the bone marrow can also show that the bone marrow has been invaded by cancer cells. The difficult part of leukemia diagnosis is to determine the type of cancer. The “immune phenotypic” method, various cytogenetic and molecular tests can distinguish between different types of acute leukemia.
Determining the subtype of leukemia is very important as it is directly related to the treatment process. Because there are different treatment methods for all subtypes of leukemia. If the patient is diagnosed with acute leukemia, risk factors are identified. When acute leukemia is diagnosed in adults, it is known that more than 70-80% of patients fall into the high risk group. This means that even if leukemia is controlled, it can recur in a very short time.
HOW IS LEUKEMIA (BLOOD CANCER) TREATED?
Leukemia treatment involves many disciplines. It is treated by adult and pediatric hematology specialists in fully equipped hospitals. The oncology center where leukemia is treated should have a well-trained team of nurses to administer chemotherapy, a well-equipped blood bank with 24-hour service, an infectious diseases specialist, a radiation oncologist to provide radiation therapy when necessary, and sophisticated laboratory infrastructure.
Leukemia is a treatable disease and the success rate of treatment is increasing day by day with many new methods discovered in recent years. The discovery of new chemotherapeutic agents, the introduction of targeted molecular drugs and biological drug therapies into daily use, the development of advanced radiotherapy devices, and advances in bone marrow transplantation have led to great strides in prolonging the life expectancy of patients and fully treating the disease.
The first treatment method that comes to mind for leukemia is chemotherapy. The type, dose and route of administration of chemotherapy drugs may vary depending on the type of leukemia. In addition to chemotherapy, which lasts about 24 months, bone transplantation is another method that comes to mind in the treatment of some types of leukemia. The success rates achieved in the treatment of leukemia in our country are at world standards with both chemotherapy and bone marrow transplantation.
Chronic myeloid leukemia has been largely curable since 2000. Since the disease is well recognized, drugs that disrupt the mechanism are used. This treatment, called targeted therapy, prevents myeloid-derived cells, which constantly proliferate in the bone marrow, from maturing or maturing and entering the blood. In patients who cannot be controlled with drugs, the most effective treatment method is “allogeneic stem cell transplantation”. Stem cell transplantation is performed with the help of stem cells taken from tissue-matched siblings, close relatives or non-relative volunteer donors. For chronic lymphocytic leukemia (CLL), a type of leukemia with a slow course, only supportive treatments are given in the early stages. In advanced stages or in high-risk patients, drugs or targeted antibodies (immunotherapy) can be applied. Although chronic lymphocytic leukemia is a disease of advanced age, it can also occur before the age of 50. In these high-risk patients, allogeneic stem cell transplantation is one of the treatment options.
THINGS YOU SHOULD KNOW ABOUT LEUKEMIA
- Leukemia is more common in men than in women.
- It is especially more common in the white race than in the black and yellow races.
- The frequency of leukemia diagnoses in adults is more than 10 times higher than in children, and the risk increases with age.
- Leukemia in childhood is more common under the age of 4.
- Genetic predisposition is important in some leukemias.
- It is known that acute forms of leukemia are more common in genetic diseases such as Down syndrome.
- Exposure to radiation and chemicals such as benzene may also be implicated in CML formation.
- Chemotherapy treatment for another cancer, smoking and the presence of certain blood diseases are also among the causes of leukemia.
- In the US, 1 person develops blood cancer every 4 minutes.
- In 2016, 60,000 new patients were diagnosed with leukemia in the US alone.
- Acute leukemia is the most common type of cancer in childhood with a rate of 35%.
- The probability of a man or woman being diagnosed with leukemia in their lifetime is estimated at 1.5%.
- Today, the survival rate of patients diagnosed with leukemia longer than 10 years has increased 4 times compared to the 70s.
- Between 2006 and 2012, the 5-year survival rate of leukemia patients was 60%.
- Eight out of 10 children diagnosed with leukemia are completely cured.
WHAT IS ACUTE LYMPHOBLASTIC LEUKEMIA?
Acute lymphoblastic leukemia (ALL) is a type of cancer that affects the blood and bone marrow. It progresses quickly and aggressively and requires urgent treatment. ALL is characterized by an overproduction of immature white blood cells called lymphoblasts or leukemic blasts. The bone marrow produces stem cells that have the ability to develop into three important types of blood cells: red blood cells, white blood cells and platelets. The bone marrow does not usually release stem cells into the blood until they become fully developed blood cells. But in acute lymphoblastic leukemia, large numbers of white blood cells are released before they are ready. These are known as blast cells. As the number of blast cells increases, the number of red blood cells and platelets decreases. Because the bone marrow cannot produce enough red blood cells, normal white blood cells and platelets, people with ALL become more susceptible to anemia, recurrent infections and easy bruising and bleeding. The blast cells can then be shed from the bone marrow into the bloodstream and accumulate in various organs, including the lymph nodes (glands), spleen, liver and central nervous system (brain and spinal cord).
ALL can occur at any age, but is more common in young children (0-14 years), who account for about 60 percent of all cases. ALL is the most common type of childhood leukemia and the most common childhood cancer. Boys are affected slightly more often than girls. With treatment, most children with ALL are cured these days, while cure rates in adults are more variable.
FREQUENTLY ASKED QUESTIONS ABOUT LEUKEMIA (BLOOD CANCER)
How is stem cell transplantation performed in leukemia?
In the treatment of leukemia, stem cell transplantation is preferred if the risk of recurrence of the disease is high in those whose disease is under control in the early period with drug therapy. Stem cell transplantation is performed with stem cells taken from the patient himself/herself (autologous) or from tissue-matched siblings, other close relatives or non-related volunteer donors (allogeneic). For stem cell transplantation, stem cells are collected from the hip bone by anesthetizing the donor or from the vein with special devices after using drugs that stimulate stem cells. Before stem cell transplantation, the patient receives high doses of medication and/or radiotherapy. The aim of this stage is to destroy cancer cells that may remain in the patient’s body and to drain the cells in the patient’s bone marrow. The transplant is then performed. “Autologous transplantation” can be performed in patients who cannot find a suitable stem cell donor, but the most effective treatment is allogeneic stem cell transplantation. Patients may need to be followed up for many years after transplantation to avoid serious problems.
Recently, stem cell transplantation from partially compatible (50-80% compatible) relatives, called “haploidentical”, can also be performed in patients who cannot find a suitable stem cell donor and have a high risk of recurrence. Haploidentical transplantation can provide disease control and survival for more than one year in approximately half of the patients, depending on the risk of the disease. However, when the immune systems of patients in this group are suppressed as a result of tissue incompatibility, they should be closely monitored in fully equipped and experienced centers.
Who should receive stem cell transplantation?
Some points should be considered when performing stem cell transplantation. Criteria such as the patient’s age, whether the patient has additional health problems, and whether the patient is in the medium or high-risk group are taken into consideration. Some patients respond to treatment later or their disease recurs more quickly. In such patients, the risk of disease recurrence can be determined by the presence of certain gene changes. As a result of the examination of gene changes, allogeneic transplantation should be performed in patients who are in the high-risk group (if they are young and do not have additional diseases). In patients with a low risk of recurrence; stem cell transplantation is not recommended in the first stage due to the high number of side effects and sometimes life-threatening side effects. However, if the disease recurs, stem cell transplantation is performed. In blood cancers that do not respond to initial treatment, allogeneic transplantation can be applied as a treatment option.
How is acute leukemia treated?
The first step in the treatment of acute blood cancers is chemical therapy treatment. The treatment is applied in two or three stages depending on the type of the disease. At the beginning of the treatment, the aim is to reduce the number of cancer cells, increase the number of normal cells and eliminate the symptoms of the disease. This is the most important stage. Even if this phase is successfully completed, cancer cells may start to multiply again in a large proportion of patients and the disease may recur. After control is achieved, so-called reinforcement treatments are applied to prevent the disease from recurring. Reinforcement treatment is again done with chemotherapeutic drugs or stem cell transplantation. In addition, in the treatment of patients with acute lymphoblastic leukemia (ALL), there is a maintenance treatment period that can last 2-3 years to prevent recurrence of the disease. Patients must be closely monitored during these phases. Patient follow-up should be carried out by a specialized team in fully equipped clinics and sterile rooms.
Does acute leukemia recur?
Acute leukemia may recur in some cases. The disease is suppressed with high-dose chemotherapy given in the treatment of acute leukemia. However, leukemia can recur in a large proportion of patients in the high-risk group, usually within the first year. In order to prevent recurrence of leukemia, allogeneic bone marrow transplantation with stem cells is recommended. First, the patient’s siblings are evaluated and if they are compatible, their stem cells are transplanted. If no compatible siblings are found, bone marrow banks are consulted and a donor is sought. The aim of allogeneic stem cell transplantation is to reduce the risk of recurrence of the disease in the future. Today, compatible transplants are performed even if a fully compatible stem cell donor cannot be found. In addition, mini-transplants using low-dose drugs can be performed for elderly patients, giving them a chance for stem cell transplantation.
How is chronic leukemia (CLL treatment) managed?
It may not be necessary to start treatment immediately for every patient diagnosed with CLL. Because most CLL patients do not need treatment for many years. In the remaining part, the disease is progressive for a few years and treatment is needed. Important criteria when starting treatment are that the disease is progressive, shows various symptoms and has no organ involvement. Symptoms of the disease do not have a significant effect on treatment. Some special laboratory evaluations are used to determine the risk factors of the disease and individualized treatment is planned. The aim of chronic leukemia treatment is to suppress the disease and prevent it from harming the patient. Apart from chemotherapy, smart drugs are frequently preferred today as they target only cancer cells. Since smart drugs have little effect on healthy cells, they have fewer side effects than chemotherapy. Smart drugs are much more beneficial for CLL, which is more common in advanced age.
How is CML treated?
Breakthroughs in the treatment of CML, the second most common type of chronic leukemia, were made in the early 2000s. Leukemia in CML patients is caused by a genetic change in stem cells called the BCR/ABL mutation. Detection of this alteration has simplified the diagnosis of CML and led to the development of drugs against this defective system. In addition, the use of trozine kinase inhibitors (TKIs) has also been an effective treatment against the disease. Today, thanks to the use of oral TKIs, most CML patients can live close to their normal life expectancy.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
WHAT IS MULTIPLE MYELOMA?
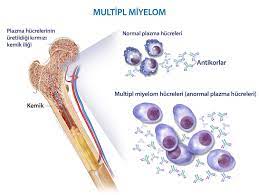
Multiple myeloma is a type of cancer that affects the plasma cells in the bone marrow that produce proteins that help the body fight infections. It is called multiple myeloma because the disease usually affects the areas around the spine, skull, pelvis, rib cage, shoulders and hips. Plasma cells are a type of white blood cell found in the bone marrow that produces blood cells. Healthy plasma cells produce antibodies to protect our bodies against diseases and infections. When an abnormal plasma cell in the bone marrow develops and multiplies rapidly, it causes multiple myeloma cancer. Like healthy blood cells, cancerous cells try to produce antibodies. However, they can only produce abnormal antibodies called monoclonal proteins or M proteins. When these harmful antibodies build up in the body, they can lead to kidney damage and other serious problems.
WHAT CAUSES MULTIPLE MYELOMA?
The exact cause of multiple myeloma cancer is not yet known. However, it is known that the cancer is caused by an abnormal plasma cell that multiplies much faster than it should in the bone marrow. Without a normal life cycle, myeloma cells continue to divide indefinitely. This can disrupt the production of healthy cells.
WHO GETS MULTIPLE MYELOMA?
The exact cause of multiple myeloma cancer is unknown. However, it is known who is at risk. Advancing age increases the risk of developing multiple myeloma. Multiple myeloma is usually seen in people over the age of 60, although it is rarely seen under the age of 35. Those at risk of multiple myeloma are
- Age: Multiple myeloma occurs mostly in people over the age of 60. Therefore, advancing age increases the risk of multiple myeloma.
- Race: The risk of multiple myeloma is higher in blacks than in other races. The reason for this difference between races is unknown.
- Men: Men have a higher risk of developing multiple myeloma cancer than women. It is not yet known why this disease is more common in men.
- History of monoclonal gammopathy of uncertain significance (MGUS): MGUS is a benign condition in which abnormal plasma cells produce M proteins. There are usually no symptoms and the abnormal M protein level is found by a blood test. Sometimes people with MGUS develop certain cancers, such as multiple myeloma. There is no cure, but people with MGUS have regular laboratory tests (every 1 or 2 years) to check for an increase in M protein levels. Regular examinations are also done to check for the development of symptoms.
- Family history of multiple myeloma: Multiple myeloma is not a genetic disease. However, studies have shown that people with a close relative with multiple myeloma have a higher risk of developing the disease.
WHAT ARE THE SYMPTOMS OF MULTIPLE MYELOMA?
Multiple myeloma can progress without any symptoms. Symptoms of the disease may vary according to the individual. Symptoms of multiple myeloma can be listed as follows:
- Bone pain( usually in the back and ribs)
- Bone fractures( usually in the spine)
- Feeling sluggish and very tired
- Feeling very thirsty
- Frequent infections
- Fire
- Appetite loss
- Weight loss
- Nausea
- Constipation
- Frequent urination
WHAT ARE THE STAGE SYMPTOMS OF MULTIPLE MYELOMA?
Patients with suspected multiple myeloma undergo various tests. The patient whose biopsy reveals multiple myeloma should make a treatment plan with his/her doctor. The degree of spread (stage) of the disease requires extra tests. The tests performed for the definitive diagnosis of multiple myeloma cancer are as follows:
- Blood tests : Blood tests such as albumin and beta-2-microglobulin are needed to determine the stages of multiple myeloma cancer.
- CT scan: Detailed pictures of the bones are taken with a computerized x-ray machine.
- MRI : A powerful magnet connected to a computer is used to create detailed pictures of your bones.
Doctors may describe multiple myeloma as asymptomatic, Stage I, Stage II or Stage III. Staging takes into account whether the cancer is causing problems with your bones or kidneys. Asymptomatic multiple myeloma is the early stage of the disease when there are no symptoms. For example, there is no bone damage. An early stage of the disease with symptoms (such as bone damage) is Stage I. Stages II or III are more advanced and there are more myeloma cells in the body.
HOW IS MULTIPLE MYELOMA DIAGNOSED?
Multiple myeloma can sometimes be diagnosed with a routine blood test. Doctors often suspect multiple myeloma after an x-ray taken for a bone fracture. Often patients go to the doctor because they have other symptoms. To find out whether such problems are caused by multiple myeloma or other conditions, your doctor will order the following tests after a family history and physical examination:
- Blood tests: Some blood tests are performed in the laboratory:
- Multiple myeloma causes high levels of proteins in the blood. A laboratory test checks the levels of many different proteins, including protein M and other immunoglobulins (antibodies), albumin and beta-2-microglobulin.
- Myeloma can also cause anemia, low levels of white blood cells and platelets. A complete blood count is done in the laboratory to measure the number of white blood cells, red blood cells and platelets.
- The laboratory also checks for high calcium levels.
- Creatinine is measured to check whether the kidneys are working well.
- Urine tests : Urine is tested for Bence Jones protein, a type of M protein. The amount of Bence Jones protein is measured in 24-hour urine. If your urine sample shows high levels of Bence Jones protein, your doctor will monitor your kidneys. Bence Jones protein can block the kidneys and cause damage.
- X-ray: X-rays may be taken to check for broken or thinned bones. You may have an X-ray of your whole body to see how many bones myeloma has damaged.
- Biopsy : Your doctor takes a tissue sample to look for cancer cells. A biopsy is the only sure way to know if myeloma cells are present in your bone marrow. Before the sample is taken, local anesthesia is used to numb the area. This helps to reduce pain. Your doctor will remove some bone marrow from your hip bone or another large bone. The pathologist uses a microscope to examine the tissue for myeloma cells.
- There are two ways your doctor can take bone marrow. Some people have both procedures in the same session:
- Bone marrow aspiration: The doctor uses a thick, hollow needle to take a sample of bone marrow.
- Bone marrow biopsy: The doctor uses a thicker, hollow needle to remove a small piece of bone and bone marrow.
WHAT ARE THE TREATMENT OPTIONS FOR MULTIPLE MYELOMA?
If you have multiple myeloma and do not experience any symptoms, your doctor will closely monitor whether the disease is progressing before initiating treatment. Regular blood and urine tests are performed to monitor the course of the disease and decide on the course of treatment.
There are treatments that can help relieve pain, reduce complications and slow the progression of the disease. These treatments are also used in case the disease progresses. The treatment options commonly used in the treatment of multiple myeloma are as follows:
Targeted therapy: With targeted therapy used in the treatment of multiple myeloma, drugs given to the patient intravenously or in pill form destroy proteins in myeloma cells and cause the cancer cells to die.
Chemotherapy: Chemotherapy, given intravenously or in pill form, is usually given in high doses before stem cell transplantation. Chemotherapy is an aggressive drug treatment that destroys myeloma and other fast-growing cells.
Corticosteroids: A type of treatment given in pill form or intravenously to reduce inflammation in the body, balance the immune system and treat myeloma cells.
Radiation therapy: Powerful radiation energy and beams are used to stop the growth, shrink and destroy myeloma cells.
Autologous bone marrow transplant: After the diseased bone marrow has been treated, stem cells are collected from the patient, then high-dose chemotherapy is given and the stem cells are returned to the patient. The stem cells can then be grafted into your body, where they are transported to the bones and begin to rebuild the bone marrow.
WHAT CAN BE DONE TO PREVENT MULTIPLE MYELOMA?
Since the exact cause of multiple myeloma cancer is unknown, the prevention of the disease is also unknown.
FREQUENTLY ASKED QUESTIONS ABOUT MULTIPLE MYELOMA
Can multiple myeloma be diagnosed early?
Multiple myeloma cancer can be diagnosed early today with advancing medical technology.
What is the risk of death from multiple myeloma?
As with any cancer, multiple myeloma has a high risk of death if left untreated.
How long does a multiple myeloma patient live?
Multiple myeloma patients can live longer thanks to newly developed chemotherapeutic drugs.
Is multiple myeloma a genetic disease?
People with a family history of multiple myeloma are more at risk of this disease. However, it is thought that this disease is not a genetic disease.
How should a patient with multiple myeloma eat?
Patients with multiple myeloma should make their nutrition programs under the control of the treating doctor. They should eat a protein-based diet as recommended by their doctor.
Is multiple myeloma cancer?
Myeloma, also known as multiple myeloma, is a bone marrow cancer caused by plasma cells.
Is there a herbal treatment for multiple myeloma?
There are scientific articles stating that ginger is good for multiple myeloma patients undergoing chemotherapy treatment.
Does multiple myeloma undergo chemotherapy?
As with other types of cancer, multiple myeloma cancer is treated with chemotherapy given intravenously or in pill form.
What are the chances of cure for multiple myeloma?
Successful results can be obtained from the treatment methods applied to prevent the progression of multiple myeloma cancer and the spread of the disease.
Is multiple myeloma bone marrow transplantation performed?
Multiple myeloma patients undergo autologous bone marrow transplantation.
What is life after multiple myeloma bone marrow transplantation?
Patients with multiple myeloma can return to normal life approximately 6 months after autologous bone marrow transplantation.
Is stem cell transplantation performed in multiple myeloma patients?
Autologous bone marrow transplantation is performed for multiple myeloma patients.
Does multiple myeloma metastasize?
Multiple myeloma metastasizes mostly to the bones.
Is multiple myeloma more common in men or women?
Multiple myeloma is more common in men than in women.
Can a woman with multiple myeloma become pregnant and is there a risk for her and the baby?
A woman with multiple myeloma can become pregnant. However, her disease must be under control and she must not be receiving chemotherapy.
Where is multiple myeloma most common in Turkey?
There is no statistical information showing how common multiple myeloma is in our country.
At what age is multiple myeloma most common?
Multiple myeloma is a rare type of cancer. It is usually seen in people over the age of 60, but it can also be seen rarely in people under the age of 35.
Is multiple myeloma a contagious disease?
Multiple myeloma is not a contagious disease.
Which doctor treats multiple myeloma?
Multiple myeloma patients are treated by hematology specialists.
Can multiple myeloma be prevented by taking vitamin D?
Multiple myeloma cannot be prevented by taking vitamin D.
Does multiple myeloma cause kidney failure?
Multiple myeloma can cause kidney failure in Stage III.
When are the results of multiple myeloma tests available?
There are many types of multiple myeloma tests. Therefore, it takes different times for each test to be finalized.
Can multiple myeloma be detected in blood and urine tests?
Multiple myeloma can sometimes be detected in a routine blood and urine test.
Is multiple myeloma a bone marrow cancer?
Multiple myeloma is a type of bone marrow cancer that is increasing in frequency.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.
What is a bone marrow transplant?

The cells responsible for blood production in the human organism are stem cells in the bone marrow. The transplantation of these cells with highly specialized functions is commonly referred to as ‘bone marrow transplantation’.
How is a bone marrow transplant performed?
The bone marrow produces blood cells. Stem cells are immature cells found in the bone marrow that make up all the different blood cells. Hematopoietic stem cells are used in transplants. The stem cells are transferred to the patient (recipient) through a vein. For this, an intravenous apparatus called a central venous catheter is usually used. After the transplant, the immature cells live in the bone marrow and differentiate into various mature blood cells, including
- Oxygen-carrying red blood cells
- Platelets that help blood clotting
- White blood cells that help fight infection
With a bone marrow transplant, damaged stem cells are replaced with healthy cells. This helps the body to make enough white blood cells, platelets or red blood cells to avoid infections, bleeding disorders or anemia.
There are different types of blood stem cell transplant. The type of transplant depends on the blood stem cell source.
- Bone marrow transplants (BMT) use blood stem cells collected from the bone marrow.
- Peripheral blood stem cell transplants (PBSCT) use blood stem cells collected from the bloodstream.
- Cord blood transplants (CBT) use blood stem cells collected from the placenta and umbilical cord of a newborn baby.
In which diseases is a bone marrow transplant performed?
A bone marrow transplant is performed when a patient’s marrow is not healthy enough to function properly. This can be due to chronic infections, various diseases or cancer treatments. Bone marrow transplants can benefit people with the following diseases:
- Acute leukemia
- Adrenolökodistrofi
- Aplastic anemia
- Bone marrow failure syndromes
- Chronic leukemia
- Hemoglobinopathies
- Hodgkin’s lymphoma
- Immune deficiencies
- Inborn errors of metabolism
- Multipl miyelom
- Myelodysplastic syndromes
- Neuroblastoma
- Non-Hodgkin lymphoma
- Plasma cell disorders
- POEMS syndrome
- Primary amyloidosis
- Treatment refractory or relapsed solid organ tumors
What are the cells produced in the bone marrow?
The donor can be discharged after being kept under observation for 24 hours after the collection procedure. The collected marrow is passed through special filters to remove fat and small bone fragments that may be mixed in. If it will not be used immediately, it is placed in special liquids and frozen. When it is to be used, it is thawed and given to the patient similar to a blood transfusion. These blood stem cells, which enter the patient’s body, settle in the bone marrow and usually start producing blood cells within 2-4 weeks.
What are the types of bone marrow?
There are two types of bone marrow transplantation (stem cell transplantation): autologous or allogeneic.
What is autologous stem cell transplantation?
The aim of autologous transplantation is to allow hematologic recovery after high-dose therapy. The cells are taken from the patient’s own bone marrow before chemotherapy and replaced after cancer treatment. So in some cases, cancer treatment involves high-dose, intensive chemotherapy or radiotherapy. In fact, cancer treatment can damage our stem cells and immune system. Before cancer treatment begins, doctors collect and freeze the person’s own stem cells for storage. After cancer treatment, these stored stem cells are returned to the person. This process is called stem cell rescue. Autologous stem cell transplantation is often used to treat diseases such as lymphoma, solid tumors in children and multiple myeloma in adults. In autologous stem cell transplantation, the risk of tissue rejection disease (GVHD), the possibility of the recipient rejecting the given stem cells, is very low. Autologous stem cell transplantation is therefore safer than allogeneic transplants.
What is allogeneic stem cell transplantation?
Allogeneic stem cell transplantation is the transplantation of stem cells from a sibling, relative or unrelated donor of the patient who will receive a stem cell transplant. Allogeneic transplants, unlike autologous transplants, create a new immune system response to fight cancer. In other words, immune system cells are transplanted along with the donor’s stem cells during the transplantation process. If the donor’s lymphocytes, which are transferred to the patient during allogeneic transplantation, perceive some of the cells in the patient as foreign, they start a war against them, which can cause ‘graft versus host’ disease, which causes severe damage to the recipient’s organs. To reduce the risk of allogeneic stem cell transplantation, immunosuppressive drugs are given to the patient immediately after transplantation to suppress the fighting capacity of the donor’s lymphocytes. After allogeneic stem cell transplantation, the patient and the donor should be as close to a tissue match as possible in order not to start a war due to tissue differences.
What are the risks of bone marrow transplantation?
After a bone marrow (stem cell) transplant, it can take a long time for the immune system to recover and start producing healthy new blood cells. Immune recovery after transplantation depends on many variables. For example, immune recovery may take up to five years depending on the stem cell source used, immunosuppressive interventions, various problems that develop, and cell subtypes that may recover at different times. Bone marrow transplant patients are at risk of infection during this period and should take precautions. In addition, the reduced number of blood cells can cause anemia, excessive bleeding, bruising and an increased risk of infection Some patients may require blood transfusions for some time.
What are the possible complications associated with bone marrow transplantation?
- Graft-versus-host disease (allogeneic transplant only)
- Stem cell (graft) failure
- Organ damage
- Infections
- Cataract
- Infertility
- New cancers
Graft versus host disease (GVHD): Graft versus host disease occurs in allogeneic transplants when transplanted cells begin to attack other cells in your body. It is a complex clinical syndrome with organ dysfunction as a result of a severe immunologic reaction mediated by healthy T-lymphocytes taken from the donor and given to the patient along with stem cells, and is considered the most important cause of mortality and morbidity after allogeneic stem cell transplantation (SCT). GVHD can occur immediately after transplantation or more than a year later.
There are two types of GVHD: acute and chronic. Acute GVHD usually occurs earlier in the first months after transplantation. It usually affects your skin, digestive system or liver. Chronic GVHD can cause severe damage to many organs.
Signs and symptoms of chronic GVHD include:
- Joint or muscle pain
- Shortness of breath
- Persistent cough
- Changes in vision
- Skin changes under the skin, including scarring or skin hardness
- Skin rashes
- Yellow color to your skin or the whites of your eyes (jaundice)
- Mouth sores
- Diarrhea
- Nausea, vomiting
What happens before a bone marrow transplant?
You will undergo a series of tests and procedures to assess your general health and condition and to make sure you are physically ready for the transplant. The evaluation may take a few days or longer. In addition, a surgeon or radiologist will insert a long thin tube (intravenous catheter) into a large vein in your chest or neck. The catheter, often called a central line, will in most cases stay in place for the duration of your treatment. Your transplant team will use the central line to infuse the transplanted stem cells, medicines and blood products into your body.
Frequently asked questions about bone marrow (stem cell) transplant
What is bone marrow transplantation in children?
Blood diseases and cancers are among the most life-threatening diseases in childhood. Success in the treatment of childhood blood diseases and pediatric bone marrow transplantation requires a fully equipped infrastructure and service quality. Established for this purpose, our Pediatric Bone Marrow Transplant Centers in Memorial Şişli, Bahçelievler and Ankara Hospitals serve our children with high-level diagnosis and treatment facilities. Bone marrow transplantation plays an important role in the treatment of thalassemia, aplastic anemias, immunodeficiencies, metabolic diseases, leukemias, lymphomas and some solid tumors in childhood. Our centers have an experienced physician-nurse-staff for bone marrow transplantation and specially designed services for this purpose.
In our Pediatric Stem Cell Transplant units, various measures are taken to prevent infections that may be transmitted to our pediatric patients from the external environment.
These measures are
- There is a special section at the entrance of each patient room, between the room and the corridor, where both transport personnel and companions are kept free from infections they may carry from outside.
- During the transplantation period, the food desired by the patients is prepared under special conditions.
- Hepafilter systems that remove airborne particles are used throughout the transplant unit to protect them from infections.
All types of bone marrow transplantation, including autologous, allogeneic (related and unrelated) and haploidentical, can be performed in the transplant unit for patients aged 0-18 years. It should be kept in mind that each patient is unique and the transplantation process should be carried out on this basis.
For which diseases is allogeneic stem cell transplantation most commonly performed in childhood?
In childhood, allogeneic transplantation is performed for malignant or non-malignant diseases that are mostly inherited. Among these diseases, the most frequently transplanted ones can be listed as follows
- Leukemias
- Myelodysplastic Syndrome
- Aplastic Mom
- Paroxysmal Nocturnal Hemoglobinuria
- Fanconi Aplastic Anemia
- Thalassemia
- Sickle Cell Anemia
- Severe Combined Immunodeficiencies
- Wiskott-Aldrich Sendromu
- Hemophagositik Lenfohistiositozis
- Kostmann’s Disease
- Chronic Granulomatous Disease
- Osteopetrosis
- Mucopolysaccharidosis
- Adrenolökodistrofi
- Metacromatik Lökodistrofi(MLD)
- Globoid hycre lökodistrofi(Krabbe)
- Wolman’s disease
- Mannosidosis
- Structural Aplastic Anemias; Dyskeratosis Congenita, Scwachman-Diamond Syndrome, Amegakaryocytic thrombocytopenia
- Diamond-Blackfan Anemia
These diseases are diagnosed by bone marrow aspiration and/or biopsy in addition to detailed history and physical examination.
For which diseases are autologous stem cell transplants most commonly performed in childhood?
The diseases for which autologous bone marrow transplantation is performed can be listed as follows
- Acute myeloid lösemia
- Non-Hodgkin’s lymphoma
- Hodgkin’s lymphoma
- Neuroblastoma
- Ewing sarcoma
- Medulloblastoma (brain tumors)
- Soft tissue tumors
- Germ cell tumors
- Wilm’s tumor (kidney tumor)
- Retinoblastoma (eye tumor)
- Some autoimmune diseases
When does the transplanted bone marrow start working?
After bone marrow (stem cell) transplantation, it usually takes 10-15 days for the stem cells to start producing blood cells again. During this time, the patient is given blood cell supplements from outside. This is because the bone marrow will need transfusions of red blood cells and platelets until the bone marrow starts to produce enough healthy cells on its own. Patients are required to come to follow-up visits where blood tests are done to assess the response to the graft. Patients may need to be followed up for many years after the transplant to avoid serious problems.
Is half-matched stem cell transplantation successful?
If donors cannot be found from fully matched siblings and bone marrow banks, the most important option today is semi-matched (haploidentical) transplants from relatives and cord blood. Transplants from half-matched relatives are an important treatment option that has increased in frequency worldwide in the last decade. Between 50% and 80% of the HLA genes of semi-conjugate related donors are compatible with the patient. While the probability of a sibling being half-conjugate is 50%, all children, mother and father of the patient are half-conjugate with the patient. It can take two to three months to find a donor from a bone marrow bank, then confirm the donor’s HLA at high resolution, and collect the stem cells. Patients with relapsed blood cancers may not have that much time to wait. In addition, obtaining stem cells from half-conjugate relatives does not take much time as they are easy to access. In case of relapse after allogeneic transplantation, the disease can be treated by giving the patient lymphocytes from the same donor, but this is not possible if cord blood is used. In the case of foreign transplants, it may take time to collect cells again. With quasi-matched transplants, it is very easy to collect cells again if the donor is still healthy. There was no significant difference in treatment outcomes between semi-matched and foreign fully matched transplants in patients with acute leukemia in China.
How are stem cells obtained from bone marrow?
Bone marrow is located in the spongy bone inside the bones. The most common location for bone marrow is in the pelvis (pelvic bone) of the human body. The collection of bone marrow from the donor is performed under general anesthesia and in a sterile environment.
How are stem cells obtained from peripheral blood?
Normally, the amount of stem cells in the blood circulating in the veins is small. For this reason, before the collection procedure, donors take medication to increase the amount of stem cells (G-CSF). These drugs are called growth factors. Peripheral stem cells are separated from the donor’s blood with special devices. The remaining blood, except for the separated stem cells, is returned to the donor. This process takes 4-6 hours. Depending on the amount of stem cells the patient needs, the procedure may need to be repeated several days in a row. In the case of autologous transplantation, the peripheral stem cell donor is the patient himself/herself. These blood stem cells enter the patient’s body and settle in the bone marrow. In this type of transplantation, engraftment starts earlier than in the bone marrow and takes place in a period of 10-20 days.
How are cord blood stem cells obtained?
Umbilical cord blood is collected from the umbilical cord or placenta after the baby is born. This blood is rich in blood-forming cells. The donated blood is tested for various aspects and stored for future use when needed. The storage units set up for this purpose are called “cord blood banks”. When needed, doctors contact these banks and look for a suitable tissue group match. If a suitable cord blood is found, the transplant is performed in a similar way to the others.
Who can receive a cord blood transplant?
Cord blood is mostly used for children because it contains a limited number of stem cells. In people with a high body weight, sometimes two or more cord bloods are combined for transplantation. The ideal stem cell source is one that is compatible in terms of tissue groups. However, in cord blood transplants, transplantation can be performed even if it is less compatible. Cord blood is stored and readily available, and cord blood is preferred if transplantation is urgently needed. The transplant team must decide which stem cell source is the most appropriate option.
How are stem cells collected for an autologous bone marrow transplant?
If a transplant using your own stem cells (autologous transplant) is planned, a procedure called apheresis (af-uh-REE-sis) will be used to collect blood stem cells. Before apheresis, you will receive daily injections of growth factor to increase stem cell production and move the stem cells into your circulating blood so they can be collected. During apheresis, blood is drawn from a vein and circulated through a machine. The machine separates your blood into different parts, including stem cells. These stem cells are collected and frozen for future use in the transplant procedure.
How are stem cells collected for allogeneic bone marrow transplantation?
Stem cells can come from your donor’s blood or bone marrow. Your transplant team will decide which is better for you based on your condition. They can also come from umbilical cord blood, which is taken from the placenta after birth and stored in special cord blood banks for future use. The blood from these cords is frozen and stored in a cord blood bank until it is needed for a bone marrow transplant.
Are there any risks to the health of the bone marrow donor?
Stem cell donation does not harm the donor’s health in any way. The donor is given a specific medication for 5 days to allow the stem cells to enter the bloodstream. When the number of stem cells in the blood reaches the desired level, they are taken from a vein in the arm like blood sampling.
Is there any age limit for bone marrow donors?
If the stem cell donor is a relative of the recipient, there is no age limit. However, people who want to donate stem cells to the tissue bank should be between the ages of 18-55.
Can stem cell therapy be used for joint pain?
Stem cell therapy is used in a different way in orthopedics. It can be applied in joints such as shoulder, hip, knee that have cartilage damage, painful joints but are in the early stage for surgical treatment or in patients who do not want to undergo surgery. However, stem cell therapy is not applied as a treatment option for almost complete loss of joint cartilage capacity.
Is it OK to exercise after a bone marrow transplant?
If the bone marrow transplantation process is completed successfully, you can start exercising. The intensity of exercise should be increased gradually and you should not over-exert yourself all at once. Your doctor will help you create an exercise plan tailored to your needs and requirements.
What is bone marrow for?
Bone marrow produces blood cells. Stem cells are immature cells found in the bone marrow that make up all the different blood cells.
What happens if the bone marrow does not work?
If the bone marrow does not work due to any disease, it causes deficiencies in vital blood production.
Why is a bone marrow test done?
A bone marrow test is performed to determine the type, quantity and maturation levels of blood cells, the structure of the bone marrow and to identify existing diseases.
Does the bone marrow renew itself?
Bone marrow, i.e. stem cells, has the ability to constantly renew itself.
How many days does the bone marrow result take?
The most common location for bone marrow is the pelvis (pelvic bone) of the human body. The collection of the bone marrow required for transplantation from the donor is performed under general anesthesia and in a sterile environment. The donor can be discharged after being kept under observation for 24 hours after the collection. Special needles are used to collect the marrow. These needles allow the marrow with a dense consistency to be extracted.
Is there pain during bone marrow harvesting?
Bone marrow is performed under general anesthesia and in a sterile environment. Special needles are used to collect the marrow. These needles allow the marrow with a dense consistency to be extracted. The donor does not feel any pain.
Is bone marrow cancer leukemia?
Leukemia is commonly known as bone marrow cancer or blood cancer.
*Page content is for informational purposes only. Please consult your doctor for diagnosis and treatment.

